Anesthetic Monitoringand Recovery – Flashcards
Unlock all answers in this set
Unlock answersquestion
Anesthetic Monitoring
answer
During anesthetic maintenance, the anesthetist has 2 important responsibilities -Animal must be monitored closely to ensure that the vital signs (esp. HR and RR) remain within acceptable limits -The anesthetist must maintain the animal at an appropriate anesthetic depth (neither too light nor too deep)
question
Why?
answer
If the animal is too light—will feel pain, may "wake up" and struggle during surgical procedure. If the animal is too deep—will have prolonged recovery, may have anesthetic overdose leading to death. This type of death is preventable and unacceptable
question
Patient Monitoring & Anesthetic Depth
answer
The anesthetist should monitor as many variables as possible and weigh all evidence before judging anesthetic depth of the patient. Each animal is unique and has an individual response to increasing anesthetic depth Determination of anesthetic plane by monitoring only one reflex or vital sign will eventually result in disaster.
question
Constant Monitoring is Best
answer
Variables to be assessed every 5 minutes Respiration rate, depth, and character Mucous membrane color and CRT Heart rate Pulse strength and rate Jaw tone, eye position, and palpebral reflex activity Oxygen flow rate (flowmeter) IV catheter placement and fluid administration Body temperature
question
Vital Signs
answer
Important to observe both vital signs and reflex activity Vital sign—those variables indicating the response of the animal's homeostatic mechanisms to anesthesia
question
Reflex Activity
answer
Involuntary response to a stimulus Gives information on depth of anesthesia
question
Heart Rate and Rhythm
answer
Minimum acceptable heart rate is 60 bpm in the dog, 100 bpm in the cat Heart rates < 25 in the adult horse are considered abnormal (what is the normal HR in the horse?) Lower heart rates may be due to excessive anesthetic depth or other problems and DVM should be notified immediately Cardiac rhythm should be normal ______. This means that the ____ node is setting the pace of the heart. A common arrhythmia, but of no clinical significance, is _________
question
heart rate under anesthesia
answer
awake dog: 70-180 awake cat:145-270 asleep dog: 60-120 asleep cat:110-220 Changes due to depressant effect of most anesthetics on heart rate and myocardial function. What drugs may actually increase heart rate? How may a patient's signalment affect the above reference values?
question
Bradycardia
answer
An animals heart rate is expected to be somewhat lower under anesthesia than when awake, but if falls below an acceptable level, can be life-threatening. -Alert surgeon if < 100bpm cat -Alert surgeon if < 60bpm dog Reasons for a decreased heart rate can include -Hypothermia -Response to Anesthetic drug (cardiac depression) -Systemic depression -Increased CO2 (inadequate ventilation)
question
How Can We Treat Bradycardia?
answer
Heart rate can be increased by: Reversal of anesthetic agents Lightening plane of anesthesia Warming the body temperature Providing adequate oxygenation Pain stimulation Administration of positive cardiotropic agents (anti-cholinergic drugs) -Atropine -Glycopyrrolate
question
Tachycardia
answer
Heart rates can increase due to -Shock -Bleeding -Pain (Note: SHOCK is in this category. A rapid heart rate does not always indicate a light plane of anesthesia and other monitoring parameters must be assessed prior to increasing anesthetic depth) Regardless of the reason that tachycardia occurs alert surgeon if: >180bpm large dog >200bpm small dog >220bpm cat However, keep in mind that there are no "set limits" If you are worried about the patient and feel something is "not right" consult doctor and alert staff
question
Cardiac Monitoring
answer
Can be accomplished by: Placing a hand over the chest wall or pulse Auscultation of the chest wall with a stethoscope Anesthetic monitoring equipment
question
Esophageal Stethoscope

answer
Allows auscultation of the heart when the chest is not accessible Thin, flexible tube attached to either regular stethoscope in place of the stethoscope head, or attached to auditory transmitter Tube is inserted through the oral cavity into patient's esophagus until at base of heart—correct placement confirmed when audible heart beat detected. Some esophageal stethoscope probes also contain ECG leads or temperature monitors Audible heart beat does not mean circulation is adequate Can be attached to stethoscope ear piece, as shown here, or may be attached to amplifier system.
question
Electrocardiogram
answer
Direct visualization of the electrical activity of the heart Allows interpretation of heart rate and rhythm Does not tell about heart function (need echocardiogram). Remember electrical activity can continue in the absence of a functioning heart Multiple methods available—can have wire lead attachments that attach to the patient or leads that are within in esophageal
question
Remembering EKG Leads
answer
Newspapers are delivered to the front porch; Christmas is at the end of the year Smoke over Fire Snow on the Grass Green and white are always right
question
EKG
answer
There must be a good contact between the ECG leads and skin Alcohol provides for good contact but it evaporates rapidly requiring frequent application, and is not as good for long-term monitoring.
question
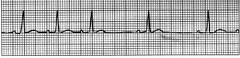
Normal Sinus Rhythm
answer
A sinus rhythm is a rhythm which originates in and is controlled by the sinoatrial node. This rhythm is the normal cardiac rhythm in all domestic animals. To determine if a rhythm is sinus or not based on the EKG requires the following criteria: -There is a P wave for every QRS complex. -The PR interval is relatively constant especially if the R wave to R wave interval varies. -The P wave is positive in lead II
question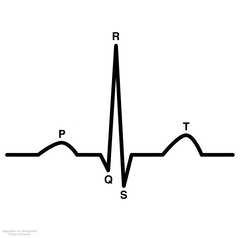
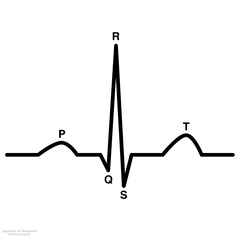
P Wave
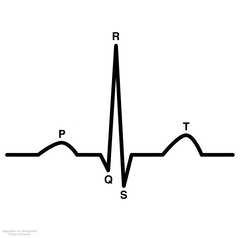
answer
The P wave is the electrocardiographic representation of electrical activation of the atrial myocardium The PR interval is the electrocardiographic representation of the delay in electrical activation of the ventricles after sino-atrial nodal discharge
question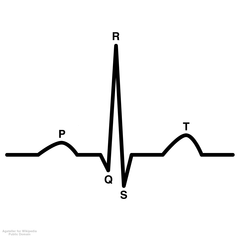
QRS Complex
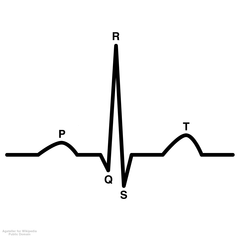
answer
The QRS complex is the electrocardiographic expression of the electrical activation (depolarization) of the ventricular myocardium
question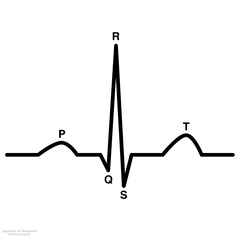
T Wave
answer
The T wave is the electrocardiographic expression of repolarization of the ventricular myocardium (getting ready for next impulse)
question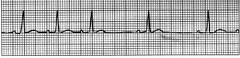
sinus arrhythmia
answer
Not all arrhythmias are pathologic Sinus arrhythmias are phasic and usually associated with respiration The heart rate increases with inspiration and decreases with expiration due to the influence of vagal tone
question
Pulse Oximetry
answer
Measures the percentage of hemoglobin saturated with oxygen in arterial blood Also monitors pulse rates Abbreviated as SpO2 Works on the principle that hemoglobin absorbs red and infrared light at different wavelengths -Depending on whether the hemoglobin is bound to oxygen (infrared) or deoxygenated (red). Uses two light-emitting diodes that pulse red and infrared light through perfused tissue several hundred times per second. The amount of light absorbed at each wavelength is measured by sensitive photodetectors. -The absorption data is expressed as a percentage of oxygenated hemoglobin to total hemoglobin.
question
Pulse Oximetry Sensors
answer
pick which sensor best to use based on animal, mm color, surgical procedure
question
Lingual Sensor
answer
looks like a clothespin. Most commonly used on the tongue. The Lingual sensor can also be applied to the pinna of the ear, webbing between toes, vulva or prepuce, or other hairless body region
question
Reflective probe
answer
can be used with a protective sleeve and placed inside the rectum or used alone on the underside of the tail.
question
Universal C-clamp
answer
designed for feet, hocks
question
Reliability of the Pulse Ox
answer
While this machine is commonly used in practice, primarily due to ease of use and low cost, can be unreliable/subject to mechanical error Note that when a patient is attached to a breathing circuit and placed on 100% oxygen, the SpO2 reading should be >95%. If the reading drops below 95% the technician should immediately evaluate the patient to determine the reason for the decrease
question
Troubleshooting—Reasons for Decreased SpO2
answer
Before checking equipment, listen to heart ensure animal is stable. If not, alert doctor. Look at anesthesia machine, ensure animal is receiving O2, there is an adequate oxygen supply and that the pop-off valve is open THEN check pulse ox -Sensor may have slipped from proper position -Tongue/mm may have dried out affecting transmission from the probe -In these situations, repositioning or wetting mm surface should result in return of normal values
question
Reasons for Low SpO2
answer
If, after troubleshooting machine, the SpO2 still displays a below normal reading, the patient may have had a change in its physiological status -Patient may have impaired gas exchange even if RR is normal. May require hand ventilation -Alert doctor
question
Capillary Refill Time
answer
Rate of returning color to a mucous membrane after the application of gentle digital pressure. Reflects the perfusion of tissues with blood Placement of pressure on the mm compresses blood flow within the capillaries Release of pressure allows blood flow to return to the area Capillaries refill with blood and color returns
question
A prolonged CRT
answer
(>2 seconds) indicates perfusion to the area is not adequate and that tissues to the area have a reduced blood supply. This may be due to -Vasoconstriction (secondary to shock, hypothermia, excessive anesthetic depth, or drug induced) -Decreased blood pressure. At the same time, a normal CRT (<2seconds) does NOT mean that perfusion is normal. -Remember an animal can have a normal CRT soon after death
question
Where can we evaluate CRT & mm color?
answer
Gingival mucosa Tongue Conjunctiva of lower eyelid Mm of prepuce or vulva
question
Blood Pressure
answer
Force exerted by flowing blood on arterial walls Best measured using blood pressure equipment - can be estimated by palpating a major artery and determining the strength of the pulse The pulse should be strong and synchronized with the heart beat Reflects the adequacy of blood circulation throughout the body
question
Where can we palpate pulses?
answer
Femoral Carotid Dorsal pedal Lingual Facial
question
Pulse pressure
answer
the pressure detected by manual palpation is the difference between the systolic and diastolic pressures. Pg 245 - 248, Pg 138-182
question
Hypotension under anesthesia may be due to
answer
Excessive anesthetic depth Excessive vasodilation Cardiac insufficiency (or preexisting heart ds) Excessive blood loss and hypovolemia
question
Normal Blood Pressure
answer
120/80 mmHg IS GENERALLY CONSIDERED TO BE THE NORMAL BP IN CATS AND DOGS.
question
Normal ranges for diastolic blood pressure
answer
(pressure during diastole or filling phase of heart beat) = 50-90 mmHg
question
Normal ranges for systolic blood pressure
answer
(pressure during systole or contraction phase of the heart beat) = 90-160 mmHg
question
MAP
answer
mean arterial blood pressure is determined by the systolic and diastolic pressure ranges from 85-120. The MAP should be maintained above 70 mmHg at all times under anesthesia. The mean arterial pressure (MAP) is the major determinant of perfusion pressure to the organs of the body. If the MAP falls below 70, blood flow to internal organs is reduced and tissues may become hypoxic. The kidneys are especially sensitive to this effect.
question
Direct Monitoring of Blood Pressure
answer
Involves placement of a catheter in an artery, then attaching a transducer to the catheter Transducer is connected to an oscilloscope that displaces the diastolic, systolic, and MAP as well as a waveform representing pulses More invasive than indirect (involves arterial catheterization). Especially difficult in cats and small dogs. More $$ equipment More accurate method than indirect monitoring In private practice, indirect methods of blood pressure monitoring are more commonly used.
question
Indirect Blood Pressure Monitoring
answer
Less invasive, less technically difficult than direct monitoring Equipment is used to occlude blood flow through an artery, and then detect the pressure at which some flow resumes (systolic pressure), the pressure at which normal flow is reestablished (diastolic pressure, or the average pressure (MAP) With both the Doppler and Oscillometric technique, generally 3 - 5 pressure readings are taken at a time and the middle reading recorded (discarded highest and lowest readings)
question
three main ways for Indirect Blood Pressure Monitoring
answer
-The noise made by the returning blood flow may be auscultated with a stethoscope (man; difficult in animals) -A doppler flow probe detects an ultrasound echo from red blood cells passing through the vessel, and thereby determines systolic pressure. -An oscillometer can detect the distention of the limb because of the increased volume of blood pulsing through the artery and limb with each heartbeat. Systolic, diastolic and MAP can be determined by this method
question
Doppler
answer
-Doppler crystals are placed on the skin over arteries producing an audible pulse beat. The Doppler probe emits a series of high-frequency sound waves. When the sound waves encounter a pulsating artery, the frequency is changed. This is detected by the instrument, which converts the sound into an audible "swishing" noise. -Can be used to assess pulse quality and blood pressure trends. -Addition of a sphygmomanometer and cuff, placed proximally to the doppler crystal enables assessment of systolic blood pressure.
question
Ultrasonic Doppler
answer
The ultrasonic doppler blood pressure device is considered the most accurate indirect method of blood pressure assessment in small animals. Doppler can be used in exotic species and neonatal animals to monitor pulse rate by placing the lubed crystal on a well lubed cornea. An audible pulse rate will be obtained
question
Using a Doppler BP
answer
Using a BP cuff that is too large or too small will result in a false reading The width of the cuff should be no more than 40% of the circumference of the leg around which the cuff is to be placed The sensor probe must be placed with the concave portion of the probe lying on the patient's skin. An artery should be palpated and the arrow on the cuff should be placed over the artery. Clip hair from the area the probe will be placed to ensure good contact Only ultrasound gel should be used on the probe The probe should ONLY be cleaned with water, NEVER alcohol or disinfectants.
question
Oscillometric Technique
answer
Consists of a cuff detector unit connected to a computerized monitor. Measures blood pressure by detecting oscillations within the cuff bladder which is placed over an artery (distal limb or tail) Oscillations are caused by the pulsation of the artery beneath the cuff, which changes the volume of the limb slightly The device the calculates the systolic mean, and diastolic pressures from these cuff pressure changes. More expensive than the Doppler Work automatically Allow determination of diastolic and mean in addition to systolic More accurate in large and medium patients
question
Respiratory Rate and Rhythm
answer
One inhalation + one exhalation = one breath. Count only inhalation or only exhalation when counting RR (breaths per minute) Generally, counts are made for 15 seconds and multiplied by 4 to determine per minute rate
question
Normal respiratory rate under anesthesia for dogs and cats
answer
is 8-20 breaths per minute. Monitor by: Watching rebreathing bag Watching animals chest movements Listen with a stethoscope Watch inspiratory/expiratory valves (least preferred)
question
Respiratory Rate Monitoring
answer
RR < 6-8 bpm alert doctor. Turn down anesthetic gas. The most likely reason for decreased respiratory rate (bradypnea) is an increased anesthetic depth. Respirations will stop before the heart stops when anesthetic depth drops to a dangerous level and is an emergency
question
Respiration Monitoring
answer
Depth and character of breathing must also be monitored At deeper planes of anesthesia, there is normally a decrease in both RR and volume of air taken with each breath (tidal volume) A decrease is RR and Vt = hypoventilation Tidal volume decreases by at least 25% in most anesthetized animals
question
Hypoventilation
answer
As tidal volume decreases, some alveoli in the lung will receive less air for gas exchange than they normally would As a result, the alveoli will partially collapse, leading to atelectasis This is especially a problem in the "down" lung in a laterally recumbent patient In early stages can be reversed by "bagging" the patient or by giving a full breath to fully inflate the lungs
question
Atelectasis
answer
In some practices, patients are routinely given a breath every 5-10 minutes while under anesthesia For long surgical procedures, such as orthopedic repairs, a mechanical ventilator should be used to prevent hypoventilation and atelectasis. Question: In what other circumstances would a artificial ventilation be necessary?
question
How to "Give A Breath"
answer
1. Close pop-off valve 2. Squeeze reservoir /rebreathing bag 3. WATCH pressure gauge—give up to 20 cmH20, however, if your patient is small don't exceed 10-15cmH2O. 4. Do not hold breath for > 2 seconds 5. After giving breath, OPEN pop-off valve
question
Difficulty Breathing
answer
Alert doctor if you notice gasping or labored breathing. Check to ensure adequate fresh gas flow, check oxygen supply, check ET tube for obstruction and correct placement, check pop-off valve. If O2 too low > increase, replace tank if needed If ET tube clogged, may need to re-intubate with clean tube or suction tube If reservoir bag too full, be sure pop-off valve is open, squeeze bag to reduce pressure, turn down oxygen flow rate
question
Capnometer / Capnograph
answer
Measurement of CO2 level in a patient's exhaled breath; Also known as ETCO2, or End-Tidal CO2 Allow evaluation of patient respiratory rate and quality of respirations Not as good as arterial blood gas at determining blood CO2 levels
question
Capnograph Measurement
answer
B-C segment recorded during exhalation. D-E segment recorded during inhalation—inspired CO2 levels are close to zero
question
Normal levels of expired CO2
answer
35-45 mmHg in dogs and cats
question
Hypocarbia
answer
(ETCO2 values < 35mmHg) can be due to Overzealous artificial ventilation, Increased RR Light anesthetic plane Pain Hypoxia -Solve by decreasing frequency of assisted RR, insure proper O2 supply, address pain, deepen anesthetic depth
question
Hypercarbia
answer
(ETCO2 > 45mmHg) can be due to Hypoventilation/decreased RR Exhausted soda lime Kinked ET tube, Malfunction of unidirectional valves in anesthesia machine. Check machine, alert doctor, give a breath!
question
Maintaining Body Temperature
answer
Body temperature is an important parameter to monitor during anesthesia/surgery. Tendency for anesthetized animals to lose body heat -Supplemental heat sources are often required to prevent hypothermia A patients body temperature should be recorded in your preanesthetic exam, and then every 15 minutes during anesthesia Some clinics will have continual monitoring of body temperature using a rectal or esophageal device that will monitor core body temperature.
question
Why Does Hypothermia Develop?
answer
Anesthetic drugs relax muscles Inhibiting the shivering response that would normally initiate when temperature drops. Metabolic rate is also decreased, decreasing normal production of body heat Shaving surgical site Washing and rinsing with alcohol cools the body through the evaporation of alcohol on the skin.
question
Hypothermia
answer
Hypothermia not only depresses an animals body functions, but also changes their anesthetic requirement. Hypothermia itself functions as an "anesthesia" agent by depressing these functions. As a result your patient may become "too deep" causing detrimental effects. Lower body temperature at the end of surgery will result in -Prolonged anesthetic recovery, -Increased muscle contractions (shivering) resulting in a higher oxygen demand and undue stress on the patient
question
Reflex
answer
an automatic reaction to a stimulus made by the animal w/out conscious awareness of the reaction.
question
Reflex Evaluation
answer
As anesthetic depth increases, reflex activity decreases until it eventually disappears Reflexes exist to keep animals from harm - ex. the swallowing reflex is triggered by a foreign object in the pharynx. Return or increasing strength of reflexes under anesthesia indicates the level of anesthesia is becoming lighter
question
Palpebral Reflex (blink)
answer
protects the globe from injury by the eyelids quickly closing. Can be triggered by lightly touching the medial canthus of the eye. The reflex is diminished and then may disappear as the patient's anesthetic depth deepens. During recovery phase, this reflex returns just prior to the laryngeal reflex.
question
Corneal Reflex
answer
When the cornea is touched, the animal will blink or retract the globe in response This reflex will remain present until very deep levels of anesthesia Not used to monitor anesthesia (as can traumatize cornea) but more often used to help assess point of death during euthanasia
question
Jaw Tone
answer
Muscles of the jaw should be decreased under anesthesia. Jaw tone can be used, combined with other findings, to determine if animal is too light. Test the resistance of the mouth to opening by carefully prying the jaws apart. In cases such as dentals where the jaw is not available to assess tone, anal tone can be assessed. In the conscious animal the anal sphincter is usually closed, anal tone generally relaxes as an animal becomes deeper
question
Eye Location
answer
Begins in central position, as the patient moves into a light to moderate depth the eye rotates rostroventrally As the patient moves to a deeper plane of anesthesia the eye rotates back to the central position—Note that at both a very light and very deep plane the eyes will be located centrally Gravity has some effect on eye position when the patient is placed in dorsal recumbency Reliable indicator in the dog and cow
question
Pedal Reflex
answer
Aka,"Withdrawal" reflex Tested by squeezing or pinching a digit or pad and observing if the patient withdraws the limb. If present indicates inadequate depth for surgical stimulus. Useful in mask inductions where the animal's face is not available
question
Stage 1 anesthesia
answer
Stage of voluntary movement Lasts from initial anesthetic administration to the loss of consciousness Tachycardia and hypertension may be present Irregular or increased respirations Patient may hold breath Pupils dilate Struggling may be present as animal becomes ataxic
question
Stage 2 anesthesia
answer
Stage of delirium or involuntary movement "excitement stage" CNS becomes depressed Loss of voluntary control Reflexes become more primitive and exaggerated Struggling, breath holding, tachypnea, hyperventilation Cardiac arrythmias may occur Eyelash and palpebral reflexes are present Vocalization Salivation Susceptible to laryngeal spasm
question
Stage 3 anesthesia
answer
Stage of surgical anesthesia Pulse rate returns to normal values Muscles relax Swallowing and vomiting reflexes are lost Divided into 3 or 4 planes depending on the reference Three planes: Light, medium, deep Four planes: I-IV
question
Stage 3, Plane I/Light
answer
Eyeball movement ceases Blood pressure returns to normal Strong pulse Begins decrease of respiratory rate and depth Pupils become less dilated Eyeball may rotate Palpebral reflex present Slight reaction to surgical manipulation Loses jaw tone
question
Plane II/(Medium)
answer
Surgical anesthesia (VTNE question) Bradycardia begins Hypotension increases Capillary refill time begins to slow Palpebral reflex diminishes and disappears Eyeball rotates ventrally Abdominal muscle tone finally lost Jaw tone minimal Pedal reflex absent
question
Plane III/(Medium)
answer
Deep surgical anesthesia Intercostal and abdominal muscle tone minimal Diaphragmatic breathing present Profound muscle relaxation present Centered and dilated pupil Bradycardia intensifies Hypotension continues to increase Respiratory rate and depth continue to decrease
question
Plane IV/Deep (Overdose)
answer
Respirations slow and irregular Lowered heart rate Cyanosis seen Widely dilated pupil and unresponsive to light Flaccid muscle tone Jaw tone lost Sphincter control lost
question
Stage 4:
answer
Beginning to die CNS extremely depressed Respirations slow and cease Heart begins to cease beating Blood pressure at shock level Capillary refill time is greatly increased Pupils relax Dysrhythmia probability at furthest level All reflexes and tone lost
question
Reliable signs of light anesthesia without conscious perception of pain
answer
Purposeful, spontaneous movement Reflex movement in response to surgical stimulation Transient hemodynamic or respiratory changes in response to surgery (peaks in HR and RR in response to surgical stimulus) Horses—nystagmus at light planes of anesthesia
question
Unreliable Signs of Depth
answer
Pupil size—too variable Shivering in response to hypothermia (Don't increase anesthesia as hypothermia influences MAC value) Heart rate: dose related decrease, but considered insensitive due to the numerous causes of changes in heart rate. -Bradycardia may be life threatening—deep anesthetic plane is one potential cause that needs to be ruled out. Bradycardia should be treated. Breathing rate: similar to heart rate: apnea and tachypnea may both occur with light and deep planes of anesthesia, as well as when agonal Blood pressure: similar to heart rate; generally increases if lighter but not always When vitals are concerned, check your patient, don't just jump to change the vaporizer setting
question
Respiratory Consequence Tachypnea
answer
Too light, too deep Hypercarpnia Hyperthermia Hypotension Atelectasis Pain Recovery/induction Pharmacological Individual variation
question
Respiratory Consequence Bradypnea
answer
Too light/too deep Respiratory center malfunction/CNS dysfunction, Drugs Individual/species variation
question
Bradycardia
answer
drugs excessive anesthetic depth vagal tone terminal hypoxia hypothermia toxemias
question
Tachycardia
answer
light/deep anesthesia pain Hypovolemia hypotension Hypoxemia hypercapnia hyperthermia drugs endogenous (hyperthyroid) myocardial conduction disturbances
question
Non-Signs of Anesthetic Depth
answer
Spasmodic muscular twitching of focal muscle groups (ketamine, propofol) Cats may flick ears when hairs are touched, regardless of anesthetic level Flaring of nares and muzzle movement with respiration
question
During Anesthesia
answer
Keep Records -record vitals at minimum of every 5 minutes. -Record any drugs given during the anesthetic period, including emergency drugs. Legal document
question
Be Sure to
answer
Ensure patient comfort Position patient comfortably during anesthetic event -Arthritic / care tying down limbs -Protect bony prominences -Help maintain body temperature Lubricate eyes every 90 minutes -Blink reflex absent -Medications, esp atropine/glyco, decrease tear secretion -Risk abrasion and corneal ulcerations
question
"Hooking and Unhooking"
answer
Remember, O2, patient to machine, then turn on anesthetic gas Unhooking (repositioning/recovery), turn off anesthetic, disconnect patient, then turn off O2 Oxygen is needed for life, please never have the patient attached to the anesthetic machine without turning the oxygen on first.
question
After turning off anesthetic gas
answer
Animal should be maintained on 100% 02 for 5 minutes before disconnecting patient from circuit Why? Decrease pollution (from both machine and patient's exhaled air) Prevent hypoxemia: -Animal has increased requirements during recovery periods (ex. Shivering), -Decreased tidal volume secondary to anesthesia and prolonged recumbency (hypostatic congestion) -Risk of respiratory distress or apnea during recovery (same concept as pre-oxygenating)
question
Anesthetic Recovery Period
answer
Reverse of Induction—reflex activity, muscle tone, and sensitivity to pain are regained as consciousness returns. The maintenance period ends and recovery period begins when the concentration of anesthetic in the brain begins to decrease The method by which the anesthetic is eliminated from the brain and circulatory system varies according to the anesthetic agent Most injectable drugs are removed from the body by the liver and undergo metabolism by liver enzymes. The metabolites are excreted by the urinary system Some drugs do not undergo metabolism and are excreted unchanged by the kidneys Inhalant agents are primarily eliminated by the respiratory tract Anesthetic molecules leave the brain, enter the blood, then the alveoli of the lungs and are exhaled. An animal recovering from general anesthesia gradually progresses back through the same anesthetic stages that were experienced during induction As animal becomes lighter, heart rate, respiratory rate and volume will increase. The pupil moves back to its normal central position Reflex responses return and become stronger Animal may then shiver, attempt to swallow, chew, or lick After swallowing, the animal will normally show signs of consciousness including movement of the head and limbs and vocalizing
question
Patient Stimulation
answer
Patient recovery may be hastened by gentle stimulation Talking to patient, pinching toes, opening mouth, gently moving limbs, rubbing of the chest This type of stimulation increases the flow of information to the reticular activation center (RAC) of the brain, which is the area responsible for maintaining consciousness in the awake animal Be wary; stimulation followed by premature extubation may cause the patient to later return to a level where they may not be able to effectively guard airway
question
Patient Reassurance
answer
Disorientation +/- pain during recovery can result in patient self-trauma as well as accidental bites Some animals may pass through a period of excitement before fully regaining consciousness -Vocalization, delirium, hyperventilation, head thrashing and paddling of the limbs may be seen Calm, quiet, padded, warm environment Additional sedatives/analgesics sometimes necessary
question
Postoperative analgesics
answer
Preferably given before animal experiences any pain Animal should be able to sleep comfortably Animal should demonstrate minimal if any signs of pain postoperatively
question
Nursing care
answer
Heat to all hypothermic animals -Warm towels, hot water bottles wrapped in towels, heat lamps (approx 1 m from animal), incubator, etc -Gentle rewarming better than fast warming -Ample bedding to prevent heat loss and increase patient comfort
question
Prevent self trauma
answer
Observation Tranquilization/analgesia for some patients Don't leave animal on table unobserved Don't leave cage door open when not attended Remove food and water bowls
question
Other post op problems
answer
Removal of sutures Hemorrhage Aspiration of vomit Burns



