Epilepsy Syndromes – Neurology Rite Review – Flashcards
Unlock all answers in this set
Unlock answersquestion
Benign Idiopathic Neonatal Seizures
answer
Typically occurs around fifth day of life "Fifth day fits" Neurologically normal infant, no family history Partial clonic seizures can progress to status epilepticus No EEG findings specific for the diagnosis GOOD PROGNOSIS - Resolves in approximately 24 hours, normal development, not at increased risk of seizures as adults.
question
Benign Familial Neonatal Seizures
answer
Begins in the first few weeks of life Focal, multifocal, or generalized seizures + Family Hx of similar neonatal seizures Autosomal dominant *(KCNQ2 and KCNQ3)* No EEG findings specific to the diagnosis GOOD PROGNOSIS - In most cases seizures resolve during infancy, normal development. However, 15% will have seizures in adulthood.
question
Early Infantile Epileptic Encephalopathy (EIEE) Ohtahara Syndrome
answer
Onset: starting age 1 day to 3 months sx: Tonic seizures, possible infantile spasms. Severe developmental delay. EEG: Ictally with tonic sz, there is a high-voltage slow wave followed by fast activity. Interictally there is a *burst suppression* pattern. Treatment: Standard AEDs. Ketogenic diet Prognosis: Poor, 50% die during infancy. Others can progress to West syndrome or LGS.
question
Dravet Syndrome
answer
Severe myoclonic epilepsy of infancy due to sodium channel mutation *(SCN1A)* with developmental delay and neurologic abnormalities. Febrile seizures start first year of life followed by other seizure types (myoclonic, atypical absence, GTC. Tx: VPA, topiramate, zonisamide and ketogenic diet. Avoid: Phenobarbital, phenytoin, carbamazepine and lamotrigine
question
Glut1 Deficiency Syndrome
answer
AD, SLC2A1mutation in glucose transporter protein type 1 sx: seizures begin around first month tx: ketogenic diet
question
West Syndrome
answer
Onset: 4-7 months Triad: 1. Infantile spasm 2. hypsarrythmia 3. developmental arrest Multiple etiologies: hypoxic-ischemic, brain malformations, structural abnormalities, congenital or acquired infections, chromosomal abnormalities, inborn errors of metabolism, cryptogenic in 30% Think tuberous sclerosis (TS) and get MRI px: poor, can progress to LGS tx: ACTH (corticotropin) or high dose prednisone. If d/t TS treat with vigabatrin
question
hypsarrythmia
answer
High voltage, disorganized, slow, multifocal epileptiform discharges (during nonREM sleep)
question
Sandifer syndrome
answer
NOT a seizure. Spastic torticollis or dystonic movement associated with reflux
question
Febrile seizures (incidence, risk factors, likelihood to develop into epilepsy, treatment)
answer
3-5% of children age 6 months to 5 years 30% have second seizure Risk factors for 1st FS: family history of FS, prolonged neonatal ICU stay, developmental delay, day care Tx: supportive for one or more simple febrile seizure, may consider prophylaxis with diazepam, antipyretics (short-term) phenobarbital or VPA (long-term) if recurrent, prolonged, afebrile, complex, developmental delay
question
Distinguish simple and complex febrile seizures
answer
Complicated if: 1. Recur within 24h 2. Prolonged (>15min) 3. Focal >15 min, focal features, abnormal exam, seizure recurrence in <24 hours, post-ictal signs (Todd's), more likely due to meningitis, encephalitis or underlying seizure disorder simple: 1. <15 min, 2. generalized, 3. no focality, 4, nl. exam, 5. no persistent deficits
question
What to tell parents with kids who had febrile seizures?
answer
Parents should be reassured after a simple febrile seizure that there is no negative impact on intellect or behavior, and no increased risk of death. Routine laboratory tests, electroencephalography, and neuroimaging are not recommended in patients with simple febrile seizures. Use of long-term continuous or intermittent antiepileptic medication after a first simple febrile seizure is not recommended because of potential adverse effects. Use of antipyretic agents at the onset of fever is not effective at reducing simple febrile seizure recurrence.
question
Generalized epilepsy with febrile seizures plus (GEFS+)
answer
AD, has been linked to multiple genes including *SCN1A* (possible link to Dravet's?) Onset: Around 2 y.o. (but can range from 4mos-10yrs) Clinical Presentation: Afebrile and febrile seizures that continue beyond age 5. Afebrile sz types can include GTC, CPS, absence, myoclonic EEG with polyspikes or generalized spike-wave. No disease specific findings tx: Valproate Prognosis: Good in most children with resolution of seizures around 11 years of age. However, about 30% will have more severe epilepsy.
question
Rassmussen's Syndrome (Etiology, clinical presentation, Tx)
answer
Rare, severe, inflammatory brain disorder Progressive unilateral hemispheric atrophy, progressive hemiparesis and cognitive decline, intractable focal seizures Antibodies to *glutamate receptor 3* Consider hemispherectomy
question
Progressive myoclonic epilepsies
answer
Lysosomal storage disorders or mitochondrial disorders Tx: VPA (avoid if mitochondrial mutation due to liver failure), clonazepam, levetiracetam, topiramate, zonisamide, lamotrigine
question
Lafora body disease (What type of disease, what are Lafora bodies, where are they found, how is it diagnosed and treated)
answer
AR, Mutation of *EPM2A* gene on Chr 6q24 (encodes laforin) Age 12-17 years Dysarthria, ataxia, emotional disturbance, dementia, multiple seizure types, death within decade. Fatal Dx: PAS positive Lafora bodies w/in apocrine sweat gland or DNA sequencing. inclusion bodies, (AKA Lafora bodies) in cytoplasm of cells composed of abnormal glycogen called polyglucosans. Found in heart, liver, muscle, and skin, Tx: Zonisamide and other AEDs.
question
Unverricht Lundborg Syndrome (Baltic myoclonic epilepsy)
answer
AR, *EPM1* gene that encodes for cystatin B (CSTB) on chrome 21q22 mcc of the progressive myoclonus epilepsies. Onset ages of 6 and 16. Onset with myoclonic jerks and tonic-clonic sz , later various sz types, ataxia, tremor, cognitive decline. Often in wheelchair and death before the age of 24. EEG: 3-5 Hz spike-and-wave or multiple spike and wave activity; marked photosensitivity tx: Valproic acid (1st line) Levetiracetam, Clonazepam, topiramate, and zonisamide. avoid: Phenytoin (worsens szs & neurodegen) carbamazepine
question
Neuronal ceroid lipofuscinosis (NCL)
answer
Lysosomal storage disease, generally *AR* disorders Accumulation of autofluorescent lipopigments resembling ceroid and lipofuscin. Made up of fats and proteins and build up in neurons, liver, spleen, myocardium, and kidneys. Variable onset, yet progressive, sx, including *sz, dementia, visual loss, and/or cerebral atrophy* 4 types 1. Early infantile variant (INCL or Santavuori-Haltia): nL birth, early visual loss --> complete retinal blindness by 2 yrs, vegetative state by 3 yrs, death at 4. 2. Late infantile variant: 2-4 years get sz and deterioration of vision. Death 10-12 yrs. 3. Juvenile NCL (JNCL, Batten Disease, or Spielmeyer-Vogt): ~4-10 yrs get vision loss d/t retinal dystrophy, with sz, psychological degeneration, and eventual death 20s or 30s. 4. Adult variant NCL (ANCL or Kuf's Disease): milder sx ~30 yrs, death ~10 years later.
question
Myocolonic epilepsy with ragged red fibers (MERRF)
answer
Seizures, myoclonus, ataxia, myopathy. maternally-inherited point mutation at position *8344 in the mt genome disrupts gene for tRNA-Lys and synthesis of proteins essential for oxidative phosphorylation (in 80%) "Ragged Red Fibers" - clumps of diseased mt accumulate in the subsarcolemmal region of the muscle fiber and appear as "Ragged Red Fibers" when stained with modified Gömöri trichrome sx: progressive myoclonic epilepsy, short stature, ataxia, hearing loss, lactic acidosis, exercise intol, poor night vision tx: symptomatic, High doses of Coenzyme Q10 and L-Carnitine
question
Progressive myoclonic epilepsy (Sialidosis)
answer
AR deficiency of lysosomal enzymes, can be demonstrated in leukocytes and cultured fibroblasts, also high urinary sialyloligasaccharides Type 1: Deficiency of alpha-neuraminidase, action myoclonus, slowly progressive ataxia, vision loss and GTC in adolescents/adults, no mental decline or dysmorphism, positive CHERYY RED SPOT Type 2: Deficiency of N-acetyl neuraminidase and beta-galactosidase, myoclonus, coarse facial features, corneal clouding, hepatomegaly, skeletal dyplasia, learning disabilities, starts in neonatal period to second decade of life
question
Absence seizures
answer
Peak age 6, more often in girls, usually normal neuro exam Multiple daily spells for a few seconds, begin and end abruptly, mild jerks of eyelids, eyes, eyebrows at onset, then blank stare, automatisms like lip smacking, nose rubbing, picking at clothes, provoked by hypoglycemia and hyperventilation. Thalamus implicated with low-threshold *T-type calcium channels* Tx: Ethosusximide (inhibits calcium channels), also may use VPA, lamotrigine, topiramate and zonisamide) AEDs can be discontinued in adolescence if seizure free 1-2 yrs and normal EEG, overall good prognosis, remissions in 90% Avoid: Lamotrigine, gabaergic drugs (activate calcium channels)
question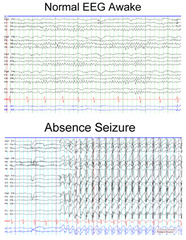
absence seizures EEG
answer
3 Herz spike and wave
question
Lennox-Gastaut Syndrome
answer
Onset: 2-8 years Triad of seizures of multiple types -tonic, atonic, atypical absence, myoclonic. 1/3 have h/o infantile spasms. - a/w MR. 50% nL cognitively before sz's, but all show severe psychomotor retardation after onset of disease EEG: Interictal <2.5 Hz bilateral slow spike-wave complexes tx: VPA, lamotrigine, topiramate. ketongenic diet. Often refractory, can consider rufinamide or felbamate in those cases
question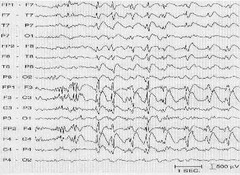
Lennox-Gastaut EEG
answer
Interictal <2.5 Hz bilateral slow spike-wave complexes
question
Myoclonic Astatic Epilepsy Doose Syndrome
answer
Onset: Preschool age (peak onset age of 2-6 yrs) sx: Previously nL child develops multiple sz types (GTC, absence, myoclonic, atonic astatic, myoclonic astatic) Usually characterized by difficult to control and possibly several seizures daily. EEG: Interictal 2-3Hz spike-and-wave discharges tx: VPA, Ethusoximide, keppra, benzos. May use LTG for GTCs. ketogenic diet can be the most effective treatment. Avoid: CBZ, vigabatrin Prognosis: VARIABLE - Some resolve completely and others develop intractable epilepsy with impaired cognition.
question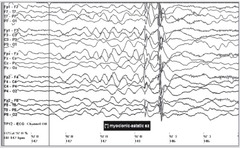
Myoclonic Astatic Epilepsy EEG (Doose s/d)
answer
Interictal 2-3Hz spike-and-wave discharges seen in
question
Landau-Kleffner Syndrome
answer
Acquired epileptic aphasia Onset 3-7 y/o Acquired auditory agnosia, Word deafness in the setting of normal hearing, receptive and expressive aphasia, EEG: Centrotemporal sharp waves that increase in sleep, Electrical status epilepticus in slow sleep (ESES) VPA and lamotrigine are usually effective for seizures, but speech recovery can be variable
question
Electrical status epilepticus during slow-wave sleep (ESES)
answer
Age 1-12 years, peak 4-5 Psychomotor retardation, multiple seizures during sleep Linked to Landau-Kleffner, but ESES has more global regression and more refractory to TH
question
Pyknolepsy
answer
Childhood absence in kids around 3-4 EEG: bilateral, synchronous, symmetric 3-Hz spike-and-wave discharge No distinct clinical or EEG features completely differentiate childhood absence epilepsy from juvenile absence epilepsy.
question
Early Onset Idiopathic Occipital Epilepsy (Panayiotopoulos Syndrome)
answer
Onset 4-8 years sx: Tonic eye deviation, *vomiting,* autonomic sx, visual auras, *GTC in sleep* EEG: occicpital spikes in 1-3 Hz bursts when eye closure Treatment not required, resolves in a few years
question
Juvenile myoclonic epilepsy (JME)
answer
Idiopathic generalized epilepsy with adolescent onset. nL development, no gender preference sx: morning myoclonic jerks, tonic-clonic seizures, and possible absence seizures. Intellectually normal. EEG: generalized 4-6Hz polyspike and wave, triggered by photic stim Tx: VPA, also lamotrigine, levetiracetam, topiramate and zonsisamide, required lifelong Avoid: alcohol and sleep deprivation Contraindicated: Carbamazepine and phenytoin, and gabapentin
question
Juvenile myoclonic epilepsy EEG
answer
generalized 4-6Hz polyspike and wave, triggered by photic stim
question
Benign childhood epilepsy with centrotemporal spikes (Rolandic epilepsy)
answer
Common (25% of childhood epilepsy), Onset: Typically begins bw 5-9 y/o, resolves mid-teenage years. Hemifacial sensorimotor sz with spread to i/L hand; progression to hemiconvulsion or GTC c in 50%, 70% only in sleep, 15% only awake. nL development and exam, nL imaging EEG: centrotermporal spikes on normal background activated by drowsiness and sleep Genetics: AD with variable penetrance; Possibly linked to 15q14; Tx: Most do not require AED. Carbamazepine (use only when prolonged or frequent seizures, wait for >2 before starting), stop after adolescence Prognosis: Excellent; most resolve before age 16 years. (only 5% continue to seize > 5 years of onset)
question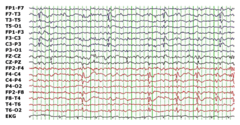
Rolandic epilepsy EEG
answer
centrotermporal spikes on normal background activated by drowsiness and sleep
question
Autosomal dominant nocturnal frontal lobe epilepsy (ADNFLE)
answer
Begin in childhood and persist into adult life, mutations of the *nicotinic acetylcholine receptors* CNRNA4 (chrome 20) and CHRNB2 (chrome 1) Bizarre episodic behaviors in the context of hypermotor seizures (thrashing, jerking) Onset during non-REM sleep, patients awaken with motor manifestations, patients will be conscious and report epigastic or other aura Often misdiagnosed as pseudo seizure because of unusual appearance and normal EEG interictally Usually responds to carbamazepine
question
Temporal lobe epilepsy (clinical presentation)
answer
mc type of partial epilepsy Auras include viscerosensory, gustatory, olfactory, auditory, fear oral/hand Automatisms, altered consciousness, deja vu, complex partial seizures, olfactory hallucinations mesial temporal sclerosis
question
Frontal Lobe Epilepsy
answer
Second most common type of focal epilepsy Semiology can be bizarre - hypermotor behavior (e.g. bicycling), may also have vocalizations Brief (typically <30sec), can be clustered, often no post-ictal confusion
question
Lateralizing signs in seizures
answer
Eye deviation: contralateral frontal lobe Extended arm: contralateral supplementary moror area Dystonic arm: contralateral temporal lobe Gelastic: hypothalamus
question
HSV encephalitis EEG
answer
PLEDs (periodic lateralizing epileptiform discharges)
question
CJD EEG
answer
Generalized periodic epileptiform discharges
question
Subacute sclerosing panencephalitis (SSPE)
answer
Generalized periodic epileptiform discharges, but typically longer interval of 4-15 sec
question
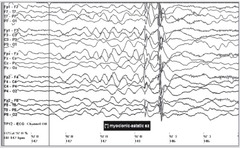
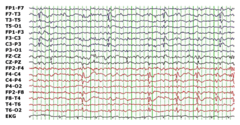
Infantile Spasms
answer
breach rhythm
question
Need pictures
answer
pleds CJD SSPE HSV



