pancreatitis and pancreatic cancer – Flashcards
Unlock all answers in this set
Unlock answersquestion
acute pancreatitis
answer
Acute inflammatory process that has the potential to become a systemic disease with involvement of peripancreatic tissues and remote organs
question
acute pancreatitis epidemiology
answer
-210,000 new US cases annually, increasing incidence -20 % will have severe acute pancreatitis (necrosis) -5 % overall mortality
question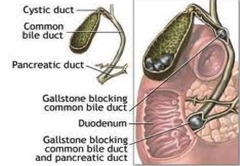
obstructive causes of acute pancreatitis
answer
gallstones (45%) pancreas divisum tumor choledochocoele worms post ERCP
question
toxic causes of acute pancreatitis
answer
EtOH (35 %) aminosalicylates flagyl, sulfa choledochocoele pentamidine, DDI azathioprine
question
acute pancreatitis diagnosis
answer
1. clinical: -pain -nausea -vomiting 2. Laboratory: -Amylase/Lipase > 3 times ULN 3. Imaging: CT
question
amylase
answer
3x ULN = 90 % specific Low sensitivity, can be wnl in hypertrig
question
lipase
answer
More sensitive (85-100%) than amylase Stays elevated longer than amylase
question
Gallstone vs EtOH as a cause of pancreatitis
answer
History -Laboratory ALT > 150 U/L = 95 % specific for gallstone pancreatitis, 48 % sensitive Lipase:Amylase ratio > 2 -Imaging CT or US
question
pancreatitis prognosis
answer
1. Interstitial or edematous pancreatitis: 80-85 %, self limiting, low mortality 2. Nectrotizing pancreatitis: 15-20 %, severe, 20 % mortality
question
hemorrhagic complications

answer
Grey-turner's sign - patient has to turn to show you
question
acute pancreatitis treatment
answer
IV fluids enteral nutrition
question
reasons for enteral feeding of pancreatitis patients
answer
? Infectious complications ? Hospital stay ? Mortality ? Organ failure
question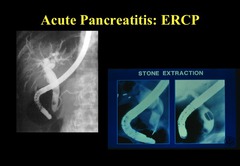
ERCP
answer
used to relieve obstruction --> endoscopic retrograde choliangiopancreascopy?
question
chronic pancreatitis
answer
Chronic inflammatory condition of the pancreas characterized by fibrosis with resultant destruction of pancreatic exocrine and endocrine tissue which can result in progressive and permanent change to the morphology and function of the pancreas -fibro inflammatory condition of the pancreas -Disfunction of the endocrine and exocrine cells: Endocrine Function- Insulin / glucagon production Exocrine Function- Digestion of fats and proteins
question
chronic pancreatitis clinical presentation
answer
Asymptomatic Pain Nausea Vomiting
question
chronic pancreatitis amylase and lipase levels
answer
often normal
question
Chronic Pancreatitis Presentation
answer
1. Pain (85%) -mid-epigastric to back, worse with food -Episodic or Chronic and steady -Chronic inflammation, increased intraductal pressure, noxious stimulation of pancreatic nerves 2. Malabsorption -loss of exocrine pancreas -80 % of gland destroyed -Weight loss -steatorrhea -vit. Deficiencies (ADEK) 3. Diabetes -loss of endocrine function -; 10% of normal exocrine function
question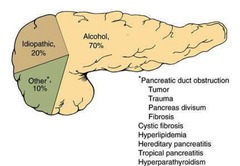
chronic pancreatitis etiology
answer
-Chronic alcoholism accounts for approximately 70% of all cases of chronic pancreatitis. Prolonged and substantial abuse is generally required to produce chronic pancreatitis, and most (but not all) patients who present with an episode of acute pancreatitis caused by alcohol consumption already have chronic pancreatic damage. -Chronic obstruction of the pancreatic duct may also produce chronic pancreatitis, such as that caused by tumors, trauma, pseudocysts, inflammation and fibrosis (such as after a severe episode of acute pancreatitis), pancreas divisum (with associated minor papilla stenosis), and even after prolonged endoscopic stenting of the the pancreatic duct. -After traumatic injury to the pancreatic duct (such as after a motor vehicle accident or a stab wound), chronic pancreatitis may develop within a few months.
question
Chronic Pancreatitis Pathophysiology
answer
1. Toxins (ETOH) lead to pancreatic juice rich in high viscous protein -Precipitation of protein plugs in small ductules than blockage/damage of larger ducts 2. Decreased production of lithostatin -Plug and stone formation 3. ETOH is a direct pancreatic toxin
question
Chronic Pancreatitis Diagnosis
answer
Histology - Gold standard Diagnosis - Clinical features + changes in pancreas structure/function Easy in late stages Difficult in "early" stages
question
Chronic Pancreatitis Imaging
answer
Abdominal x-ray - 30% with calcifications Ultrasound -Dilation of ducts, calcifications, change in pancreatic parenchyma -70% sensitivity CT/MR -Sensitivity of 75-90% ERCP - 95% sensitivity -Abnormal main and side branches, stricture, dilation, stones Endoscopic ultrasound
question
Chronic Pancreatitis complications
answer
Pseudocyst Bile duct obstruction Splenic vein thrombosis Pseudoaneurysms Pancreatic cancer
question
Chronic Pancreatitis treatment
answer
1) Pain management 2) Correction of pancreatic insufficiency 3) Complication management General -EtOH (? mortality) and Tobacco cessation -Small low fat meals and hydration Pain -Pancreatic enzyme replacement -Analgesia (Narcotics) Specialized Pain therapy -Endoscopy -Celiac plexus block -ESWL -Surgery Dilated main pancreatic duct - Lateral pancreaticojejunostomy
question
treatment of malabsorption/steatorrhea
answer
-Pancreatic enzyme replacement - varying amounts of lipase, amylase, protease -Vitamin supplementation -Medium chain triglycerides *Monitor for Chronic pancreatitis complications
question
pancreatic neoplasms
answer
4th leading cause of adult cancer deaths in the US presents the same as chronic pancreatitis: back pain and steattorrhea Exocrine cells ? Ductal Adenocarcinoma
question
Pancreatic Adenocarcinoma Prognosis
answer
20 % survival at 1 yr ;4 % survival at 5 yrs
question
Pancreatic Adenocarcinoma Risk Factors
answer
Smoking (biggest) ; 50 yrs old Diets high in fat Obesity Hereditary Pancreatitis
question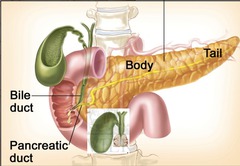
pancreas head Adenocarcinoma Clinical Presentation
answer
70 % of lesions -Jaundice -Steatorrhea -Constant pain: radiates to the back -Courvoisier's sign
question
pancreas tail Adenocarcinoma Clinical Presentation
answer
30 % of lesions -Diagnosed later than head lesions -Weight loss -Constant pain: radiates to the back
question
Pancreatic Adenocarcinoma Diagnosis
answer
Laboratory: -Mild elevation amylase/lipase -Elevated bilirubin/alkphos -Elevated CEA and CA 19-9 Imaging Studies: - Ultrasound - Dilated biliary ducts, 80 % sen. 90 % spec. -CT scan - 90% sen. 95 % spec. -ERCP - sen. and spec. of 90% -Endoscopic ultrasound - > 90% sen. and spec.
question
Pancreatic Adenocarcinoma: Staging
answer
T1 - 2 cm, confined to pancreas T3 - Invades major blood vessels or other organs N1 - regional lymph node metastasis M1 - Distant metastasis
question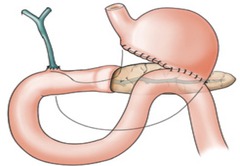
Pancreatic Adenocarcinoma Treatment
answer
-80% of patients unresectable at presentation -Cancer of pancreatic head - pancreaticoduodenectomy (Whipple) -Cancer of body or tail - distal pancreatectomy -2-5% operative mortality -Surgical resection - 10-25% 5 year survival
question
Pancreatic Adenocarcinoma Palliative Treatment
answer
Pain relief -Narcotic -Celiac ganglion block Biliary obstruction -Surgical bypass vs. endoscopic or percutaneous stenting Duodenal obstruction -Surgical bypass vs. endoscopic stent Chemotherapy/radiation
question
pancreatic adenocarcinoma survivability
answer
Resectable: -Median survival: 15-17 months 5 yr survival: 5-25 % Unresectable: -Median survival: 6-10 months locally advanced 3-6 months metastases
question
Cystic neoplasms of the pancreas
answer
1. Serous cystadenoma 2. Mucinous cystic adenoma/ adenocarcinoma (bad) 3. Intraductal papillary mucinous neoplasm (IPMN)
question
Serous cystadenoma
answer
-Patient: middle aged women -EUS: microcystic, located throughout pancreas -Fluid Analysis: sero sanginous, clear, ? amylase, ? CEA -Cytology: glycogen rich, cuboidal cells -Management: determined by location, considered a benign lesion
question
Mucinous cystadenoma/cystadenocarcinoma
answer
-Patient: 9:1, F:M, most common cystic neoplasm -EUS: macrocystic, septated, body/tail pancreas -Fluid Analysis: viscous, ? CEA -Cytology: mucinous columnar cells -Management: resection, considered premalignant
question
Intraductal papillary mucinous neoplasm
answer
-Patient: M=W -ERCP/EUS: thick mucus from ampulla, head of pancreas, dilated PD -Fluid Analysis: viscous, ? amylase -Cytology: mucinous columnar cells -Management: resection (main branch = premalignant) - Can cause pancreatitis
question
Pancreatic Endocrine Insulinoma
answer
-Most common panc. endocrine tumor -Clinical: Whipple's triad, change in MS -Diagnosis: hypoglycemia ; inappropriate plasma insulin level 90 % benign 70 % solitary lesions -Surgery: Curative 75-90 %
question
Pancreatic Endocrine Gastrinoma
answer
-Incidence of Zollinger Ellison unknown, -M;F -0.1 % of patients with DU -Massive gastric acid secretion ? ulcer disease ; diarrhea -10-15 % arise from the duodenum - 66 % local or nodal spread at diagnosis -Diagnosis: secretin stimulation test Rise in serum gastrin ; 120 pg/ml Sensitivity/Specificity ; 94 %
question
Pancreatic Endocrine Pancreatic Endocrine Gastrinoma
answer
- Rare -Presentation: glucose intol, wt loss, anemia and necrolytic migratory erythema -Most are large and malignant/metastatic -Diagnosis: ; plasma glucagon (nl ; 150 pg/ml) -Rx: octreotide
question
VIPoma
answer
Verner Morrison Syndrome -Rare -Presentation: large volume secretory diarrhea, hypokalemia -; 5 cm in size at diagnosis -Rx: Octreotide
question
acute pancreatitis
answer
Presention: RUQ pain, nausea/vomiting Etiology: Gallstones, EtOH Treatment: IVF, enteral feeding, ERCP
question
chronic pancreatitis
answer
Chronic epigastric pain Etiology: EtOH Treatment: Supportive
question
Pancreatic adenocarcinoma
answer
Poor prognosis, smoking risk factor, surgery is only chance for cure, multiple palliative therapies
question
Acute pancreatitis presentation
answer
-*Pain in epigastric area of radiating to the back* due to pancreatic inflammation -pain is steady and boring in nature and more intense when supine -patients are relieved by sitting, flexing their trunk, and pulling up their knees -nausea and vomiting are common because of hypo motility of the intestines
question
Acute pancreatitis laboratory data
answer
-Amylase and lipase levels increased in parallel with one another -amylase levels return to normal after 48 to 72 hours -lipase is elevated for 7-14 days -*threefold increase in serum lipase accompanied by classic abdominal pain is diagnostic for acute pancreatitis*
question
Other conditions in which amylase is elevated
answer
-Renal insufficiency -salivary gland lesions -cancer of the lungs, esophagus, breast, or ovaries -diabetic ketoacidosis -pregnancy -intestinal obstruction
question
Factors that determine the severity of acute pancreatitis
answer
-Presence of pancreatic necrosis and secondary inflammatory mediators that perpetuate the injury
question
hemoconcentration
answer
-Independent marker of severity -indicates the degree of intravascular hypovolemia stemming from the inflammatory cascade
question
Complications associated with acute pancreatitis
answer
Local complications: 1. *necrosis* -presence or absence of pancreatic necrosis -infected versus sterile necrosis -CT scan will show nonviable pancreas -infected the curses can be diagnosed with percutaneous biopsy and warns antibiotic treatment and possibly surgical debridement 2. *pseudo-cysts* -localized collections of pancreatic secretions that lack an epithelial lining -develop over a period of 4 to 6 weeks and occur in 10% of patients -resolved spontaneously but may cause pain, nausea, vomiting, infection, or bleeding
question
Systemic complications of acute pancreatitis
answer
-result from the release of *Inflammatory mediators* -highly correlated with the presence of necrosis -most common problems are: 1. Respiratory failure ? pleural effusion and acute respiratory distress syndrome may be seen in up to 20% of patients 2. Renal failure ? volume depletion results in acute tubular necrosis which is a poor prognostic sign 3. Hypotension/shock 4. Disseminated intravascular coagulation 5. G.I. bleeding -hyperglycemia and hypocalcemia are the most commonly observed metabolic disorders
question
Common etiologies of acute pancreatitis
answer
-*Gallstones* (45%) -*alcohol* (35%) -*idiopathic* (10%) -drugs: ART, azathioprine, sulfa -hypertriglyceridemia (;1000 mg/dL) -blunt trauma; post-ECRP, EUS, biopsy -abdominal and non-abdominal operations -sphincter of Oddi dysfunction
question
Uncommon etiologies of acute pancreatitis
answer
Pancreas divisum tumor hypercalcemia hypotension vasculitis autoimmune pancreatitis cystic fibrosis hereditary pancreatitis
question
Rare etiologies of acute pancreatitis
answer
Worms-ascariasis scorpion venom in Trinidad mumps cytomegalovirus Coxsackie virus
question
3 phases of acute pancreatitis pathogenesis
answer
1. Activation of zymogen granules with asking ourselves, fusion with the basal lateral membrane, and releases the interstitial space 2. Recruitment of activated neutrophils 3. Digestion of pancreatic and peripancreatic tissue by activated proteolytic enzymes such as trypsin
question
Zymogen granule activation
answer
Activated through a variety of both proposed mechanisms, including colocalization with lysosome/endosomes and cleavage of trypsinogen to trypsin by the hydrolase *cathepsin-B*, disruption of calcium signaling in acinar cells, and decreased activity of intracellular pancreatic trypsin
question
zymogen granules in pancreatitis
answer
-Activated zymogens I released to the basolateral membrane into the interstitial space -auto digestion and recruitment of activated neutrophils occur as a result -activated neutrophils convert trypsinogen ? trypsin will -trypsin activates elastase and phospholipase, which cause proteolysis, third spacing, hemorrhage, and necrosis -decreased intravascular volume from 3rd spacing leads to hypoperfusion of the pancreas, promoting additional inflammation and pancreatic necrosis
question
Systemic inflammatory response syndrome (SIRS)
answer
Systemic illness that results from the release of bradykinin, peptides, vasoactive substances, antihistamine which leads to vasodilation, increased vascular permeability, and 3rd spacing -also known as extra pancreatic inflammation; it can ultimately result in multi-organ failure
question
use of imaging in the diagnosis of acute pancreatitis
answer
-Imaging has little role in the diagnosis -ultrasound and CT show enlarged, edematous pancreas with associated fluid -may aid in determining the cause; gallstone or other obstruction -can be useful in evaluating for complications such as necrosis (which is not typically seen on CT scan for 48 to 72 hours after the onset of symptoms)
question
Treatment of acute pancreatitis
answer
-Based on severity -for mild cases, rest pancreas by not feeding the patient, and replacing fluids intravenously while providing sufficient pain relief -for severe pancreatitis when extended bowel rest is required, preferred method of feeding is via nasojejunal route
question
Goal of hydration in the treatment of acute pancreatitis
answer
Prevention of hypoperfusion and necrosis
question
Gallstone pancreatitis
answer
-Results from a gall stone being impacted in the distal common bile duct and subsequent inflammation and impaired flow from the pancreatic duct
question
Treatment of gallstone pancreatitis
answer
-Endoscopic sphincterotomy and stone extraction in patients with cholangitis or evidence of biliary obstruction
question
Treatment of severe pancreatitis
answer
-Aggressive supportive care and monitoring in the ICU for evidence of necrosis -suspected infected necrosis should be confirmed with CT guided percutaneous biopsy and treated with *imipenem/meropenem* or surgical debridement
question
Clinical manifestations of chronic pancreatitis
answer
1. Pain 2. Malabsorption due to exocrine insufficiency 3. Diabetes due to endocrine insufficiency
question
Chronic pancreatitis pain presentation
answer
-Multifocal and includes increased intra-ductal pressure from obstruction, inflammation/noxious stimulation of afferent nerves, and inflammation of the organ
question
Malabsorption and chronic pancreatitis
answer
-Pancreatic enzymes are needed to digest fat, protein, and carbs -with chronic disease states more exocrine cells are destroyed and nutrients can't be absorbed -result is diarrhea, weight loss, and vitamin A, D, E, K deficiencies -secretion of enzymes is efficient Intel destruction of more than 90% of the gland is present
question
Percent of pancreatic destruction required before exocrine insufficiency occurs
answer
90%
question
Diabetes and chronic pancreatitis
answer
-Endocrine cells (islet cells) are destroyed resulting in glucose intolerance and diabetes -occurs only at end-stage disease when >80-90% of the gland is no longer functional due to fibrosis/necrosis and inflammation
question
Etiology of chronic pancreatitis
answer
-major cause in the United States is *alcohol* (70-80%) -*idiopathic* (10-30%) ? 15% of idiopathic cases are secondary to genetic defects including *hereditary pancreatitis* -others: pancreatic duct obstruction (tumor, trauma, divisum, fibrosis) cystic fibrosis hyperlipidemia hereditary pancreatitis tropical pancreatitis hyperparathyroidism
question
Hereditary pancreatitis
answer
-Autosomal dominant disorder with incomplete penetrance -affects the gene encoding trypsinogen, along with the cystic fibrosis transmembrane regulator (CFTR) gene mutation, which functions as a cyclic AMP-regulated chloride channel
question
Autoimmune pancreatitis
answer
-Condition can mimic pancreatic cancer by presenting with obstructive jaundice and enlargement of the pancreatic head on imaging due to swelling -increased levels of IgG4 are often seen -increasingly recognized as a cause of chronic pancreatitis
question
Pathophysiology of chronic pancreatitis
answer
-*Sentinel acute pancreatitis event (SAPE) hypothesis*: pancreatic acinar cells are stimulated by alcohol or oxidative stress ? fibrosis doesn't occur because the pro-fibrotic cells aren't present ? zymogen activation does occur causing the 1st episode of pancreatitis which is referred to as the sentinel event. This results in a massive inflammatory episode that is divided into 2 phases: early phase = in flux of pro-inflammatory cells such as neutrophils which release cytokines that later attract and anti-inflammatory cell infiltrate during the late phase. Early phase also includes recruitment of pro-fibrotic *stellate cells*. continued exposure to alcohol or oxidative stress results in deposition of collagen leading to fibrosis and chronic pancreatitis however, if the initial insult were removed the pancreas would heal to it normal state
question
Diagnosis of chronic pancreatitis
answer
-Primarily made through imaging: 1. abdominal x-ray will demonstrate pancreatic calcifications in 30-40% of cases 2. Ultrasound has a 70% sensitivity showing dilation of the pancreatic duct, heterogeneity of the parenchyma, and calcifications 3. CT can demonstrate the same findings but with higher sensitivity 4.* Gold standard = endoscopic retrograde pancreatography (ERP)*, which has a 95% sensitivity and demonstrates abnormal main and side branch pancreatic ducts, stones, strictures, and dilation -less frequently through pancreatic function tests 1. Malabsorption leads to ? stool fat and ? fecal chymotrypsin late in the disease 2.* Gold standard of pancreatic function = secretin test*, which becomes abnormal when >60% of the exocrine function is lost. Usually correlates with onset of chronic abdominal pain
question
Secretin test
answer
intravenous stimulant that will result in decreased levels of duodenal bicarbonate, lipase, and trypsin in patients with chronic pancreatitis
question
goal of treatment in chronic pancreatitis
answer
Treat pain and pancreatic insufficiency Stop any ongoing toxins to the pancreas
question
Treatment of chronic pancreatitis
answer
1. Pain: -often requires oral *narcotic analgesia*. -*Synthetic pancreatic enzymes* inhibit pancreatic stimulation via the CCK feedback loop; potentially decreasing pain. -*Celiac plexus blockades* -*endoscopic stricture dilation, stone removal, or sphincter ablation* to remove obstructions that cause pain 2. Malabsorption/exocrine insufficiency: -successfully treated with synthetic pancreatic enzymes that contain protease, lipase, and amylase. provides necessary enzymes and nutrients can be absorbed, avoiding weight loss and resolving diarrhea and preventing vitamin deficiencies
question
Puestow procedure
answer
Used to treat chronic pancreatitis as an obstruction is present with a dilated main pancreatic duct -a.k.a. pancreatojejunostomy
question
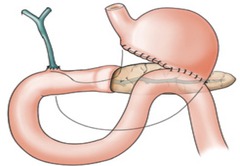
Whipple procedure
answer
Used for localized disease; Distal pancreatectomy is the removal of the head of the pancreas
question
Total or near total pancreatectomy
answer
Aggressive form of surgical treatment that can result in brittle diabetes
question
Percentage of malignant cancers of the pancreas that arise from exocrine cells; specifically ductal and acinar cells
answer
95%
question
Percent of pancreatic tumors that arise from endocrine cells
answer
2%
question
Only potential curative treatment for ductal adenocarcinoma
answer
Surgical resection
question
Percent of pancreatic cancer patients that are candidates for surgical resection
answer
15% ? most present too late in the disease
question
Percent of patients that survive one year after diagnosis of pancreatic cancer
answer
20%
question
Percent of patients that are alive 5 years after diagnosis of pancreatic cancer
answer
<4%
question
pancreatic carcinoma epidemiology
answer
peak age of incident = 7th decade of life -very rare in patients under 45 -more common in males and African-Americans
question
Environmental risk factors for pancreatic carcinoma
answer
Smoking (Nitro amines) -relative risk rapidly decreases when the patient stop smoking High fat/meat diet Obesity Lack of physical activity
question
Genetic risk factors for pancreatic carcinoma
answer
7-8% have a first-degree relative with the disease -main genetic alterations are the activation of oncogenes and inactivation of tumor suppressor genes -K-ras oncogene mutation (>90%) -p16 (95%), p53 (75%), DPC4 (55%) = tumor suppressor gene mutations -hereditary pancreatitis-patient have 50% lifetime risk of developing cancer -non-hereditary chronic pancreatitis is also a risk factor -diabetes mellitus is often known to predate diagnosis of cancer but has not been proven to be causative
question
location/presentation of pancreatic tumors
answer
-Based upon location of tumor in the pancreas -70% of rise in the pancreatic head -30% develop in body, tail or diffusely throughout the gland
question
presentation of pancreatic head tumors
answer
Jaundice or steatorrhea
question
Presentation of pancreatic body or tail tumors
answer
Pain and weight loss
question
Size of pancreatic head cancers at the time of diagnosis
answer
> 2 cm in diameter
question
Reason for jaundice in pancreatic head tumors
answer
Common bile duct courses to the head of the pancreas so >50% of patients present with mechanical obstruction of the common bile duct -for this reason had tumors are diagnosed earlier than body or tail tumors which are large and can metastasize prior to detection
question
Courvoisier's Sign
answer
Palpable, nontender gallbladder due to obstruction of the biliary system commonly caused by pancreatic head tumors
question
Pain in pancreatic tail or body tumors
answer
Pain is common (36-87% and is described as dull pain located in the epigastric region, and in advanced cases radiating to the back pain is secondary to tumor invasion of the celiac and superior mesenteric plexus
question
new onset glucose intolerance and pancreatic cancer
answer
Occurs in 6 to 68% of patients -secondary to overproduction of islet amyloid polypeptides -loss of 10% of body weight, fatigue and anorexia are associated with glucose intolerance
question
Less common presenting signs of pancreatic cancer
answer
-Acute pancreatitis secondary to obstruction -gastroparesis secondary to infiltration of the splanchnic neural network -thrombophlebitis (trousseau syndrome) -depression -aversion to meat
question
Diagnosis of pancreatic cancer
answer
-Based on identifying the presence and location of tumor -early diagnosis difficult due to lack of symptoms -1st modality used in diagnosis should be *thin section, dual phase pancreatic protocol CT scan* ? will identify primary tumor in ;90% of cases; will also identify the presence of liver metastases, and aid in evaluating whether the tumor is resectable
question
Diagnosis of tumors that are less than 2 cm
answer
Endoscopic ultrasound (EUS) is a better choice because it provides detailed images of the pancreas and surrounding structures through the posterior gastric wall And also allows for fine needle aspiration of the tumor tissue for diagnosis
question
Endoscopic retrograde cholangiopancreatography (ERCP)
answer
Endoscopic technique used to evaluate the bile ducts and pancreatic duct -has a sensitivity and specificity approaching 90% in identifying the presence of pancreatic cancer -more invasive so should not be used in the diagnosis alone; but could be used for therapeutic stenting of biliary obstruction
question
CA 19-9
answer
Serum blood test ? is elevated with pancreatic cancer but suffers from low sensitivity and specificity
question
Treatment of pancreatic cancer
answer
-Based on preoperative staging to determine if the patient has an operable tumor -only 20% of tumors are operable at the time of presentation and evaluation
question
Reasons why tumors may be unresectable
answer
-Metastatic disease to the liver, peritoneum, or any extra abdominal site -locally advanced disease including involvement of the bowel mesentery, Portomesenteric vasculature, or celiac axis
question
Metastatic staging
answer
-Performed with CT scan and sometimes PET scan or laparoscopy -local invasion of large vessels is done by a combination of CT scan and EUS
question
resection technique for tumors of the pancreatic head
answer
*Whipple procedure* or pancreatoduodenectomy
question
Survival rates after resection
answer
5 year rates are 10-25%
question
Resection technique for tumors of the body or tail
answer
Distal pancreatestomy
question
Treatment for locally advanced non-resectable tumors
answer
Radiation plus chemotherapy has a median survival improvement of 11 months
question
Treatment for metastatic disease
answer
Chemotherapy with *5 fluorouracil or gemcitabine* has shown small improvements in survival
question
3 basic types of pancreatic cystic neoplasms
answer
Serous cystadenomas Mucinous cystadenomas or cystadenocarcinomas Intraductal papillary mucinous neoplasms (IPMNs)
question
Serous cystadenomas
answer
-Account for 25% of cystic tumors -considered *benign lesions* without malignant potential -micro cystic, consisting of multiple small cysts with the larger lesions having central fibrotic or calcified scar -;50% diagnosed incidentally on imaging -symptoms (if present) are due to mass effect = nausea, vomiting, pain, bloating
question
Diagnosis of Serous cystadenomas
answer
Combination of CT and endoscopic ultrasound (EUS) -ultrasound guided cyst fluid and analysis will show no malignant cells and normal tumor markers for the cyst fluid
question
Serous cystadenoma Treatment
answer
Expectant observation and less symptoms from the mass effect of assist our present or if there is doubt about the malignant potential of the lesion
question
Mucinous cystadenomas and cystadenocarcinomas
answer
-Most common pancreatic cystic neoplasm -present far *more commonly in women (9:1)* -more common in the body and tail -macro cystic (Cysts ;1 cm in diameter) with discrete cuboidal cavities of varying size -presence of a mass, vocal tic meeting, or irregularity on imaging may suggest malignancy -should be *considered premalignant or frankly malignant* -frequently contain *K-ras oncogene or lack p53 tumor suppressor gene*
question
diagnosis of Mucinous cystadenomas or cystadenocarcinomas
answer
-Similar to serous cystadenomas because ;50% are diagnosed incidentally -remaining cases are diagnosed because of mass effect with nausea, bloating, pain -made by classic imaging of unilocal or multi component cystic lesion of the pancreas and *cyst fluid analysis* ? *elevated carcinoembryonic antigen and low amylase*
question
Treatment of Mucinous cystadenomas or cystadenocarcinomas
answer
Surgical resection because of the risk of malignancy -overall five-year survival = 50% (much better than pancreatic adenocarcinoma)
question
Intraductal papillary mucinous neoplasms (IPMNs)
answer
-Considered *premalignant to malignant* cystic neoplasm -affect men and women equally -generally in older patients -can develop from main pancreatic duct (80%) or from side branch (20%) -cause ductal dilation because of excessive mucin production from the cells lining the duct
question
Fish mouth papilla
answer
Massive pancreatic ductal dilation with mucin that can be see extruding from the papilla (associated with IPMN)
question
Presentation of Intraductal papillary mucinous neoplasms (IPMNs)
answer
Acute or chronic pancreatitis and abdominal pain due to ductal obstruction by mucin
question
Diagnosis of Intraductal papillary mucinous neoplasms (IPMNs)
answer
*Gold standard is ERCP* -shows mucin extruding from the papilla, diffuse ductal dilation, cystic dilation of side branches, and mucin filling defects pathology can be attained by brushing or pancreotoscopy directed biopsy
question
Treatment of Intraductal papillary mucinous neoplasms (IPMNs)
answer
Based on the suspicion of the presence of malignancy and the age and condition of the patient if patient is healthy and if there are symptoms or suspicion of malignancy, resection is performed
question
Pancreatic neuroendocrine tumors
answer
-Originate from neuroendocrine cells of the pancreas, which produce a variety amines and peptides -classified into fuctional and nonfunctional tumors based on whether the tumors are secreting hormone or not
question
Most common functional neuroendocrine tumors
answer
-Gastrinoma ? Gastrin -insulinoma ? insulin -VIPoma ? vasoactive peptide
question
Gastrinoma
answer
Result in extensive ulcer disease and diarrhea due to excess acid driven by extremely high production ? Zollinger Ellison syndrome
question
Insulinoma
answer
Cause hypoglycemic syndromes
question
VIPoma
answer
Result in severe watery separatory diarrhea and dehydration
question
Diagnosis of neuroendocrine pancreatic tumors
answer
-Detection of excess hormone production usually in serum -also commonly secrete proteins from the secretary granules called *Chromagranin* which are elevated in serum -tumor must be localized when excess hormone production is discovered tumor localization is achieved by combination of CT scan, endoscopic ultrasound, and somatostatin receptor scintigraphy -90 to 100% of tumors possess somatostatin receptors
question
somatostatin receptor scintigraphy
answer
Locates neuroendocrine tumors in 56-100% of patients -does not work so well on insulinomas which have low density of receptors
question
Treatment of neuroendocrine tumors
answer
Twofold: -correct excess hormone production -surgical resection ;10% of insulinomas are malignant; but 50-100% of other types are malignant and should be resected



