NUR 120 (UNIT 4) CAD, CABG and CHF 5.1- 6.1 – Flashcards
Unlock all answers in this set
Unlock answersquestion
Coronary Artery Disease is:
answer
an umbrella disorder that includes: - athereosclerosis - angina pectoris - acute coronary sndrome (can lead to MI if not resolved) - myocardial infarction - heart failure - pulmonary edema
question
atherosclerosis is:
answer
abnormal accumulation of fat in the arteries and arteries walls lipid deposit and fibrous tissue build up in the wall which leads to plaques which cause a decrease in blood flow
question
atherosclerosis is significant because:
answer
it is the most common caused of CAD
question
atherosclerosis pathophysiology
answer
foam cells (macrophages that have become distended with lipid) begin to form fatty streaks, - fatty streaks build up to become ?brous atheromatous plaque - these lead to damage to artery walls which causes an inflammatory response in the artery - ?brous atheromatous plaque build up to become complicated plaques - the inflamm response then leads to plaque build up - the plaque build up slows blood flow - the plaque can dislodge and becomes an emboli and may move to the brain or lung and cause stroke or death
question
Atherosclerosis clinical manifestations
answer
- Acute Coronary Syndrome - coronary ischemia - coronary infarction
question
Angina and Coronary Artery Disease
answer
- clinical syndrome with episodes of pressure and pain in the chest as a result of lack of O2 in the heart muscles due to insufficient blood flow to the myocardial tissues - angina is progressive
question
How does activity effect Angina?
answer
- it increases metabolic demands and O2 requirements which leads to exacerbation and angina caused by atherosclerotic disease
question
What may lead to an exacerbation of angina?
answer
- significant obstrucution of major coronary artery - high BP (increases O2 demand) - cold weather (causes vasoconstriction) - heavy dinner: blood shunt to the GI and increase in O2 demand, decrease peristalsis
question
Coronary Arteries and Angina
answer
- right coronary artery becomes --> posterior descending artery - left main coronary artery becomes --> circumflex and anterior descending arteries - coronary arteries are filled during diastole - if the coronary arteries are clogged and blood perfusion is decreased (along with diminished O2 supply) ischemia occurs and angina pain presents
question
clinical management and tx of angina
answer
- decrease their O2 demand - REST (supine position) - increase their O2 supply - NTG (sublingual, 3 doses every 5 mins, no more then go to ER) - PCI/CABG - Surgery to reduce plaque formation **rest will resolve early angina, usually**
question
pharmacological tx of angina
answer
- usually done in hospital - O2 administration (increases O2 sat) - Nitroglycerin admin (dilates coronary arteries and increases blood/O2) - Beta Blocker admin (decreases sympathetic stimulation of the heart) - Ca+ Channel Blocker admin (dilates blood vessels) - Antiplatelet/anticoag admin (ASA) (thins blood/reduces viscosity)
question
Nursing Interventions for a pt with Angina
answer
- start with assessment of pain (usu COLD AAA acronym) - tx and prevent pain - reduce anxiety - teach self care
question
Myocardial Infarction and CAD
answer
the left anterior descending (LAD) coronary artery is blocked with a blood clot causing damage to the heart muscle and reads with an irregular ECG/EKG
question
MI's may also be called
answer
- Acute Coronary Syndrome - Heart Attack - coronary infarction
question
MI pathophysiology
answer
- the coronary vessel is clogged by plaque and clotting factors - the part of the muscle distal to blockage doesnt get blood or O2 - then the BP raises (sympathetic/parasym kicks in) increasing O2 demand - heart rate and respiratory rate increases - causes anaerobic environment which is ischemia - ischemia causes pain - no blood and no O2 causes infarction and necrosis of the tissue **not all MI are the same** **ask how bad was it?**
question
Where do MI's mostly occur?
answer
- anterior, inferior, lateral aspects of the heart --> right ventricle (ventricles) **ask where was the MI occurred**
question
Typical causes of MI
answer
- vasoconstriction that is persistent - plaque - clot
question
MI Chest pain is described as:
answer
Severe, crushing, constrictive, heavy pain **does not go away with rest or NTG**
question
SNS Response during MI
answer
- GI distress, nausea, vomiting - Tachycardia (HR increases) and peripheral blood vessels will vasoconstrict (shunts blood to the heart) - Anxiety, restlessness (may be caused by hypoxia)
question
MI may lead to:
answer
- following the SNS response, hypotension and possibly shock - if not treated can lead to cardiac arrest **the SNS response is a compensatory state and hypotension is a decompensatory state**
question
MI Hx and Phys findings
answer
- take VS - take ekg (tells where, if and how bad MI is) - get CK, ISO and troponins from blood (these help to dx.) - do phys exam and take hx
question
MI pt Tx goals
answer
- promote tissue perfussion (give O2 to treat hypoxia, ntg, ASA, beta blocker admin, thrombolytic therapy: clot busting tx = all of these are to reduce the size of the infarction) - relieve pain - reduce anxiety - prevent complications
question
What are some complications of an MI
answer
- dysrhythmias (like complete heart block, tachy, brady) - cardiogenic shock - acute pulmonary embolism (potential) - cardiac failure - thrombo-embolytic episodes
question
Nursing Responsibility for pt with MI
answer
- assessment dx (head to toe for cardiac signs) - Planning: tx and prevent pain - reduce anxiety - teach self care - probably in CCU **when writing pathophys of MI you had better mention how the inflamm process, edema, WBC, etc are involved**
question
Acute MI Medical Treatment
answer
- Drugs - Percutaneous Coronary Intervention (PCI) - Coronary Artery Bypass Graft (CABG)
question
Acute MI Thombolytic Tx:
answer
- if patient is Dx by symptoms and EKG, begin this therapy. - ideally begins within 3-6 hrs of infarction. - must get informed consent from pt. - contraindicated in pt with bleeding abnormalities or recent surgery. - tx is systemic, usu pressure dressings, sml needles, hold pressure (5-10mins) when inserting IV.
question
Thrombolytic Tx is used to
answer
- increase blood flow - decrease size of infarction - cause re-perfusion **thrombolytic tx is called door to needle time. once throm tx occurs the patient must have access to PCI usu at cath lab.**
question
Nursing Care for Pts with MI's
answer
- ongoing assessment - dx - planning: (independent interventions and dependent interventions and collaborative interventions)
question
Immediate tx of an MI
answer
M- orphine O- O2 (standing orders) N- NTG A- ASA **must watch respiratory rate, heart rate, LOC, etc** **MONA** **dependent and collaborative interventions**
question
Invasive Med Interventions for MI
answer
- Percutaneous Transluminal Coronary Angioplasty (PTCA) - Coronary artery stent - CABG - Heart Transplant
question
PTCA: Percutaneous Transluminal Coronary Angioplasty
answer
- used for pts who have had acute MI, helps reperfuse, - can use for angina and recurrent chest pains - done in cath lab - use angiography to locate of plaque - surgeon uses fem artery and inserts balloon cath - uses flouroscopy to place - balloon inflates to compress plaque against wall - insert stents to hold wall lumen open. - can have angioplasty without stent placement
question
PTCA Nursing Considerations
answer
- may cause coronary artery rupture - may cause emboli from dislodged plaque to move to the brain - may cause bleeding - may cause hematoma formation - do 5 P assessment - with CABG you need to worry about clot, shock, impaired tissue perfusion - keep leg straight and secure (sandbag, restraints)
question
Coronary Artery Stinting Pts Teaching
answer
- not permanent solution - must have lifestyle change to prolong lifetime of stent - stent is coated with anticoag drugs to prevent coag - risk of thrombus with stint - wire mesh
question
Percutaneous Coronary Intervention (PCI)
answer
an invasive procedure in which a catheter is placed in a coronary artery, and one of several methods is employed to remove or reduce a blockage within the artery
question
Complications of PCI's
answer
- dissection - perforation - abrupt closure - or vasospasm of the coronary artery - acute MI - acute dysrhythmias (eg, ventricular tachycardia), and cardiac arrest.
question
Post operative Complications of PCI's
answer
- abrupt closure of the coronary artery - bleeding at the insertion site - retroperitoneal bleeding - hematoma - arterial occlusion - acute renal failure
question
Periprocedure care for Pt's receiving PCI
answer
- Patients who are not already hospitalized are admitted the day of the PCI. - Those with no complications go home the next day. - During the PCI, patients receive IV heparin or a thrombin inhibitor - are monitored closely for signs of bleeding - pt may receive medication tx for several hours following the PCI to prevent platelet aggregation and thrombus formation in the coronary artery. - sheaths where PCI was inserted will be replaced after blood studies confirm that heparin is inactive and clotting times are normal - The patient must remain ?at in bed and keep the affected leg straight until the sheaths are removed and then for a few hours afterward to maintain hemostasis. - Because immobility and bed rest may cause discomfort, treatment may include analgesics and sedation. - Sheath removal and the application of pressure on the vessel insertion site may cause the heart rate to slow and the blood pressure to decrease (vasovagal response). - An IV bolus of atropine is usually given to treat this response - a pressure dressing is applied to the site
question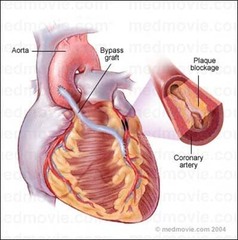
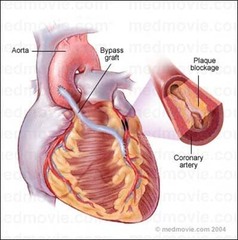
Coronary Artery Bypass Graft (CABG) (diagram)
answer
- A.K.A Coronary Artery Revascularization
question
CABG uses:
answer
- can be used to prevent MI - viable option pts with CAD - variant angina (prinzmetal angina) happens at rest - unstable angina - positive exercise stress test - pts not responding to NTG - pts that have blockages that arent treatable by angioplasty
question
CABG Nursing Considerations
answer
- need to preped for OR: clean skin, prep for gen anesthesia - will use coronary artery bypass machine due to stopping heart - blood vessels taken from another part of body and used for the heart (leg, mammary artery) - pts will be on heparin - anticoagulated - will be hypothermic 82-89 degrees (slow body processes like metabolic rate to reduce O2 demand) - not permanent
question
Complications of CABG
answer
- potential for death - when veins are used they don't last as long, not as muscular, not as many layers as arteries, will fail due to arterial pressure - possible infection r/t long incision - possible edema from removal of vein in leg
question
What veins are commonly used for CABG?
answer
- greater and lesser saphenous veins - mammary artery
question
CABG preop care
answer
- preop teaching: IV meds - PCA - morphine, inc spiro, cough and deep breathe, splinting incision, - phys and psych assessment - pts who are less anxious do better postop - health hx - informed consent - nursing process
question
Nursing Dx for CABG
answer
- impaired tissue perfusion - pain - risk for infection - impaired gas exchange r/t ineffective airway clearance - altered breathing pattern - anxiety - decreased cardiac output - activity intolerance - risk for injury
question
CABG intraoperative care:
answer
- Holding: Assess, prepare for OR ; PACU - IV lines are inserted - Anesthesia --> ETT --> Mechanical Ventilator - Periop RN: Assist with procedure and Ensure pt comfort and safety
question
CABG Postoperative care
answer
- Hemodynamic stability (assess for pressures in and around the heart) - Recover from general anesthesia - Wound care (slow healing, dehiscence) - Fluid and Electrolytes - Progressive activity - Diet - D/C home in 3-5 days
question
CABG Complications
answer
- MI - Dysrhythmias - Hemorrhage - Stroke - Infection
question
"Congestive" Heart Failure is
answer
** r/t Inadequate Tissue Perfusion** - Evaluate cardiac, pulmonary and systemic congestion - when you have heart failure the heart is not able to provide sufficient O2 to meet tissue needs which results in inadequate tissue perfusion - is contributed to by coronary artery disease - can be acute or chronic (insidious-gradually occurring and moves from stage A to B to C to D) - can be left or right sided - A form of cardiac failure - A syndrome - not a disease
question
CHF is usually a:
answer
lifelong issue (chronic) some symptoms may be able to be resolved.
question
CHF Pathophysiology:
answer
- systolic or diastolic overloading ; myocardial weakness --> - then as this physiological stress reaches critical level, contractility is reduced (pain is a late symptom) --> - Cardiac Output declines --> - Venous input to ventricles remains the same
question
CHF Acute vs Chronic Patho
answer
- Acute - short term response (Ventricular muscle dilatation and increased force of contraction) - Chronic - ventricular hypertrophy
question
CHF Etiology
answer
- damage to the heart muscle (affects afterload) - ventricular overload rt increased *preload*: 2° MI, IV fluid volume overload ; kidney failure --> increased venous return - ventricular overload rt increased *aferload*: 2° uncontrolled chronic HTN, valve problems - constriction of the ventricles: r/t cardiac temponade
question
Cardiac Reserve is:
answer
- the ability of the heart to compensate under stress
question
Cardiac reserve is affected by:
answer
- increased sympathetic activity (fight or flight) - Na and water retention (ALD, RAAS can increase preload) - anaerobic metabolism of affected cells - increased uptake of O2 by peripheral cells **when these fail or overwork, cardiac reserve is affected negatively**
question
CHF Compensatory Mechanisms include:
answer
- Tachycardia - Ventricular dilation - Cardiac Hypertrophy - Changes in Vasculature, Kidneys, and Liver
question
Left Sided Heart Failure (memory)
answer
- notice he is in tripod position to facilitate breathing
question
Left Sided Heart Failure
answer
- decreased cardiac output and pulmonary congestion - from decreased Cardiac Output you see activity intolerance and signs of decreased tissue perfusion. - if left ventricle is congested --> blood backs up into the pulmonary vein --> then into the lungs --> then into the pulmonary artery causing pulmonary congestion - from pulmonary congestion you can have impaired gas exchange (alveoli and caps) which means the blood that moves through will have *less O2* which causes *decreased tissue perfusion* - decreased tissue perfusion leads to cyanosis and signs of hypoxia. - because of congestion in the lungs, capillary pressure in the lungs begins to change - protein rich fluids begin to seep out of the caps into the alveoli which presents as *crackles* --> which leads to pulmonary edema - pulmonary edema can show as a cough with frothy sputum (can be pinkish due to blood) - orthopnea (pop up in bed to breathe) - paroxysmal nocturnal dyspnea - dont worry about elevated pulmonary capillary wedge pressure **most of these symptoms are heart and lung related --> symptoms close to the heart**
question
With left ventricular failure there is
answer
- a stroke volume problem - compromised stroke volume and decreased cardiac output
question
Right Sided Heart Failure
answer
- congestion is in the right ventricle - blood will back up into the right atria --> & then the superior and inferior vena cava --> which leads to congestion of peripheral tissue --> which leads to dependent edema and ascites (r/t portal HTN) and JVD - can cause liver congestion - from liver congestion may see signs r/t to impaired liver funx - can caused GI tract congestion - from GI you may see anorexia, GI disress and weight loss **Most of these symptoms extend to more peripheral systems --> away from heart and lungs**
question
What is Systolic Heart failure?
answer
- the most common type - is when there is *alteration in ventricular contraction* remember *systolic* = *contraction*
question
What is diastolic heart failure?
answer
- is char by stiff and non compliant heart muscle - wont relax enough to fill correctly - *doesnt relax and fill properly* (Preload problem in ventricle) remember *diastolic* = *relax*
question
What is Ejection Fraction?
answer
- % of blood volume in the ventricle at end of diastole that is ejected during systole - measure of contractility - an indicator of severity of CHF **% of blood volume in the ventricles that can be squeezed from the ventricles at the end of systole.**
question
What is normal ejection fraction
answer
- we want it to be greater than 55%
question
CHF signs and symptoms:
answer
- fatigue and tiredness - hypertrophy (XRAY) - lower ejection fraction (ECHO) - SOB
question
CHF Dx studies
answer
**help evaluate cardiac, pulmonary and systemic congestion** - CXR - Echocardiogram: shows = ejection fraction which is an indicator for severity of disease - pulse ox (not diagnostic but indicator) - hemodynamic monitoring
question
Lab Tests for CHF
answer
- BNP - shows LVH (normals are 100 and under-usually) - CK-MB - shows cardiac muscle stress
question
Stage A of Heart Failure
answer
- Stage A Patients at high risk for developing left ventricular dysfunction but without structural heart disease or symptoms of heart failure - pts can usu have pretty normal lives with limited symptoms
question
Stage B of Heart Failure
answer
- Stage B Patients with left ventricular dysfunction or structural heart disease who have not developed symptoms of heart failure - pts have slight limitations with ADL, symptoms with activity
question
Stage C of Heart Failure
answer
- Stage C Patients with left ventricular dysfunction or structural heart disease with current or prior symptoms of heart failure - pts have marked limitiation in ADL, comortable at rest
question
Stage D of Heart Failure
answer
- Stage D Patients with refractory end-stage heart failure requiring specialized interventions - pts can't breath or manage themselves at rest (usu tx is heart transplant)
question
UNLOAD FAST for CHF
answer
U - pts will be in *upright position* to help breathing - tripod N - give *Nitrates* to vasodilate and increase tissue perfusion L - give *lasix* (loop diuretic) to loose fluids (will loose K too) O - give *O2* A - give *ACE-Inhibitors* (chronic cough and angioedema can become hypotensive) D - admin *digoxin* F -* fluid restriction* (caution c IV fluids, 1500-2000ml of H2O or less) A - decrease *AFTERLOAD* S - *Sodium restriction* (less than 2g) T - *Test* (ABG's, digoxin level, potassium levels) **will need to give potassium supplement due to lasix**
question
Clinical Mgt of CHF
answer
- Decrease preload - Decrease afterload - Improve contractility
question
Conditions that decrease preload
answer
- tachycardia (ventricles cant fill properly- effects stroke volume) - venous stasis - dehydration (either cellular or vascular): high temp, diarrhea, diuretics, heat
question
Things that affect Afterload:
answer
- vascular tone (constricted vessels increase afterload and dilated vessels decrease afterload) --> System Vascular Resistance --> vasodilators and vasoconstrictors **after load is is the pressure that the ventricles must overcome to eject the blood during systole**
question
Things that affect contractility:
answer
- think Starling's Law: the greater the stretch the greater the force of ejection until the muscle is overstretched then there is hypertrophy and weakened force of contraction ** it is the force generated by the heart muscles**
question
Nursing Care for CHF
answer
- Nursing Process - Assessment - Promote Activity Tolerance - Manage Fluid Volume - Control Anxiety - Be aware of conditions that affect preload/afterload - Interventions that increase venous return which increase preload (foot pumps, massage - distal to proximal, elevate the lower extremities) - fluid retention is a big deal (1500-2000 fluid per day or less) - weight daily - teach to weigh daily at home - pt call md if more than 3 lbs of weight gain in one day - need occup therapist to check to see if home is okay for activity level - teach about diet - may be on home health care - may be on transplant list - may have pacemeaker
question
Nursing Interventions for CHF
answer
- Promote Activity Tolerance - Reduce Fatigue - Manage Fluid Volume - Control Anxiety - Minimize Powerlessness - Promote Home and - Community Based Care
question
Digoxin and CHF
answer
- cardiac glycoside, PO, 0.25 - 0.125 mg, once daily - decreases heart rate and increase contractility to decrease blood pressure - Therapeutic serum digoxin levels range from 0.5-2 ng/mL - be aware for Digoxin overdose - antidote = digifab - check apical and must be 60 or above - pts are "digitalized" = at therapeutic level of drug
question
Digoxin overdose S/S:
answer
EENT: Blurred vision, Halos around objects (yellow, green, white) * Skin: Allergic reaction (see: Stevens-Johnson syndrome), Hives, Rash GI: Diarrhea, Loss of appetite*, N/V, Stomach pain, CV: Irregular heartbeat (or slow), Weakness CNS: Confusion, Depression*, Disorientation, Drowsiness Fainting, Hallucinations*, Headache, Lethargy Psychological: Apathy (not caring what happens) *are usu only seen in chronic toxicity
question
Dopamine drip and CHF
answer
- vasodilator to increase tissue perfusion