General Anesthetics – Flashcards
Unlock all answers in this set
Unlock answersquestion
The state of "general anesthesia" includes: (5)
answer
1. analgesia 2. amnesia 3. loss of consciousness 4. suppression of reflexes 5. skeletal muscle relaxation
question
Which single drug can achieve *balanced anesthesia*?
answer
NO SINGLE DRUG. Combination is used to produce anesthetic state.
question
The onset of inhalational anesthetics is
answer
slow (usually anesthetized with IV agent)
question
Halogenated hydrocarbons are __________ analgesics and a ___________ is ____________.
answer
1. not good 2. supplemental 3. required
question
These drugs are used to provide adequate paralysis for surgical access
answer
Neuromuscular blockers
question
2 types of general anesthetics
answer
1. Inhaled anesthetics 2. IV anesthetics
question
2 types of inhaled anesthetics
answer
1. Gases (i.e. N2O) 2. Volatile Halogenated Hydrocarbons (i.e. halothane)
question
The example of a Gas used as an Inhaled Anesthetic
answer
N2O
question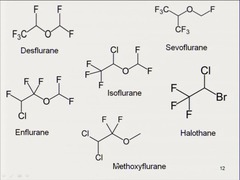
6 examples of volatile halogenated hydrocarbons used as inhaled anesthetics
answer
1. Haloth*ane* 2. En*flurane* 3. Iso*flurane* 4. Des*flurane* 5. Sevo*flurane* 6. Methyoxy*flurane*
question
4 Examples of IV anesthetics
answer
1. Barbiturates 2. Propofol 3. Ketamine 4. Etomidate
question
These general anesthetics are used alone, or in combination with other drugs to: 1. achieve anesthesia; 2. as components of balanced anesthesia; 3. sedate patients in ICU who must be mechanically ventilated for long periods
answer
IV anesthetics: 1. Barbiturates 2. Propofol 3. Ketamine 4. Etomidate
question
These anesthetics are used for maintenance of anesthesia
answer
Inhaled Anesthetics 1. Gases: N2O 2. Volatile Halogenated Hydrocarbons: xxx*furane*
question
6 *Common Features* of Inhaled Anesthetics
answer
1. increased perfusion of brain (i.e. increased ICP) 2. bronchodilation 3. decrease minute ventilation (hypoventilation) 4. potency ? liposolubility 5. rate of onset 1/? blood solubility 6. recovery due to redistribution from brain
question
The actions of inhaled anesthetics are the consequence of direct interactions with
answer
*ligand-gated ion channels*: 1. positive modulation of *GABA-A and glycine* (*G*o on *G*aba and *G*lycine) 2. inhibition of *nicotinic* receptors (*N*o on *n*icotine)
question
Inhaled anesthetics _______________ GABA-A and glycine receptors, while ______________ nicotinic receptors
answer
1. positively modulating 2. inhibiting
question
This is the standard for comparison of potency of general anesthetics
answer
*Minimum Alveolar Concentration (MAC)*
question
The *MAC* refers to
answer
*concentration that results in immobility of 50% of patients when exposed to a noxious stimulus (i.e. surgical incision)* (MAC is expressed as % of alveolar gas mixture)
question
MAC relationship to potency
answer
1. LOW = potent 2. HIGH = weak (Big MAC is weak compared to the Whopper)
question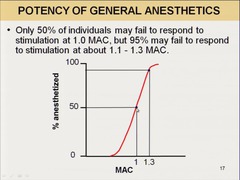
The dose-reponse curves (DRC) for inhalational anesthetics are generally ____________ and the MAC tells us ____________ about the DRC
answer
1. steep 2. nothing (note very small window between 50% anesthetized and 97% anesthetized)
question
The values of various MAC values are
answer
*additive*: 0.7 MAC isofurane + 0.3 MAC N2O = 1 MAC (thus Nitrous Oxide gas can be used as a "carrier gas", decreasing the anesthetic requirement of other inhaled anesthetics)
question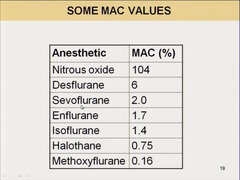
Compare MAC Values
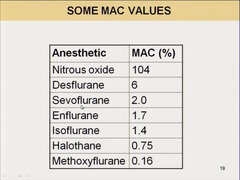
answer
NB: Big MAC = weak; so Methoxyfurane = most potent
question
The Meyer-Overton Correlation
answer
*potency* of anesthetic *predicted by* its *liposolubility*
question
A good measure of the *lipo*solubility of an inhaled general anesthetic
answer
?(oil:gas) (oil:gas partition coefficient)
question
The potency of an anesthetic can be predicted from its
answer
liposolubility (Meyer-Overton Correlation)
question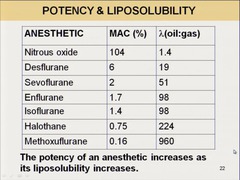
The relationship between ?(oil:gas) and MAC
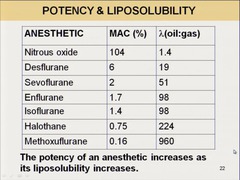
answer
*inverse*: the more liposoluble, the more potent, but the smaller the MAC the less needed to take effect (i.e. not solubilized, rather mobilized)
question
The partition coefficient of an anesthetic is the ratio of
answer
the concentrations of a compound in one solvent to the concentration in another solvent (ex. a ?(oil:gas) of 19 means that the anesthetic is 19x the concentration in oil than it is in alveolar gas when the partial pressure of the anesthetic is identical at both sites)
question
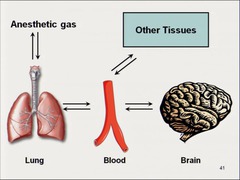
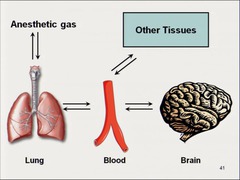
The induction of anesthesia requires transfer of anesthetic from (3)
answer
1. alveolar air -> 2. blood -> 3. brain
question
The rate at which a given concentration of anesthetic in the brain is reached depends on: (5)
answer
1. *solubility of anesthetic* 2. *concentration in inspired air* 3. *pulmonary ventilation rate* 4. *pulmonary blood flow* 5. *arterio-venous concentration gradient*
question
This is a useful index of an anesthetics solubility in blood
answer
?(blood:gas)/blood:gas partition coefficient (defines the relative solubility of an anesthetic in blood compared to air)
question
An anesthetic with low solubility in blood diffuses from lung into the arterial blood and the arterial tension ___________.
answer
rises quickly
question
An anesthetic with high solubility diffuses from lung into the arterial blood and the arterial tension ___________.
answer
rises slowly (more molecules of the anesthetic will dissolve in blood before the partial pressure changes significantly)
question
The relationship between ?(blood:gas) and the rate of rise of its tension in arterial blood
answer
inverse
question
*A low blood:gas partition coefficient determines a __________ onset of anesthesia*
answer
*a faster onset* (molecules less inclined to stay in blood, so they go to brain)
question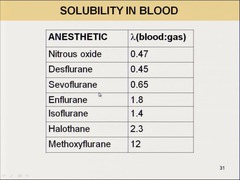
Which anesthetics have the 1) *highest* and 2) *lowest* ?(blood:gas), or the slowest and fastest onsets.
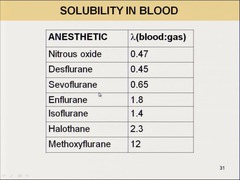
answer
1. methoxyflurane 2. nitrous oxide
question
The ?(blood:gas) of halothane
answer
*2.3; very soluble* in blood, but slow onset (Mnemonic: *H*alothane is *H*appy to be in blood)
question
The ?(blood:gas) of Nitrous Oxide
answer
0.47; quick increase in arterial tension and quick onset
question
The rate of rise of anesthetic gas tension in arterial blood is directly dependent on ______________ and ______________ of ventilation
answer
1. rate 2. depth
question
The magnitude of the effect of ventilation rate on the rise of anesthetic gas tension in arterial blood depends on
answer
the blood:gas partition coefficient
question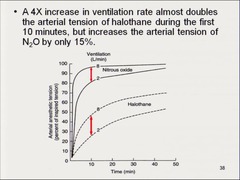
An anesthetic with low blood solubility will cause a ___________ in arterial tension with an increase in pulmonary ventilation
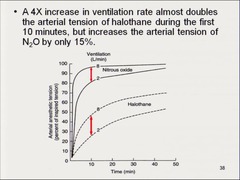
answer
only a slight increase
question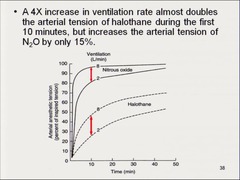
An anesthetic with a moderate or high blood solubility will cause a _____________ in arterial tension with an increase in pulmonary ventilation
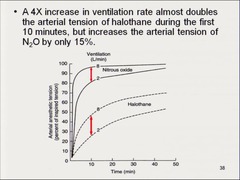
answer
a significant increase
question
An increase in pulmonary blood flow (i.e. increased cardiac output) has this effect on rate of rise of arterial tension of anesthetic
answer
slows the rate of rise (because exposes larger volume of blood to the anesthetic and blood "capacity" increases)
question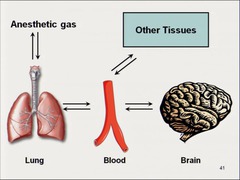
The arteriovenous concentration gradient is dependent mainly on the
answer
*uptake of the anesthetic by tissues*
question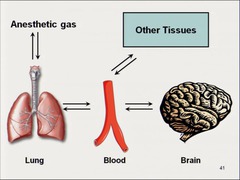
The uptake of anesthetics by tissues has this effect on onset
answer
*slows down the onset*
question
This process is largely the reverse process of uptake of anesthetics
answer
elimination
question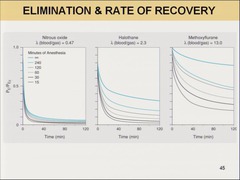
Agents with low blood and tissue solubility will have a recovery from anesthesia that
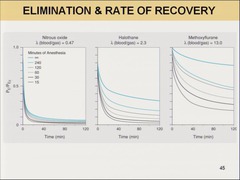
answer
mirrors induction regardless of duration of anesthetic administration
question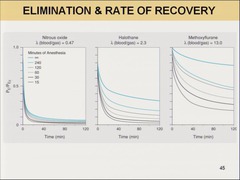
Agents with high blood and tissue solubility will have recovery from anesthesia that is _______________. Why?
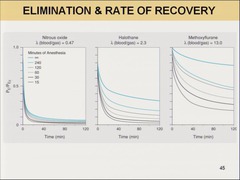
answer
1. a function of the duration of anesthetic administration 2. because the anesethetic accumulated in fat over time, this will prevent blood (and therefore alveolar) partial pressures from falling rapidly (molecule out of blood, another one from accumulation goes into blood)
question
The general effects of inhaled anesthetics on the CVS (2)
answer
1. depress normal cardiac contractility 2. decrease MAP
question
These 2 inhaled anesthetics reduce MAP *mainly by myocardial depression* with little effect on PVR
answer
1. *Halothane* 2. *Enflurane* (Mnemonic: *H*eart *E*ffected more than periphery, not good for people with impaired cardiac function, but could give *scopolamine* to prevent muscarinic effects))
question
These 3 inhaled anesthetics produce vasodilation and have minimal effect on cardiac output
answer
1. *Isoflurane* 2. *Desflurane* 3. *Sevoflurane* (*better choices for patients with impaired myocardial function*)
question
Nitrous Oxide's effect on blood pressure as compared to other inhaled anesthetics
answer
lowers blood pressure *less than* others
question
This inhaled anesthetic *sensitizes the myocardium to circulating catecholamines*, which may lead to ventricular arrhythmias
answer
*Halothane*
question
Volatile anesthetics have this effect on the lungs
answer
1. bronchodilation 2. respiratory depression
question
These 2 anesthetics are "pungent" and therefore not suitable in patients with bronchospasm
answer
1. Isoflurane 2. Desflurane
question
These 2 volatile anesthetics are the most respiratory depressant
answer
1. Isoflurane 2. Enflurane (Mnemonic: severe *E*ffects on *I*nspiration)
question
This inhaled anesthetic is the least respiratory depressant
answer
N2O
question
All inhaled anesthetics have this effect on the CNS and are therefore undesirable in these patients.
answer
1. *increase ICP* 2. patients with increased ICP: a. tumor, or b. head injury
question
At high concentrations, this anesthetic may cause tonic-clonic movements
answer
Enflurane
question
This anesthetic exchanges with other molecules in air-containing body cavities, entering faster than it escapes and therefore can increase the volume and/or pressure of the cavity
answer
*Nitro*us oxide *exchanges* with *nitro*gen in air of air-containing cavity
question
Because of its gas-exchanging capabiltites, this anesthetic should be avoided in these 7 scenarios
answer
*nitrous oxide* 1. pneumothorax 2. obstructed middle ear 3. air embolus 4. obstructed loop of bowel 5. intraocular air bubble 6. pulmonary bulla 7. intracranial air
question
This anesthetic can result in potentially severe, life-threatening and irreversible *h*epatotoxicity that may require transplant
answer
*H*alothane (*H*alothane = *H*epatotoxic (and *H*eart effected)
question
Due to fluoride being released during its *m*etabolism, this anesthetic has nephrotoxic potential
answer
*M*ethoxyflurane
question
This is potentially fatal genetic disorder of skeletal muscle that is triggered in susceptible individuals when they inhale volatile anesthetics (i.e. *halothane*) and depolarizing skeletal muscle relaxants (i.e. *succinylcholine*)
answer
Malignant Hyperthermia
question
Malignant hyperthermia is genetically transmitted as ________________ trait
answer
*autosomal dominant* (incidence is 1:12,000)
question
*This is one of the main causes of death due to anesthesia*
answer
Malignant hyperthermia
question
A patient is begun on anesthesia and develops *tachycardia*, *hypertension*, *severe muscle rigidity*, *hyperthermia*, *hyperkalemia* and *acidosis*. They are experiencing
answer
malignant hyperthermia
question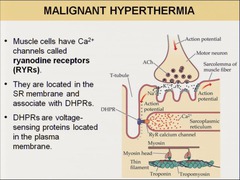
The genetic defect in malignant hyperthermia is in the ____________ *gene* and syndrome results from _____________. The treatment is with _____________.
answer
1. *ryanodine receptor gene (RYR1)* 2. *altered control of Ca++ release from SR* 3. *Dantrolene*: blocks Ca release from SR
question
The *ryanodine receptors (RYRs)* are located
answer
on the sarcoplasmic reticulum of muscle cells
question
The ryanodine receptors associate with
answer
DHPRs: voltage-gated proteins in plasma membrane in T-tubule
question
The defective ryanodine receptor leads to
answer
unregulated Ca release from the SR of muscle cells
question
The increased Ca concentration in muscle cells after release by defective ryanodine receptors leads to (5)
answer
1. sustained muscle contraction that generates heat 2. accelerated aerobic metabolism produces CO2 and depletes O2 and ATP 3. anaerobic metabolism dominates and worsens acidosis 4. energy stores are depleted 5. muscle fibers die -; release K+ and myglobin
question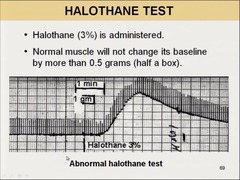
The most *reliable* test to establish malignant hyperthermia
answer
*Caffeine-Halothane Muscle Contraction Test* 1. muscle sample removed from thigh (with anesthesia not known to cause MH) 2. strips prepared 3. strips put in physiological bath 4. attached to simulator (twitches every 10 s) 5. strength measured 6. Halothane (3%) or 2 mM caffeine administered 7a. . Normal muscle will not change baseline by more than 0.5 gm 7b. abnormal indicated by ;0.2 gm evoked by caffeine
question
Prolonged exposure to this anesthetic can decrease methionine synthase activity and cause megaloblastic anemia, which can present as this potential occupation hazard for staff working in poorly ventilated dental operating suites
answer
*Nitrous Oxide* and *hematotoxicity*
question
4 Intravenous Anesthetics
answer
1. Barbiturates 2. Propofol 3. Ketamine 4. Etomidate
question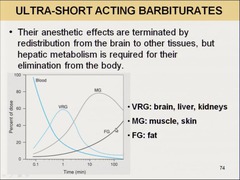
2 "ultra-short acting* barbiturates
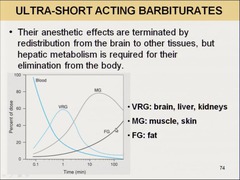
answer
1. *thiopental* 2. *methohexital*
question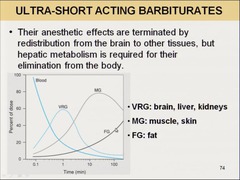
These 2 ultra-short acting barbiturates are used for induction of anesthesia and for short surgical procedures
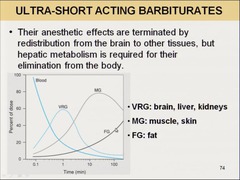
answer
1. thiopen*tal* 2. methohexi*tal*
question
Ultra-short acting barbiturates have this effect on ICP
answer
*decrease* ICP (good combo with volatile inhaled anesthetics)
question
With respect to pain, barbiturates may cause
answer
hyperalgesia
question
Barbiturates are a concern for these patients because of their potential AEs
answer
1. asthmatic 2. apnea, coughing, chest wall spasm, laryngospasm, bronchospasm
question
This is the most popular IV anesthetic that *does not often cause postoperative vomiting* and is used for induction and maintenance of anesthesia
answer
propofol
question
Propofol produces no ___________, is rapidly metabolized by ____________, is a potent ______________ and reduces ______________.
answer
1. no analgesia 2. metabolized by the liver 3. potent respiratory depressant (MJ) 4. reduces ICP
question
This IV anesthetic is primarily used for anesthetic *induction of patients at risk for hypotension*
answer
Etomidate
question
This IV anesthetic is *associated with nausea and vomiting* and may *inhibit steroidogenesis* with decreased levels of hydrocortisone
answer
Etomidate (Mnemonic: *E*tomid*ate* is *E*metic and can make you aspir*ate* so give Odansetron)
question
This IV anesthetic produces anesthesia characterized by catatonia, amnesia, and analgesia with or without loss of consciousness
answer
*Ketamine* produces *dissociative anesthesia*
question
This is the only IV anesthetic with analgesic properties and the ability to produce CV stimulation
answer
Ketamine (*K*etamine may change your E*K*G)
question
This IV anesthetic increases ICP
answer
Ketamine (*K*etamine is not good for you *K*ranium)
question
This IV anesthetic can cause sensory and perceptual illusions and vivid dreams. This is called ______________ and can be reduced with ____________ (3)
answer
1. ketamine 2. *'emergence phenomena'* 3. diazepam, midazolam, or propofol
question
*Neurolept analgesia* can be established with the combination of (2)
answer
1. *fentanyl* (potent opioid) 2. *droperidol* (potent neurolept)
question
Neurolept analgesia may be converted to ____________ by the concurrent administration of ____________.
answer
1. *neurolept anesthesia* 2. 65% N2O in O2
question
5 Adjuvants to Anesthetics
answer
1. *Benzodiazepines* 2. *Opioids* 3. *Neuromuscular blockers* 4. *Antiemetics* 5. *Antimuscarinics*
question
BZDs are used as anesthetic adjuvants for
answer
anxiolytic and anterograde amnestic properties
question
Opioids are used as adjuvants for anesthesia for
answer
analgesia
question
NM-blockers are used as adjuvants to anesthesia in order to
answer
achieve muscle relaxation
question
Antiemetics, such as ___________, are used to
answer
1. *ondansetron* 2. prevent possible aspiration of stomach contents (possibly from Etomid*ate*, which may make you aspir*ate*)
question
Antimuscarinics such as ____________ are used for (3)
answer
*scopolamine* 1. amnestic effects 2. prevent salivation and bronchial secretions 3. protect the heart from bradycardia caused by inhalational agents (i.e. H&E) and NM blockers



