Anesthesia Neuro Assessment – Flashcards
Unlock all answers in this set
Unlock answersquestion
CN I
answer
olfactory sense of smell
question
CN II
answer
optic sense of sight
question
CN III
answer
oculomotor movement of the eye pupillary constriction and accommodation
question
CN IV
answer
trochlear movement of the eye
question
CN V
answer
trigeminal general sensation of the face, scalp, cornea, nasal/oral cavity opens/closes mouth (muscles of mastication)
question
CN VI
answer
abducens movement of the eye
question
CN VII
answer
facial taste - anterior 2/3 of tongue facial movement salivation and lacrimation
question
CN VIII
answer
vestibulocochlear hearing propriception of the head balance
question
CN IX
answer
glossopharyngeal sensory supply to the palate - gag reflex swallowing salivation taste - posterior 1/3 of tongue chemo/baroreception in carotid body and sinus
question
CN X
answer
vagus general sensation of the pharynx, larynx, esophagus chemo/baroreceptors of the aortic bodies/arch visceral sensation of abd and thorax speech and swallowing - moves soft palate, larynx, pharynx, upper esophagus control of CV, resp, GI systems
question
CN XI
answer
spinal accessory movement of head and shoulders via sternomastoid and trapezius
question
CN XII
answer
hypoglossal movement of the tongue
question
neuro physical exam - things to assess/ questions to ask
answer
LOC Speech Extremity Strength Range of Motion ETOH Prescription Medications Recreational Drug Use
question
why is it important to know and assess a pts range of motion
answer
May cause further injury if over- extension occurs while the patient is anesthetized Communicate with the surgeon . May need to change the way the surgery is going to be proceeded. You do not want the pt to wake up with an injury or pain
question
effects of acute alcohol intoxication
answer
Sedative effect Dehydration Diuresis Vasodilation Hypotension Tachycardia Consider Metabolic Acidosis increased CNS effects with sedatives, hypnotics, narcotics
question
chronic alcoholism and anesthesia considerations
answer
Increased tolerance Careful with drug choice if patient has liver damage! withdraw - DTs
question
anesthetic considerations in a pt w spinal cord injury
answer
Consider: Where is the level of injury? Has the patient lost motor, sensory or both? Muscle Relaxation? Pain Control? High level or low level of SCI? Quadripalegia? Paraplegic? If a pt has no sensation in lower extremeties they may need anxiolysis, but perhaps not pain control. How invasive is the procedure? SCI may have sensory but no motor - ask the pt what they can and cannot do. May have fine motor but not gross motor. Maybe they have a tick or jerk or termor = may need them to be asleep because of this be mindful of autonomic dysreflexia and hyperkalemia from sux
question
autonomic dysreflexia
answer
can happen if pt has the SCI at T6 or higher. any kind of noxious stimulus below level of injury causes sudden high BP. If left untreated, autonomic dysreflexia can cause seizures, retinal hemorrhage, pulmonary edema, renal insufficiency, myocardial infarction, cerebral hemorrhage, and, ultimately, death. Complications associated with autonomic dysreflexia result directly from sustained, severe peripheral hypertension. This condition is distinct and usually episodic, with the people experiencing remarkably high blood pressure (often with systolic readings over 200 mm. Hg), intense headaches, profuse sweating, bradycardia facial erythema, goosebumps, nasal stuffiness, a "feeling of doom" or apprehension, and blurred vision. An elevation of 40 mm Hg over baseline systolic should be suspicious for dysreflexia. be mindful of the catheter - make sure its not kinked
question
surgeries w biggest risk of autonomic dysreflexia in someone with SCI
answer
Bowel distention - laproscopic surgery can cause abd to be filled with gas. Colonoscopy - air / water. Can be a trigger Cystoscopy and sx that distends bowl = biggest risk procedures for AD
question
things to make note of in preop assessment in someone with CVA/TIA
answer
Make note of: Hemi paralysis Residual weakness Range of motion Consider maintaining blood pressure close to baseline to maintain cerebral perfusion Make sure you know their baseline before surgery!! You don't want to wonder if a stroke happened intraop - you don't want to be blamed for it!
question
surgeries with greatest risk for CVA/TIA
answer
open heart and carotid procedures
question
things to make note of in preop assessment in someone with diabetic neuropathy
answer
Make note of: Numbness/Tingling in extremities preoperatively Has the patient experienced any vision loss? Consider surgical procedure: If extremity has little or no sensation, may not require as much pain management Can procedure be done under MAC?
question
preop/anesthetic considerations for someone with restless leg syndrome
answer
Is this patient a candidate for MAC / IV Sedation? How much relaxation is required for this surgical procedure? How long is the procedure? Will movement interfere with the procedure?
question
what drugs should you avoid in someone with restless leg syndrome
answer
Antiemetic agents with dopamine antagonist or histamine antagonist properties (metoclopramide, prochlorperazine and promethazine) Opioid antagonists (naloxone, naltrexone) Antihistamines that cross the blood-brain barrier (diphenhydramine in particular)
question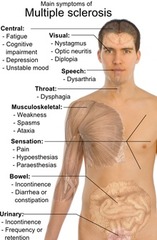
multiple sclerosis
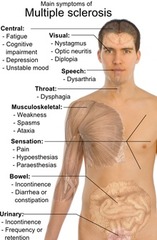
answer
Multiple sclerosis (MS) is a demyelinating disease in which the insulating covers of nerve cells in the brain and spinal cord are damaged. This damage disrupts the ability of parts of the nervous system to communicate, resulting in a range of signs and symptoms, including physical, mental, and sometimes psychiatric problems. Specific symptoms can include double vision, blindness in one eye, muscle weakness, trouble with sensation, or trouble with coordination. MS takes several forms, with new symptoms either occurring in isolated attacks (relapsing forms) or building up over time (progressive forms). Between attacks, symptoms may disappear completely; however, permanent neurological problems often remain, especially as the disease advances. While the cause is not clear, the underlying mechanism is thought to be either destruction by the immune system or failure of the myelin-producing cells. Proposed causes for this include genetics and environmental factors such as being triggered by a viral infection. There is no known cure for multiple sclerosis. Treatments attempt to improve function after an attack and prevent new attacks. administration of high doses of intravenous corticosteroids, such as methylprednisolone, is the usual therapy. eleven disease-modifying medications have been approved by regulatory agencies for relapsing-remitting multiple sclerosis (RRMS). They are interferon beta-1a, interferon beta-1b, glatiramer acetate, mitoxantrone, natalizumab, fingolimod,[61] teriflunomide,[62] dimethyl fumarate,[63] alemtuzumab,[64] daclizumab,[65] and ocrelizumab
question
Parkinson's Disease
answer
Parkinson's disease (PD) is a long-term degenerative disorder of the central nervous system that mainly affects the motor system. The symptoms generally come on slowly over time. Early in the disease, the most obvious are shaking, rigidity, slowness of movement, and difficulty with walking. Thinking and behavioral problems may also occur. Dementia becomes common in the advanced stages of the disease. Depression and anxiety are also common occurring in more than a third of people with PD. Other symptoms include sensory, sleep, and emotional problems. The main motor symptoms are collectively called "parkinsonism", or a "parkinsonian syndrome". The cause of Parkinson's disease is generally unknown, but believed to involve both genetic and environmental factors. Those with a family member affected are more likely to get the disease themselves. There is also an increased risk in people exposed to certain pesticides and among those who have had prior head injuries, while there is a reduced risk in tobacco smokers and those who drink coffee or tea. The motor symptoms of the disease result from the death of cells in the substantia nigra, a region of the midbrain. This results in not enough dopamine in these areas. The reason for this cell death is poorly understood, but involves the build-up of proteins into Lewy bodies in the neurons. There is no cure for Parkinson's disease. Initial treatment is typically with the antiparkinson medication L-DOPA (levodopa), with dopamine agonists being used once levodopa becomes less effective. As the disease progresses and neurons continue to be lost, these medications become less effective while at the same time they produce a complication marked by involuntary writhing movements
question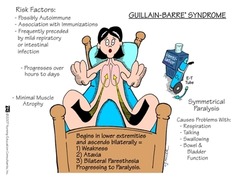
Guillain Barre Syndrome
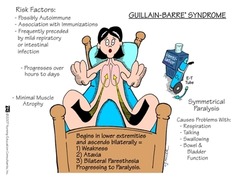
answer
a rapid-onset muscle weakness caused by the immune system damaging the peripheral nervous system. The initial symptoms are typically changes in sensation or pain along with muscle weakness, beginning in the feet and hands. This often spreads to the arms and upper body with both sides being involved. The symptoms develop over hours to a few weeks. During the acute phase, the disorder can be life-threatening with about 15% developing weakness of the breathing muscles requiring mechanical ventilation. Some are affected by changes in the function of the autonomic nervous system, which can lead to dangerous abnormalities in heart rate and blood pressure. The cause is unknown. The underlying mechanism involves an autoimmune disorder in which the body's immune system mistakenly attacks the peripheral nerves and damages their myelin insulation. Sometimes this immune dysfunction is triggered by an infection or, less commonly, surgery or vaccination. In those with severe weakness, prompt treatment with intravenous immunoglobulins or plasmapheresis, together with supportive care, will lead to good recovery in the majority. Recovery may take weeks to years. About a third have some permanent weakness.
question
Cerebral Palsy
answer
Cerebral palsy (CP) is a group of permanent movement disorders that appear in early childhood. Often, symptoms include poor coordination, stiff muscles, weak muscles, and tremors. There may be problems with sensation, vision, hearing, swallowing, and speaking. Often babies with cerebral palsy do not roll over, sit, crawl, or walk as early as other children of their age. Other symptoms include seizures and problems with thinking or reasoning, each of which occurs in about one third of people with CP. While the symptoms may get more noticeable over the first few years of life, the underlying problems do not worsen over time. Cerebral palsy is caused by abnormal development or damage to the parts of the brain that control movement, balance and posture. Most often the problems occur during pregnancy; however, they may also occur during childbirth, or shortly after birth. Often the cause is unknown. Risk factors include preterm birth, being a twin, certain infections during pregnancy such as toxoplasmosis or rubella, exposure to methylmercury during pregnancy, a difficult delivery, and head trauma during the first few years of life, among others. About 2% of cases are believed to be due to an inherited genetic cause. CP is partly preventable through immunization of the mother and efforts to prevent head injuries in children such as through improved safety. There is no cure for CP; however, supportive treatments, medications, and surgery may help many individuals. This may include physical therapy, occupational therapy, and speech therapy. Medications such as diazepam, baclofen, and botulinum toxin may help relax stiff muscles. Surgery may include lengthening muscles and cutting overly active nerves. Often external braces and other assistive technology are helpful. Some affected children can achieve near normal adult lives with appropriate treatment. While alternative medicines are frequently used there is no evidence to support their use.
question
Muscular Dystrophy
answer
Muscular dystrophy (MD) is a group of muscle diseases that results in increasing weakening and breakdown of skeletal muscles over time. The disorders differ in which muscles are primarily affected, the degree of weakness, how fast they worsen, and when symptoms begin. Many people will eventually become unable to walk. Some types are also associated with problems in other organs. due to mutations in genes that are involved in making muscle proteins. This can occur due to either inheriting the defect from one's parents or the mutation occurring during early development. There is no cure for muscular dystrophy. Physical therapy, braces, and corrective surgery may help with some symptoms. Assisted ventilation may be required in those with weakness of breathing muscles. Medications used include steroids to slow muscle degeneration, anticonvulsants to control seizures and some muscle activity, and immunosuppressants to delay damage to dying muscle cells. Outcomes depend on the specific type of disorder.
question
Myasthenia Gravis
answer
Myasthenia gravis (MG) is a long-term neuromuscular disease that leads to varying degrees of skeletal muscle weakness. The most commonly affected muscles are those of the eyes, face, and swallowing. It can result in double vision, drooping eyelids, trouble talking, and trouble walking. Onset can be sudden. Those affected often have a large thymus gland or develop a thymoma. Myasthenia gravis is an autoimmune disease which results from antibodies that block or destroy nicotinic acetylcholine receptors at the junction between the nerve and muscle. This prevents nerve impulses from triggering muscle contractions. Rarely, an inherited genetic defect in the neuromuscular junction results in a similar condition known as congenital myasthenia. Myasthenia gravis is generally treated with medications known as acetylcholinesterase inhibitors such as neostigmine and pyridostigmine. Immunosuppressants, such as prednisone or azathioprine, may also be used. The surgical removal of the thymus gland may improve symptoms in certain cases. Plasmapheresis and high dose intravenous immunoglobulin may be used during sudden flares of the condition. If the breathing muscles become significantly weak, mechanical ventilation may be required
question
anesthetic considerations/preop assessment for those pts with neuromuscular diseases
answer
How advanced is the disease? Make note of preoperative deficits Is the patient current on his/her medications? Increased risk for Succinylcholine induced hyperkalemia Delayed recovery from muscle relaxants Increased sensitivity to respiratory depressant affects of narcotics Consider regional anesthesia Consider need for postop mechanical ventilation
question
anesthetic considerations/preop assessment for those pts with cognitive disorders
answer
How advanced is their condition? Are they current on their medications? Consider anesthesia drug interactions MAOI - avoid indirect, careful with direct sympathomimetics SSRI - avoid tramadol, Demerol TCA - avoid indirect sympathomimetics What is their baseline mental state? Modify narcotic/hypnotic anesthetic dosage: How much does the patient need? How long is this procedure? Will this surgery/procedure cause significant levels of pain? Intraoperative pain vs. Postoperative pain
question
paresthesia
answer
Sudden nerve pain due to direct contact with nerve root/bundle Immediately remove/redirect the needle Less incidence of paresthesia with use of ultrasound
question
local anesthetic toxicity causes
answer
Systemic toxicity of local anesthetics can occur after administration of an excessive dose, with rapid absorption, or because of an accidental intravenous injection CAUSES drug overdose IV injection rapid absorption from hight vascular area accumulation of multiple injections or infusion
question
early signs of local anesthetic toxicity
answer
Tongue numbness Metallic taste in mouth Lightheadedness Dizziness Ringing in ears Disorientation/drowsiness
question
late signs of local anesthesia toxicity
answer
muscle twitching convulsions unconscioiusness resp/cardiac arrest
question
local anesthetic toxicity treatment
answer
airway management seizure suppression management of arrhythmias lipid emulsion 20%
question
sympathectomy
answer
The sympathectomy produced by spinal anesthesia induces hemodynamic changes. The block height determines the extent of sympathetic blockade, which determines the amount of change in cardiovascular parameters. Hypotension and bradycardia are the most common side effects seen with sympathetic denervation. Nausea is often the first indication Risk factors associated with hypotension include hypovolemia, preoperative hypertension, high sensory block height, age older than 40 years, obesity, combined general and spinal anesthesia, and addition of phenylephrine to the local anesthetic. Chronic alcohol consumption, history of hypertension, elevated BMI, high level of sensory block height, and urgency of surgery all increase the likelihood of hypotension after spinal anesthesia. sympathectomy can lead to high and complete spinal
question
high spinal
answer
severe hypotension agitation danger!
question
complete spinal
answer
resp. collapse cardiac arrest loss of consciousness MEDICAL EMERGENCY!
question
how can you tell if your pt is "getting light" under anesthesia?
answer
Tearing/Grimacing Sweating Movement Increase in vital signs/respiratory effort
question
which surgical cases have increased incidence of awareness? why?
answer
Emergency C-Section with GA - less meds because of the baby Trauma - unstable hemodynamics: do not use gas or sedatives!! Ketamine and scopolamine Cardiopulmonary Bypass - pt is not inhaling the anesthetic gas through the machine. The perfusionist controls gas during that. Time lapse can cause awareness
question
intraoperative neuromusclar blockade considerations
answer
How much muscle relaxation is required for this procedure? Can the surgeon inject local? Is the plan for the patient to remain intubated?
question
NMB reversal/recovery considerations
answer
Twitches? Spontaneous breathing Head Lift Swallowing / Stick out tongue Strong cough / gag reflex
question
this nerve is at increased risk for injury in the lithotomy position
answer
peroneal nerve injury over extension/abduction of the hips
question
BP considerations for the beach chair position
answer
Keep cuff on upper extremity 20cm rise = 15mmHg drop in MAP Example: Ear = 50mmHg Arm = 65mmHg Leg = 80mmHg
question
this nerve is at increased risk for injury in the prone position
answer
optic nerve
question
intraoperative neuro monitoring
answer
Bispectral Index (BIS) Somatosensory Evoked Potentials (SSEP) Cerebral Oximetry NIM Endotracheal Tube
question
bispectral index (BIS)

answer
Bispectral index (BIS) is one of several technologies used to monitor depth of anesthesia. Titrating anesthetic agents to a specific bispectral index during general anesthesia in adults (and children over 1 year old) allows the anesthetist to adjust the amount of anesthetic agent to the needs of the patient, possibly resulting in a more rapid emergence from anesthesia. Use of the BIS monitor could reduce the incidence of intraoperative awareness during anaesthesia. The BIS is an electroencephalogram-derived multivariant scale that correlates with the metabolic rate of glucose. Both loss of consciousness and awakening from anesthesia are correlated with this scale. The efficacy of BIS index monitoring is not without controversy.
question
Somatosensory Evoked Potentials (SSEP)
answer
Somatosensory evoked potential (SEPs or SSEPs) tests measure the electrical activity of the brain that results from the stimulation of touch. SEP components include a series of positive and negative deflections that can be elicited by virtually any sensory stimuli. For example, SEPs can be obtained in response to a brief mechanical impact on the fingertip or to air puffs. However, SEPs are most commonly elicited by bipolar trancutaneous electrical stimulation applied on the skin over the trajectory of peripheral nerves of the upper limb (e.g., the median nerve) or lower limb (e.g., the posterior tibial nerve), and then recorded from the scalp. In the recent decade, the clinical usefulness of SEPs entered the operating room, allowing the intraoperative monitoring of the CNS and, thus, safeguarding CNS structures during high risk surgeries. Continuous SEP monitoring can warn a surgeon and prompt intervention before impairment becomes permanent. Testing with median nerve SEPs is used to identify the sensory and motor cortex during craniotomies and in monitoring surgery at the midcervical or upper cervical levels. Posterior tibial nerve SEP monitoring is widely used for monitoring the spinal cord during scoliosis procedures and other surgical interventions in which the spinal cord is at risk for damage. Recording of far field intracranially generated peaks can facilitate monitoring even when the primary cortical peaks are impaired due to anesthetic agents. Over time, SEP testing and monitoring in surgery have become standard techniques widely used to reduce risk of postoperative neurologic problems for the patient. Continuous SEP monitoring can warn a surgeon about potential spinal cord damage, which can prompt intervention before impairment becomes permanent. Overall, SEPs can meet a variety of specific clinical objectives, including: to establish objective evidence of abnormality when signs or symptoms are equivocal; to look for clinically silent lesions; to define an anatomical level of impairment along a pathway; to provide evidence about the general category of the pathology; to monitor objective changes in the patient's status over time.



