Stanford Plastic Surgery Oral Board Review – Hand – Flashcards
Unlock all answers in this set
Unlock answersquestion
Hand Surgery Review Vincent R Hentz MD What are the likely problems you should be expecting for hand?
answer
Simple congenital Mutilated hand / Replantation Nerve injury Still joints / Dupuytrens Flexor / Extensor tendon injuries Simple tendon transfers
question
What cases should you definitely prepare for?
answer
Mutilated hand Syndactyly Thumb reconstruction Peripheral nerve injury Stiff hand or finger Dorsal hand wound Replantation salvage Hand burn Dupuytren's contracture Acute flexor tendon injury Staged flexor tendon injury Easy tendon transfers
question
What are the principles of hand surgery that you need to remember?
answer
Know the anatomy Perform the pertinent examination Get radiographs Remember the hand emergencies (devascularized digits / hand infection / compartment syndrome) Priorities (revascularization / bone stability / soft tissue coverage)
question
What are the remaining principles?
answer
Plan the different stages of the reconstruction Stage operations based on post-operative therapy "Test-drive" the patient with hand therapy Resist the temptation to amputate Rigid fixation and early motion Beware of complications (stiffness / RSD)
question
What are the general considerations to take into account with congenital hand timing and what should you beware of?
answer
Timing of surgery - anesthetic risk versus improved outcome with early use of reconstructed hand Most surgeries start at 6 months and are completed by 2 years Beware of injuring growth plates / abnormal growth / patient and family compliance (wound / splints / therapy)
question
What are the seven classifications of congenital hand abnormalities by the IFSSH (International federation of societies for the surgery of the hand)?
answer
1. Failure of formation (transverse arrest) 2. Failure of differentiation (syndactyly) 3. Duplication (polydactyly) 4. Overgrowth (macrodactyly) 5. Undergrowth (brachydactyly) 6. Constructed band syndrome 7. Generalized skeletal abnormalities (Madelung's deformity)
question
What are the different type of terminology used for syndactyly?
answer
Simple (soft tissue) Complex (including bone) Complete (to fingertips) Incomplete (short of fingertips)
question
When it comes to syndactyly planning - what are the key steps?
answer
Diagnose the problem (need radiographs) Rule out associated problems (Poland syndrome) Timing - 6 months Stage reconstruction - Release border digits to prevent deviation - One side of finger at an operation
question
What should you know for syndactyly technique?
answer
Know how to draw incisions Reserve flap for the web space Address the lateral nail fold FTSG Revision surgery (Re-release / osteotomy)
question
When might you perform surgery earlier than 6 months?
answer
If there are distal boney unions
question
What are the three types of duplications (polydactyly)?
answer
Pre-axial Post-axial Central (usually with syndactyly)
question
What is the name of the thumb duplication classification - which is the most common - and what's the general difference between odd and even numbers?
answer
Wassel classification Most common is #4 Odd #s are partial duplication Even #s are complete duplication
question
Which element is typically excised in thumb duplication and why?
answer
Usually radial is the excised element Because you want to preserve the ulnar collateral ligament (reinforce ulnar)
question
Can you combine two elements into one?
answer
Yes
question
What do you do after removal of a radial element postoperatively?
answer
Large cast Therapy for webspace (splints) Observe for web space creep Reuse containing scars
question
What are some of the problems you might run into postoperatively?
answer
Joint instability caused by tendon imbalance versus ligament instability causing progressive instability
question
What can you do about this?
answer
Capsulloraphy Chondrodesis Arthrodesis Osteotomy
question
When it comes to radial longitudinal deficiency (aka radial club hand) what is the pathoanatomy of the humerus / radius / ulna / radial carpus / and thumb?
answer
Humerus - short / hypoplastic lateral condyle Radius - partial or complete absence Ulna - short and bowed Radial carpus - absent / hypoplastic / coalitions Thumb - hypoplastic / absent
question
What are some of the syndromes you should rule out when it comes to radial longitudinal deficiency?
answer
VACTERL association (vertebral abnormalities / anal atresia / cardiac abnormalities / TE fistula Radial dysplasia and renal abnormalities / lower limb abnormalities) Holt-Oram syndrome (cardiac ASD / bilateral radial dysplasia) Fanconi anemia (subclinical progressive pancytopenia and radial dysplasia)
question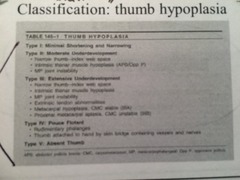
What are the five different types of thumb hypoplasia and what is the name of this classification system?
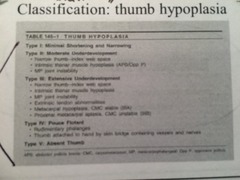
answer
Blauth Classification of thumb hypoplasia
question
What are the surgical goals of treating thumb hypoplasia?
answer
Improve appearance Improve function (stabilize wrist improved mechanical advantage of finger flexors / "lengthen" arm / Thumb reconstruction for grasp of large objects)
question
What are the key components of the overall plan to treat thumb hypoplasia?
answer
Perinatal stretching of wrist followed by early surgery Wrist centralization (3 months to 1 year) Thumb reconstruction (pollicization) 1 year to 2 years
question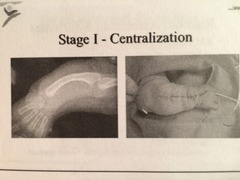
What does wrist centralization look like? What is the thumb surgery for type I through V thumb hypoplasia?,
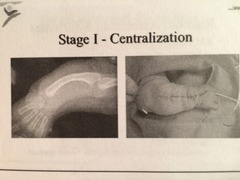
answer
Type I - none Type II and possible Type III - thumb reconstruction Pollicization - Tyles IIIB, IV, and V
question
Why pollicization for IIIB, IV, and V?
answer
No platform
question
What are your priorities with a mutilated hand injury?
answer
ABCs Check perfusion (angiogram) Irrigation and exploration Release compartments Stabilize bone (external fixation) Definitive debridement Soft tissue coverage (immediate or delayed)
question
How do you do a cross finger flap?
answer
- crossed finger flaps can be used to cover finger tip injuries w/ excessive loss of volar pulp tissue - rectangular flap is raised from 3 sides of the dorsal surface of middle phalanx of the adjacent finger typically the flap is based on the lateral side of the adjacent digit but the flap can also be based proximally (in order to raise a flap from the thumb to the radial side of the index finger) - flap is harvested thru the subcutaneous tissue and down to (but not thru the underlying epitenon) - by cutting Cleland's ligament, the flap will extend 20% longer - flap is swung outward on its hinge and is sutured in place - full thickness graft is sutured to the hinge of the primary defect- - flap is divided within two weeks, in order to avoid finger stiffness
question
What's a good flap for covering the volar surface of the thumb?
answer
First dorsal metacarpal artery flap
question
What is the workhorse flap for hand coverage prior to the advent of microsurgery and what vessel is it based on and where does the vessel run?
answer
Groin flap Based on superficial femoral circumflex artery (around 2cm below and parallel to the inhuinal ligament) Vessel runs deep to thigh fascia and pieces into the subcutanoue tissue at the medial border of the sartorius muscle
question
When can this flap be safely divided?
answer
3 weeks
question
What's another common flap used for coverage of a volar finger tip and what is it'd downside?
answer
Thenar flap Infrequently used because of joint stiffness
question
What are the chronic effects of compartment syndrome of the upper extremity?
answer
Volkmann's ischemic contracture with necrotic and fibrous tissue
question
What is the number one cause of compartment syndrome of the upper extremity?
answer
Fractures (humeral supracondylar / distal radius)
question
What are the classic signs of compartment syndrome?
answer
Pain out of proportion to exam Pain with passive extension Diminished sensation Tenseness of involved compartment
question
How do you measure the compartment pressures?
answer
18 gauge angiocath and IV tubing Hook up to pressure monitor Fill IV tubing with saline Place into compartment (subfascial) and flush the line
question
What is a normal intracompartmental pressure and when should you do a fasciotomy?
answer
Normal compartment pressure is 0-8mm Hg Fasciotomy >30 mm Hg
question
What should you do when in doubt when dealing with question of compartment syndrome?
answer
When in doubt - open the fascia
question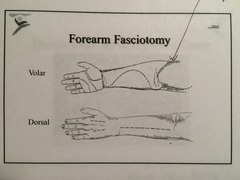
When doing a fasciotomy - what are you releasing and what do you do down the line?
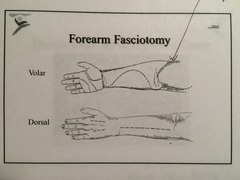
answer
Release skin and fascia Incise each muscle belly individually Release the transverse carpal ligament and lacertus fibrosis Secondary closure versus skin grafting
question
What are the medical treatments for myoglobinuria?
answer
Since it leads to renal failure - must hydrate to maintain high UOP Mannitol diuresis Alkalinize urine
question
What should you try to keep covered when you perform these incision?
answer
The median nerve
question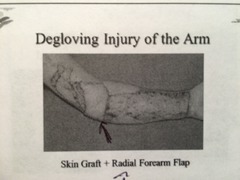
What are you trying to do with this reconstruction?
answer
Trying to prevent elbow contracture
question
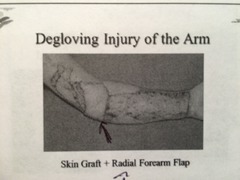
What's a good way of reconstructing this dorsal hand injury?
answer
Reversed radial forearm flap
question
What would be the next step in this case?
answer
Staged tendon grafting
question
How do you harvest the plantaris tendon?
answer
Vertical incision is made just anterior the medial aspect of the Achilles starting at the insertion and proceeding proximally - the tendon is identified and bluntly dissected anterior to the Achilles tendon and divided at its insertion. Tendon stripper is advanced over the tendon which will divided the tendon once it gets to the muscle belly of the plantaris. Carefully palpate after this to make sure you don't get a compartment syndrome.
question
What can you use for bone reconstruction after thumb avulsion injury?
answer
Iliac crest bone graft
question
What do you do with this mutilated arm?
answer
Debride Shunt Provisional stabilization (ex fix) Revascularize Soft tissue
question
What's neuropraxia?
answer
Sunderland first degree nerve injury Compression or stretch lead to a conduction block Axons are intact and without degeneration Both motor and sensory loss
question
How long does neuropraxia last?
answer
Lasts weeks to months - resolves spontaneously
question
What is axonotmesis and how does it recover?
answer
Sunderland's 2nd / 3rd / and 4th degree nerve injury From a crush or traction injury where axons are disrupted and undergo Wallerian degeneration Supporting tubes are in continuity though Axonal regeneration occurs through intact pathways allows functional recovery
question
What is neurotmesis and how do you fix it?
answer
Sunderland 5th degree injury Completely transected nerve Endoneural and perineural elements are not in continuity Surgical repair is required to make axonal regeneration possible
question
What are the critical issues to examine when evaluating a nerve laceration?
answer
Age Level of injury Mechanisms of injury Time of injury Condition of the wound Nerve gap
question
When it comes to denervation and reinnervation what is your goal in terms of getting sensory nerves up and running again?
answer
Sensory end organs may survive years of denervation The goal is to provide protective sensation after one year
question
When do you ideally want to reinnervate motor nerves and why?
answer
Motor end plates die by 3 months Ideal reinnervation before 3 months Functional reinnervation can be expected up to one year No reinnervation can be expected after 3 years
question
When should you do a primary nerve repair?
answer
Primary repair if: Sharp transection Minimal contamination Viable bed and cover Absence of associated injuries Good equipment and trained staff Suitable operative candidates
question
How are you going to repair your nerve?
answer
Epineurial or group fascicular (attempt to repair intraneuronal topography)
question
When would you use a interposition nerve graft?
answer
If a tension free repair is not possible
question
When do transected axons begin to sprout after injury?
answer
6 hours after injury
question
How quickly do axons regenerate?
answer
1mm/day
question
What are some potential nerve graft donors?
answer
Sural nerve Lateral antebrachial nerve Medial antebrachial nerve Posterior interosseous nerve Spare parts nerves
question
What is a reasonable goal for functional recovery with digital nerve repair?
answer
75% of patient under 20 should achieve 2pd<6mm 25-50% of adults should achieve 2pd<6mm
question
Patient has a digital nerve laceration - how do you diagnose it and how do you treat it?
answer
Examine deficit Check two point discrimination Repair without tension Nerve graft sources PIN or vein
question
How do you harvest a PIN?
answer
Distal wrist on dorsal surface atop the interosseous membrane next to anterior interosseous artery
question
What are some of the methods used to decrease the size of the nerve graft in an ulnar nerve laceration?
answer
Mobilization and transposition
question
Where should a nerve end of a neuroma be buried?
answer
In muscle or bone
question
What are normal - bands or cords (in Dupuytren's contracture)?
answer
Bands are normal Cords are abnormal
question
What cords appear at the MCP joint?
answer
Pretendinous cord Natatory cord
question
What cords appear at the PIP joint?
answer
Central cord Spiral cord Lateral cord Retrovascular cord
question
What are the components of the spiral cord?
answer
Spiral band Lateral digital sheet Pretendinous band Grayson's ligament
question
What is the significance of the Spiral cord?
answer
Displaces the nerve volarly and causes a PIP contracture
question
What are indications for surgery on a patient with Dupuytrens?
answer
>30 degrees of MCP joint flexion contracture Any PIP joint flexion contracture Adduction contracture Restricts normal work or activity
question
Should you operate on pain associated with Dupuytrens?
answer
No
question
What are the surgical procedures?
answer
All through brunner incisions Fasciotomy - incise the cord Local fasciectomy - excise a short segment of the cord Regional fasciectomy - excise all diseased fascia Extensive fasciectomy - excise diseased and surrounding normal fascia Dermatofasciectomy - excise diseased fascia and overlying skin
question
What are the technical issues with surgery for Dupuytrens?
answer
Design incisions carefully Elevate skin flaps off diseased fascia Find nerves and vessels proximally and protect Excise all diseased fascia Meticulous hemostasis Skin rearrangement versus skin grafting
question
How should you be cautious regarding PIP joint release?
answer
May be necessary in recurrent cases But do not sacrifice strong flexion (grip) for full finger extension
question
What are some of the ways you can close the wound after fasciectomy for Dupuytrens?
answer
Z-plasty tissue rearrangement Skin graft Healing by secondary intention
question
What are the surgical complications of surgical treatment of Dupuytren's contracture?
answer
Hematoma Skin loss Infection Joint stiffness Nerve injury Arterial ischemia RSD
question
What will you do for postop therapy after Dupuytren's surgery?
answer
Splint with fingers in extension Early active and passive motion Night extension splinting
question
What is a reasonable approach to a spastic contracture?
answer
Release tight volar structures Flexor origin slide Tendon step lengthening Supeficialis to profundus transfer Transect flexor tendons Or Shorten the arm with a proximal row carpectomy
question
When you're presented with a PIP contracture - what structures should you be thinking about when it comes to structures that limit PIP Extension?
answer
Volar skin Fascia Tendon sheath Flexor tendons Volar plate (check-rein ligaments) Accessory and proper collateral ligaments Bony block
question
What are some of the structures that might limit PIP flexion?
answer
Dorsal skin Extensor mechanism Interosseous muscle / tendon Collateral ligaments Volar plate (check rein ligaments) Bony Block



