Treatment of congestive cardiac failure – Flashcards
Unlock all answers in this set
Unlock answersquestion
Chronotropy
answer
Heart RATE
question
Inotropy
answer
Myocardial CONTRACTILITY
question
Dromotropy
answer
Conduction SPEED
question
Lusitropy
answer
Rate of RELAXATION after contraction
question
Preload vs Afterload
answer
Preload: Ventricular end DIASTOLIC volume (stretch after blood fills ventricles) Afterload: The amount of resistance the heart must overcome to open the aortic valve and push the blood volume out into the systemic circulation
question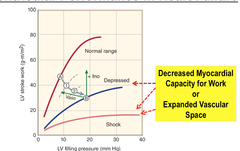
Hear failure
answer
Cardiac pump DYSFUNCTION-> congestion + DECREASED perfusion Will have: -Dyspnea -Orthopnea -Fatigue -Rales -JVD -Pitting edema Exercise-> Mycoardial oxygen demand increases-> inadequate compensation-> Heart Failure -Graph shows Ventricular Performance in Heart Failure
question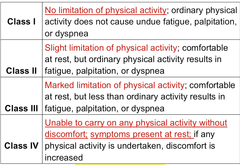
HF classification
answer
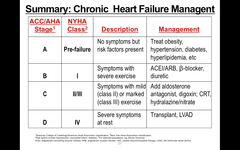
Class I (A): NO limitation of physical activity (risk factors are present) Class II (B): Slight limitation of physical activity (severe exercise) Class III (C): MARKED limitation of physical activity Class IV (D): Unable to carry on any physical activity WITHOUT discomfort-> symptoms present even at rest (Severe symptoms at rest!)
question
Chronic Cardiac Failure (CCF)
answer
Heart failure develops and progresses SLOWLY -Edema and congestion are hallmark symptoms Goal of Therapy: IMPROVE symptoms and PREVENT progression of CHF
question
Acute Heart Failure (ACF)
answer
-May develop suddenly during CCF->SHOCK!!! -Usually due to myocardial damage-> infarction -Goal of Therapy in ACF: Re-establish adequate tissue perfusion and O2 delivery to end organs -ENSURE airway, breathing, and circulation (ABC)!
question
Drugs to treat CCF
answer
*Diuretics*: DECREASE congestion -Thiazide diuretics -Loop diuretics -Natriuretic peptides: *Nesiritide* -Vasodilators (dilate arteries and veins): ACEI -Angiotensin receptor blockers (ARBs) -Nitrodilators -Direct-acting arterial dilators -Natriuretic peptides
question
Drugs used to treat heart failure
answer
Drug selection depends on patient's initial clinical state and responsiveness to initial therapy (CHF) ABCDE -ACE inhibitors -?-blockers: mild-to-moderate HF only -Cardiac Glycosides -Diuretic agents -Eplerenone/ Spironolactone: Aldosterone inhibitors Additional Agents for severe or acutely decompensated HF: -Vasodilators -Parenteral inotropic agents DO NOT use CCBs!
question
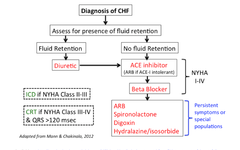
Choice of Agent based on Degree of HF
answer
ACE Inhibitor Beta blocker Cardiac glycoside: DIGOXIN Diuretic --- Decrease mortality with Ace inhibitors, beta blockers, and spironolactone
question
Vasodilators for Heart Failure
answer
-*ACEIs and ARBs are FIRST line agents* -*Direct Vasodilators*: Isosorbide dinitrate, nitroprusside, hydralazine, amlodipine, and prazosin ;Used specially in patients who cannot tolerate ACE inhibitors -Use limited by high incidence of *side effects in HF* *All can help REDUCE symptoms of heart failure by DECREASING myocardial oxygen demand*
question
Diuretics Used in Heart Failure
answer
INCREASED elimination of edematous fluid improve tissue perfusion and pulmonary function -DECREASE fluid volume and relieve symptoms of heart failure -Produce few side effects-; often used in combination with other HF drugs to REDUCE patient's symptoms -Potent diuretics such as *furosemide* (loop diuretic) are particularly valuable in treating acute HF ---- Aldosterone inhibitor: *Spironolactone and Eplerenone* -*K+-sparing diuretics* -> DECREASE hypokalemia caused by thiazides and loop diuretics
question
Spironolactone (Indications)
answer
Treatment of CHF -Spironolactone administration in patients with severe heart failure improved symptoms, decreasing mortality by 27%, and also DECREASING rate of hospitalization --- Other uses: -Primary hyperaldosteronism -Edematous conditions -Hypokalemia -Essential HTN
question
Spironolactone (Contraindications)
answer
-HYPERkalemia -Patients with significant *renal impairment*
question
ACEIs (& ARBs) for Heart Failure
answer
ACEI: (-prils) Captopril, Enalapril, Lisinopril, and Others -1st-line drugs in the treatment of HF ARBs: (-sartan) Losartan, Candesartan, and Others) may be used when ACEIs NOT tolerated! Improve heart failure by DECREASING peripheral edema and INCREASING cardiac output -Effective and have relatively LOW potential for serious adverse effects! -Decrease peripheral edema and increase CO
question
Beta Blockers
answer
*Metoprolol, Propranolol, Carvedilol* Use with caution in Heart Failure -Nearly always used in combination with other drugs in HF -Recommended for use in patients with *LV ejection fraction <35%* and NYHA class II or III symptoms in conjunction with an *ACEI or ARB and diuretics*
question
Beta Blockers (effects on HF)
answer
DECREASE myocardial contractility, heart rate, and blood pressure ->DECREASES symptoms of HF -Start at very LOW doses (~1/10 of final target and titrate cautiously upwards)
question
Digoxin and cardiac Glycosides

answer
*Cardiac glycosides: DIGITOXIN and DIGOXIN* Selective inhibition of the *plasma membrane Na+ pump* -Cardiac myocytes extrude LESS Na+ causing RISE in INTRAcellular Na+ concentration -ELEVATED intracellular Na+ alters the equilibrium of the Na+/Ca2+ exchanger ->Decreased Ca2+ efflux due to gradient for Na+ entry, while Ca2+ INFLUX is INCREASED due to INCREASED gradient for Na+ efflux! -Positive INOTOROPIC -Vagal stimulation-> Decreases sympathetic activation and HR --- Slide shows that blockage of 3Na+/2K+ exchange causes accumulation of intracellular sodium-> REpolarization is INHIBITED!
question
Digoxin Uses
answer
HF -Increases inotropy -INCREASES Ejection Fraction -DECREASES preload -Decreases pulmonary congestion/edema Arrhythmias -DECREASES AV nodal conduction-> PNS effect: Prolongs the effective refractory period -DECREASES ventricular rate in *atrial flutter and fibrillation* (SA node depression) --- -Sinus node: decreases rate -Atrial muscle: Decreases refractory period -AV node: INCREASES refractory period + decreases conduction velocity -Purkinje system/Ventricular muscle: SLIGHT DECREASE refractory period -Electrocardiogram: INCREASED PR Interval, DECREASED QT interval
question
Digoxin (Adverse effects)
answer
-*Narrow Therapeutic Index: Requires monitoring!* Extracardiac (symptoms similar to the flu): -Anorexia -NVD -Abdominal pain -Blurred vision >Abnormal color perception: Yellow or green spots -Anxiety -Nightmares -Hallucinations -Delirium -Fatigue -Muscle weakness -Gynecomastia -Toxicity Management Digibind-> Digoxin immune FAB ==== Toxic doses: -Can lead to atrial muscle having arrhythmias -Tachycardia, fibrillation, extrasystoles
question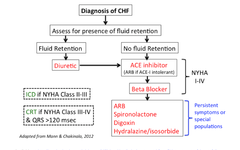
Digoxin (Contraindications)
answer
-*Ventricular tachycardia* -*Heart block* -*Hypokalemia* -Hypercalcemia -Renal impairment (*Digoxin removed by KIDNEYS*) -Do NOT give with verapamil, amiodarone, quinidine, diuretics: Displace from binding site and decrease CLEARANCE -Treat overdose with DiGiBind: Anti-Digoxin Fab fragments
question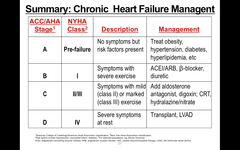
Management of CHF: Summary
answer
REMEMBER: ABCDE -ACE inhibitors -?-blockers: mild-to-moderate HF only -Cardiac Glycosides -Diuretic agents -Eplerenone/ Spironolactone: Aldosterone inhibitors
question
Acute Heart failure (AHF): management
answer
Beta adrenergic agonists: *isoproterenol* -Beta 1 agonist: *Dobutamine* -*Dopamine* (low and medium doses) -*Phosphodiesterase-III Inhibitors (PDEI)*: Milrinone, Inamrinone, Theophylline, Calcium chloride -*Pressor Agents*: Agents to restore tissue perfusion >Epinephrine/ Norepinephrine >HIGH dose Dopamine
question
Beta-Adrenergic Receptor Agonists (Indications)
answer
ACUTE conditions where there is LOW cardiac output (CO)-> *cardiogenic shock*
question
Beta-Adrenergic Receptor Agonists (In Congestive Heart Failure)
answer
-Have had LIMITED use in chronic management of CHF -BETA adrenergic receptor agonist efficacy limited by REDUCTION in receptor numbers and Desensitization: a significant LOSS of Beta-1 receptors (~ 50%) occurs
question
Dobutamine
answer
Racemic mixture that binds to and activates ?-1 and ?-2 adrenoceptors -Positive inotropic action mediated by ?-receptor activation predominates -Does NOT activate *dopamine receptors* and therefore does NOT increase renal blood flow Mechanism of action: LOW doses *Beta-1 selective adrenergic agonist * -*INCREASES CONTRACTILITY (inotropic) WITHOUT substantially increasing either HR or peripheral resistance* -LESS arrhythmogenic and LESS tachycardia than endogenous catecholamines or *isoproterenol*
question
Dobutamine (Indications)
answer
SHORT-term *inotropic* (elevate heart contractility) support in patients with cardiac decompensation due to depressed contractility
question
Dobutamine (Adverse Effects)
answer
-INCREASES systolic blood pressure by 10-20 mm and heart rate by ~5-15 beats/minute in most patients *Increased SBP and HR*
question
Dopamine
answer
DOSE DEPENDENT Low Doses: Selectively activate D1 receptors in several vascular beds (kidneys)-> VASODILATION-> INCREASES renal blood flow (ex: in the TREATMENT OF SHOCK) Intermediate Doses: ACTIVATE cardiac BETA-1 receptors -Improve myocardial contractility (* +ve inotropic effect*) -Produces LESS of an INCREASE in heart rate compared to isoproterenol! --- Low and medium is therapeutic; high will cause vasoconstriction (alpha agonist)-> NOT wanted
question
Dopamine (mechanism)
answer
-Dilates renal arteries achieves *better renal perfusion than dobutamine or isoproterenol* -*Corrects hemodynamic disturbances* in shock due to *myocardial infarction, trauma, septicemia, open-heart surgery, and renal failure * *Tolerance may develop with continued infusion!*
question
Dopamine (Indications)
answer
In Chronic cardiac decompensation (Congestive HF) -> Corrects hemodynamic IMBALANCES in SHOCK-> MI, trauma, septicemia, open-heart surgery, *renal failure*, etc
question
Dopamine (Side effects)
answer
-Cardiac arrhythmias -Dyspnea -Nausea -Vomiting -Headache
question
Dopamine (contraindications)
answer
Contraindicated in: -Pheochromocytoma -Uncorrected tachyarrhythmias -Ventricular fibrillation
question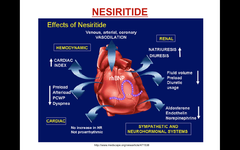
Nesiritide
answer
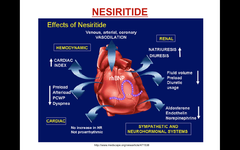
Recombinant *B-type natriuretic peptide* -Arterial and venous VASODILATOR with modest diuretic and natriuretic properties -Used to treat acutely *decompensated congestive heart failure with dyspnea at rest* -Normally produced by the ventricular myocardium
question
Nesiritide (Mechanism of action)
answer
INCREASE cardiac output by VASODILATION without increasing heart rate or oxygen consumption -Counterregulation of the renin-angiotensin-aldoesterone system via stimulation of cGMP-> smooth muscle relaxation-> Promotes vasodilation, natriuresis, and diuresis
question
Ivabradine
answer
In patients on maximally tolerated -blocker therapy >HR or in whom Beta-blockers are contraindicated, or resting HR ?70 & (LVEF ? 35%) >For anti-anginal (chronic stable angina), anti-ischemic, and symptomatic CHF. Mechanism: Selective blocker of If (funny channels are blocked)-> DECREASED pacemaker activity-> HR only decreases Side effects: -Inappropriate sinus tachycardia is an uncommon disorder characterized by multiple symptoms, including palpitations, dizziness, orthostatic intolerance, and elevated heart rates. -Visual disturbances
question
Milrinone and Inamrinone
answer
-NONE drugs *Phosphodiesterase III inhibitors* used for the SHORT-term management of HF -INCREASE force of contraction (inotropic) and cause VASODILATION -Only given IV and can produce potentially SERIOUS adverse effects -Used for a SHORT time when HF refractory to other drugs
question
Milrinone and Inamrinone (side effects)
answer
IV ONLY and short time use Clinically significant *thrombocytopenia* occurs in ~10% of patients receiving inamrinone (rare with milrinone)
question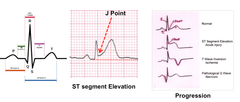
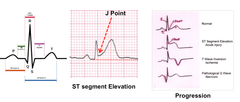
ACUTE HEART FAILURE: EKG manifestations of Damage to the myocardium
answer
*ST Segment elevation*: Myocardial damage may cause elevation of S portion and T wave elevates( can be close or even higher than R wave) >Typically with MI (ST elevated MI= STMI) >Starts in ventricles and moves outwards (affects electrical activation) *INVERSION of T wave*: Appears later on-> ISCHEMIA *Q waves can go further down*= EXAGGERATION>DEAD tissue NOT conducting anymore in the ventricles (NECROSIS)-> rest may look normal
question
Possible Consequences of MI: Types of shock
answer
-Hypovolemic Shock -Cardiogenic Shock -Distributive Shock -Neurogenic Shock -Septic shock >Thirst and dry mouth >Low blood sugar >Fever
question
Possible Consequences of MI: Anaphylaxis
answer
Hives and swelling of the face and throat
question
Possible Consequences of MI: Signs and symptoms
answer
-Rapid, weak, or ABSENT pulse and irregular heart rate -Cool, clammy skin -Rapid and shallow breathing -Decreased BP and urine output -Chest pain and nausea -Confusion, anxiety, and light headedness -DILATED pupils or lackluster eyes
question
Cardiogenic Shock
answer
Cardiac dysfunction persistent hypotension (SBP <80 to 90 mm Hg or MAP 30 mmHg lower than baseline) with severely cardiac index (<1.8 L/ min per m2 without support or Patients most commonly succumb to MULTI-organ dysfunction due to ongoing ischemia -- Cardiogenic shock may follow MI, acute decompensated heart failure, and low CO states after cardiac surgery
question
Cardiogenic shock: Causes and pathogenesis
answer
-Acute myocardial infarction: usually ST elevation myocardial infarction + Left ventricular failure -Mechanical complications: Acute mitral regurgitation or rupture of either the ventricular septal or free walls -Acute, severe left or right ventricular dysfunction may lead to cardiogenic shock
question
Cardiogenic shock: General measures
answer
-Ventilation support (O2) to correct hypoxemia and acidosis -Optimize intravascular volume -Sodium bicarbonate only for severe metabolic acidosis (arterial pH less than 7.10 to 7.15) -ASPIRIN -*IV Heparin (UFH)* -Possible glycoprotein IIb/IIIa inhibitor with NSTEMI -Insertion of pulmonary artery catheter
question
Cardiogenic shock: Treatment
answer
Shock is a medical emergency -Goal find and treat the cause of shock -Supportive therapy to maintain tissue perfusion and oxygenation -Drugs to INCREASE blood pressure and improve heart function: *-Dobutamine -Dopamine -Epinephrine -Norepinephrine -Milrinone and amrinone*



