PANCE Review Neurology – Flashcards
Unlock all answers in this set
Unlock answersquestion
Tension HA S/S
answer
-Bilateral, non-throbbing, Band like "dull," "pressure," "head fullness", "head feels large," or, more descriptively, "like a tight cap", "band-like," or a "heavy weight on my head or shoulders." -Without photophobia, phonophobia, nausea, or vomiting.
question
What is the common HA:
answer
Tension HA
question
Tension HA Tx
answer
1st NSAIDS 2nd Relaxation exercises
question
Triggers for Tension HA
answer
Stress, fatigue
question
Migraine S/S
answer
Unilateral, throbbing, photophobia, N/V Migraine patients often retreat to quiet, dark rooms and prefer to lie quietly.
question
Migraine triggers:
answer
including chocolate, red wine, hard cheeses, monosodium glutamate, hormonal changes, exertion, fatigue, and stress.
question
Migraine often precede by
answer
aura (involving visual changes, field cuts, or flashing lights affecting one's visual hemifield.)
question
Migraine often is associated with other diseases, such as
answer
seizure disorders, essential tremor, Tourette's syndrome, depression, anxiety, and stroke.
question
The triad of headache, nausea, and vomiting in the morning are concerning for a brain tumor in the
answer
posterior fossa
question
Migraine Tx
answer
Mild to moderate migraine headache (1) Abortive therapy may include aspirin, acetaminophen, NSAIDs, or isometheptene. A variety of products may be combined with caffeine, which has an adjunctive effect. (2) Subsequent measures for migraine might include serotonin-receptor agonists, such as the triptans (e.g., sumatriptan, zolmitriptan, rizatriptan, naratriptan, almotriptan, frovatriptan, eletriptan). Various forms of the ergotamines also are useful. Triptans, Reglan (Metocloppramide: SE --> Tardive Dyskinea), *Verapamil for Basilar migraine*
question
Migraine HA prophylaxis
answer
BB, Tricyclic, Progestin if menses related.
question
Cluster HA S/S
answer
-Severe, unilateral, periorbital headaches, Lacrimation, eye injection, rhinorrhea, -unilateral pain of cluster headache often is accompanied by ipsilateral lacrimation, conjunctival injection, nasal congestion, and myosis and ptosis
question
Headaches Diagnosis Test
answer
CT scan or MRI
question
Prophylactic therapy for cluster headaches includes:
answer
valproate, cyproheptadine, lithium, *calcium channel blockers*, and oral corticosteroids.
question
Cluster HA Tx
answer
-Administration of *100% oxygen, injectable forms of ergotamines or sumatriptan*, and analgesics (e.g., intranasal butorphanol).
question
Cluster HA assoc.
answer
Horner's Syndrome (ptosis, miosis, anhydrosis) and Alcohol
question
Complex regional pain syndrome (CRPS) is a disorder of a body region, usually of the extremities, that is characterized by
answer
pain, swelling, limited range of motion, vasomotor instability, skin changes, and patchy bone demineralization. It frequently begins following an injury, surgery, or vascular event such as a stroke.
question
Three stages may occur during the course of CRPS

answer
It is a systemic disease affecting both the central and peripheral nervous system
question
Complex Regional Pain Syndrome S/S
answer
Severe Pain, burning inupper or the lower extremities; involvement of both upper and lower limbs in the same patient is unusual. "Pain out of proportion"
question
Complex Regional Pain Syndrome risk factor:
answer
immobilization, trauma, female
question
Complex Regional Pain Syndrome Dx
answer
Radionuclide uptake on Bone scintigraphy
question
Complex Regional Pain Syndrome Treatment
answer
Stage 1: 1st Neurotin Stage 2: Add steroid Stage 3: Pain management -Temporary sympathetic nerve block -Smoking cessation ?Anticonvulsants ?Bisphosphonates ?Oral glucocorticoids ?Nasal calcitonin
question
Peripheral Neuropathy S/S
answer
Slow onset for DM (sensory), but fast onset for Guillain (Motor): Sensory Loss, Burning, Weakness
question
Peripheral Neuropathy Dx
answer
Electromyography/ Nerve conduction study
question
Peripheral Neuropathy for DM Tx
answer
Tight blood sugar control Med: Gabapentin, if obese give Topiramate
question
Diabetic Neuropathy
answer
is primarily a symmetrical sensory polyneuropathy, initially affecting the distal lower extremities.
question
Diabetic polyneuropathy is generally considered *predominantly axonal-sensory*
answer
Is extremely complex and likely relates to inflammatory, metabolic, and ischemic effects
question
The earliest signs of diabetic polyneuropathy probably reflect the gradual loss of integrity of both large myelinated and small myelinated and unmyelinated nerve fibers:
answer
?Loss of vibratory sensation and altered proprioception reflect large-fiber loss ?Impairment of pain, light touch and temperature is secondary to loss of small fibers
question
Treatment of diabetic peripheral neuropathy ?Glycemic control ?Foot care ?Treatment of pain
answer
-Pregabalin has been found to significantly decrease mean pain score -On a daily basis, patients need to inspect their feet for the presence of dry or cracking skin, fissures, plantar callus formation, and signs of early infection between the toes and around the toe nails. Regular foot examinations by the physician to detect early neuropathy are also an essential component of the treatment of diabetic patients.
question
Treatments that are beneficial for painful diabetic neuropathy include:
answer
a number of antidepressants (eg, amitriptyline, duloxetine, venlafaxine), anticonvulsants (eg, pregabalin, sodium valproate), and capsaicin cream
question
Complications — Diabetic polyneuropathy is
answer
frequently insidious in onset and can lead to formation of foot ulcers and muscle and joint disease.
question
The most common forms of hereditary neuropathy
answer
*Charcot-Marie-Tooth* types 1A, 1B, and X-linked, are all predominantly demyelinating in nature, although substantial coexistent axonal loss is usually also identified.
question
Charcot-Marie-Tooth is
answer
also known as hereditary* motor and sensory neuropathy* (HMSN), encompasses the majority of hereditary peripheral neuropathies
question
The most common features of Charcot-Marie-Tooth are weakness and atrophy of the lower leg and foot. High-arched feet and hammertoes (pes cavus) are common but not pathogneumonic.
answer
Most patients present with difficulties walking, twisting of the ankles, and slapping of the feet. Features are normally symmetric, although asymmetries may occasionally occur. The majority of patients remain ambulatory, although they may need braces and other assistive devices. Severe cases also exist. Children with delayed motor milestones, who never ran or ambulated, have a severe early-onset phenotype of CMT1, CMT2, and CMT4 called Dejerine-Sottas syndrome.
question
Diagnostic Factors for Charcot-Marie-Tooth
answer
-family history of neuropathy, pes cavus, or abnormal gait -walking difficulties -pes cavus (hammertoe) -*steppage gait* -diffuse deep tendon hyporeflexia or areflexia -reduced muscle strength -reduced sensation -transient sensory symptoms -transient motor symptoms
question
Charcot-Marie-Tooth treatment
answer
Low-impact exercises, such as cycling and swimming, as well as *physical therapy* sessions, increase energy, as well as reducing fatigue and pain
question
*Initial diagnostic procedure for patients with suspected polyneuropathy *
answer
Electrodiagnostic testing with electromyography and/or nerve conduction studies (EMG/NCS)
question
Restless Leg Syndrome is
answer
is a disorder characterized by voluntary leg movements prompted by an urge to move which is often associated with unpleasant paresthesias.
question
Restless Leg Syndrome
answer
The urge to move is worse at rest and at night and relieved by movement. Accompanied by *dysesthesias described as creeping, crawling, tingling, cramping, or aching of the extremities.*
question
Restless Leg Syndrome Risk factors:
answer
-Family history consistent with autosomal dominant inheritance -Conditions associated with iron deficiency -End-stage renal disease (hemodialysis patients); associated factors that have been posited to play a role include anemia, iron deficiency, elevated serum calcium, and alterations in central nervous system dopamine. -DM, Multiple sclerosis, Parkinson's Disease pt
question
Restless Leg Syndrome Treatment:
answer
-Iron replacement -Dopamine Agonist: pramipexole or ropinirole
question
Bell's Palsy S/S
answer
Unilateral facial paralysis: -Inability close eye -unable to Wrinkle the forehead -Mouth drawn the non affected side -Loss of taste 2/3 anterior of the tongue -hyperacusis (hearing sensitivity)
question
Bell Palsy's with left affected
answer
On physical exam, the left eye is more open than the right, the left *nasolabial fold is absent, and the left corner of her mouth droops.* On the left side, she cannot voluntarily raise her eyebrow, close her eyelid, elevate her mouth into a smile, snarl, or pucker her lips.
question
Bell's Palsy+ Zoster
answer
Ramsay Hunt Syndrome
question
Bell's Palsy Tx
answer
Predinose, Acyclovir (if +herpes)
question
Bell's Palsy others causes
answer
Lyme disease
question
Transient ischemic attack (TIA) is a
answer
Transient episode of neurologic dysfunction caused by focal brain, spinal cord, or retinal ischemia, without acute infarction.
question
Majority of TIAs resolve within the
answer
first hour, and diagnostic imaging allows recognition that some events with rapid clinical resolution are associated with permanent cerebral infarction
question
Etiology of TIA
answer
-atherosclerosis, lipohyalinosis, inflammation, amyloid deposition, arterial dissection, developmental malformation, aneurysmal dilation, or venous thrombosis. -embolism of thrombus -Inadequate cerebral blood flow due to decreased perfusion pressure or increased blood viscosity. -rupture of a vessel in the subarachnoid space or intracerebral tissue.
question
A transient ischemic attack (TIA) should be considered a syndrome. These syndromes are conveniently divided into three pathophysiologic mechanisms:
answer
?Large artery low-flow TIA (true TIA) ?Embolic TIA, which may be artery-to-artery, or due to a cardioaortic or unknown source ?Lacunar or small penetrating vessel TIA
question
Large artery low-flow TIA (true TIA) Low-flow TIAs usually are short-lived (minutes) and often recurrent.
answer
Due to hemodynamically significant stenotic lesions at the origin of the internal carotid artery, at the siphon portion of the internal carotid artery where collateral flow to the circle of Willis is inadequate, or in the middle cerebral artery stem. Symptoms due to ischemia from these lesions often include hand, arm, leg, face, tongue, or cheek numbness or weakness together
question
Embolic TIAs in the anterior circulation: Embolic TIAs typically last hours rather than minutes as in low-flow TIAs.
answer
may be large enough to occlude the middle cerebral artery stem, producing a contralateral hemiplegia
question
TIA Clinical features
answer
a. If the TIA is related to a disturbance in carotid circulation, patients may demonstrate contralateral hand-arm weakness with sensory loss, ipsilateral visual symptoms or aphasia, or amaurosis fugax. Carotid bruit may be present, but with a high-grade stenosis (95%), it may be absent. b. Those experiencing vertebrovascular TIA may demonstrate diplopia, ataxia, vertigo, dysarthria, cranial nerve palsies, lower extremity weakness, dimness or blurring of vision, perioral numbness, or drop attacks.
question
TIA S/S
answer
Has weakness , visual loss, numbness but resolves
question
TIA Dx
answer
-Brain imaging with CT or MRI -Noninvasive options for evaluation of large vessel occlusive disease include magnetic resonance angiography (MRA), computed tomography angiography (CTA), carotid duplex ultrasonography (CDUS), and transcranial Doppler ultrasonography (TCD)
question
TIA tx
answer
-ASA, clopidogrel (Plavix) -*Cardiogenic TIA* requires anticoagulation, initially with *intravenous (IV) heparin for those who are admitted to the hospital and with warfarin for long-term therapy.*
question
TIA with BP ;185/100 treat with:
answer
Labetalol
question
Ischemia — There are three main subtypes of brain ischemia:
answer
?Thrombosis ?Embolism ?Systemic hypoperfusion
question
What is a major risk factor for ischemic stroke?
answer
Chronic hypertension Others: hypercholesterolemia, diabetes, oral contraceptives, cigarette smoking, heavy alcohol use, AIDS, and elevated blood homocysteine levels.
question
Stroke Clinical features a. Signs and symptoms of stroke begin abruptly and, by definition, last longer than 24 hours. They correlate with the area of the brain that is supplied by the affected vessel, especially with ischemic events.
answer
b. In most cases, hemiparesis or hemisensory deficit is revealed on history and physical examination. One can localize the lesion to one side, contralateral to these deficits.
question
Anterior Circulation Stroke:
answer
associated with hemispheric signs and symptoms (aphasia, apraxia, hemiparesis, hemisensory losses, visual field defects: Homonymous Hemianopia).
question
Posterior Circulation Stroke:
answer
which supplies the brain stem, cerebellum, thalamus, and portions of the temporal and occipital lobes, commonly are associated with evidence of brain stem dysfunction (coma, drop attacks, vertigo, nausea, vomiting, ataxia).
question
Ischemic Stroke Anterior involves
answer
Frontal and middle cerebral arteries
question
Ischemic Stroke S/S
answer
Hemiparesis
question
tPA contraindition
answer
1. BP ; 185/100 2. Recent MI the last 3 months 3. Major surgery 14 days ago 4. Increase PTT 5. Platelet 1.7 7. Glucose ;50 8. Active bleed 9. Head trauma the last 3 months 10. Hx of intracranial Hemorrhage
question
Ischemic Stroke Posterior Cerebellar Function "VANISH'D
answer
Vertigo Ataxia Nystagmus Intention tremor Slurred speech Heel-shin test Dysdiadochokinesia
question
Lacunar Stroke Syndrome
answer
?Pure motor hemiparesis ?Pure sensory stroke ?Ataxic hemiparesis
question
Lacunar Stroke often occur with pt with
answer
HTN and Diabetes
question
Pure motor hemiparesis
answer
It is characterized by weakness involving the face, arm, and leg on one side of the body in the absence of "cortical" signs (aphasia, agnosia, neglect, apraxia, or hemianopsia) or sensory deficit.
question
Pure sensory stroke
answer
defined as numbness of the face, arm, and leg on one side of the body in the absence of motor deficit or "cortical" signs.
question
Ataxic hemiparesis
answer
Develop ipsilateral weakness and limb ataxia that is out of proportion to the motor deficit. Some patients may exhibit dysarthria, nystagmus, and gait deviation towards the affected side.
question
What is the Cerebral Aneurysm?
answer
is an acquired focal abnormal dilation of the wall of an artery in the brain. Intracranial aneurysms are most commonly located at branching points of the major arteries at the base of the brain, which course through the subarachnoid space.
question
Types of cerebral aneurysm
answer
*Saccular* -Often termed a *berry aneurysm*, as it resembles a berry hanging from a vine -Rounded outpouching attached by a neck or stem to a brain artery. *Fusiform* -Also called atherosclerotic aneurysm -Forms as media damage leads to arterial stretching and elongation -Intraluminal clots may form.
question
Cerebral Aneurysm most common
answer
Berry Aneurysm
question
Ruptured saccular (berry) aneurysm accounts for approximately 75% of nontraumatic cases of:
answer
subarachnoid hemorrhage (SAH) and has a mortality rate of 50%
question
Cerebral Aneurysm Presentation
answer
HA, nuchal rigidity (New neck stiffness that includes pain on stretching the neck meninges with maneuvers.)
question
Cerebral Aneurysm assoc with
answer
Polycystic kidney Disease, Coarctation of the aorta, Endocarditis, Ehlers-Danlos
question
Cerebral Aneurysm Dx
answer
CT(referred initial diagnostic study)/MRI
question
Cerebral Aneurysm Tx
answer
Coiling. Clipping
question
Cerebral Aneurysm if rupture can lead to:
answer
Subarachoid Hemorrhage
question
Subarachnoid hemorrhage S/S:
answer
Acute onset Tunderclap HA, "Worst HA of my life" PE: Nuchal rigidity, impaired mental state Other signs of meningeal irritation, including *photophobia, nausea/vomiting*, and meningeal stretch signs, may also be seen.
question
HA, nuchal rigidity (Cerebral Aneurysm) + photophobia, nausea/vomiting (bleeding) =
answer
Subarachnoid hemorrhage
question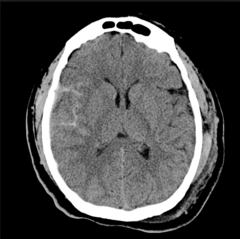
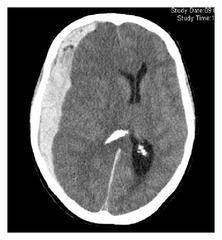
Subarachnoid hemorrhage Dx on CT
answer
-Look for Hyperdense area on CT. -Hyperdense areas in the basal cisterns, major fissures, and sulci
question
Subarachnoid hemorrhage Tx
answer
Clip or coil aneurysms
question
How you reverse Heparin treatment?
answer
Protamine Sulfate "He Pro me"
question
Subarachnoid hemorrhage: What should be performed if CT is unrevealing?
answer
Lumbar Puncture
question
How you reverse Warfarin treatment?
answer
Vitamin K & fresh frozen plasma (FFP) "War with Kings"
question
Brain Tumor Met
answer
1st Breast 2nd Lung 3rd GI 4th Kidney "Be loved or Get Knocked up"
question
Brain Tumor Dx
answer
MRI
question
Primary Brain Tumor Frontal lobe
answer
personality or intellectual change
question
Primary Brain Tumor Temporal Lobe
answer
lip smacking, olfactory or gustatory
question
Primary Brain Tumor Parietal Lobe
answer
sensory seizure or sensory loss
question
Primary Brain Tumor Brain stem
answer
cranial nerve palsy
question
Primary Brain Tumor Pituitary Tumor
answer
Endocrine symptoms
question
Primary Brain Tumor Occipital Lobe
answer
Visual defect or hallucination
question
Primary Brain Tumor Tx
answer
Surgery or radiotherapy
question
Epidural hematoma caused by
answer
Someone getting hit in the head
question
Epidural hematoma
answer
Transient loss of consciousness so-called "lucid interval"
question
Epidural hematoma other signs to look for:
answer
hematoma expansion leads to elevated intracranial pressure and clinical signs, such as an ipsilateral dilated pupil, hemiparesis.
question
Epidural hematoma artery involved
answer
Middle meningeal artery "MMA fighter"
question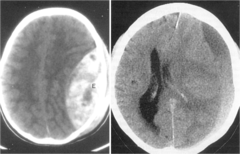
Epidural hematoma CT brain
answer
Convex, biconvex, lens shape
question
Epidural hematoma Tx
answer
Urgent surgery
question
Elderly pt with multiple fall over the past 6 months or year..think!
answer
Subdural Hematoma
question
Subdural hematoma is
answer
a collection of blood between the dural and arachnoid coverings of the brain. As the volume of the hematoma increases, the intracranial pressure may rise and cause herniation.
question
___________ is the most common cause of Subdural hematoma, with the majority of cases related to motor vehicle accidents, falls, and assaults.
answer
Head trauma
question
Subdural hematoma risk factors:
answer
-Patients with significant cerebral atrophy are at high risk for SDH. -Recent trauma, elderly, those with a history of chronic alcohol abuse, and those with previous traumatic brain injury, coagulopathy, anticoagulant use.
question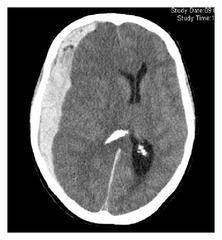
Subdural Hematoma Dx:
answer
CT brain -Concave, crescent shaped
question
The categories of acute, subacute, and chronic SDH are arbitrarily defined by time from onset:
answer
?Acute SDH presents one to two days after onset ?Subacute SDH presents 3 to 14 days after onset ?Chronic SDH presents 15 or more days after onset
question
Acute subdural hematoma PE
answer
symptoms of elevated intracranial pressure including headache, vomiting, anisocoria, dysphagia, cranial nerve palsies, nuchal rigidity, and ataxia.
question
Chronic subdural hematoma PE
answer
The insidious onset of headaches, light-headedness, cognitive impairment, apathy, somnolence, and occasionally seizures, may occur as a consequence of chronic SDH, and symptoms may not become evident until weeks after the initial injury. Global deficits such as disturbances of consciousness are more common than focal deficits after SDH.
question
Subdural Hematoma S/S
answer
HA, N/V, nuchal rigidity, anisocoria, dysphagia
question
Subdural Hematoma Tx
answer
*Burr holes* or craniotomy -Once the diagnosis has been established, *burr holes* over the hematoma are indicated to evacuate the clot.
question
Subdural Hematoma increase intracranial pressure. What is treatment?
answer
Hyperventilation, *Mannitol*
question
Seizure Partial Seizure: Simple and complex
answer
Simple: Consciousness is not impaired Complex: Consciousness is impaired (Over 30 sec)
question
Seizure Generalized: Absence, Tonic-Clonic
answer
Absence: Staring <15 sec Tonic: Body very stiff and rigid Clonic: Convulsions and limb jerking
question
Seizure eval:
answer
Glucose Level, Electrolytes, ABG, CBC, Urine toxic, Drug
question
Partial Seizure two type: -Complex partial seizure -Simple partial seizure
answer
-A complex partial seizure (CPS) implies that consciousness is impaired -Simple partial seizures (SPS) are not associated with altered consciousness.
question
Complex partial seizure
answer
they often seem to stare into space and either remain motionless or engage in repetitive behaviors, called automatisms, such as facial grimacing, gesturing, chewing, lip smacking, snapping fingers, repeating words or phrases, walking, running, or undressing. Patients may become hostile or aggressive if physically restrained during complex partial seizures.
question
-Simple partial seizures
answer
-Beginning of the seizure are referred to as the warning or aura. -The symptoms of simple partial seizures vary from one patient to another and depend entirely on where the seizure originates in the brain, that is, the part of the cortex that is disrupted at the onset of the seizure. A seizure that begins in the occipital cortex may result in flashing lights, while a seizure that affects the motor cortex will result in rhythmic jerking movements of the face, arm, or leg on the side of the body opposite to the involved cortex (Jacksonian seizure).
question
Partial Seizure focal location in the brain affected often
answer
temporal lobe
question
Generalized Seizure: start midbrain or brainstem, spread to both cortices
answer
Subtypes of generalized seizures are: -tonic-clonic seizures (grand mal) -absence seizures (petit mal) -myoclonic seizures.
question
What is the frequent complication of alcohol withdrawal?
answer
Generalized Seizure
question
Tonic-Clonic Seizure Presentation
answer
-It begins with an abrupt loss of consciousness, often in association with a scream or shriek. -*All of the muscles of the arms and legs as well as the chest and back then become stiff*. The patient may begin to appear cyanotic during this *tonic phase* -After approximately one minute, the *muscles begin to jerk and twitch for an additional one to two minutes. During this clonic phase* the tongue can be bitten, and frothy and bloody sputum may be seen coming out of the mouth.
question
Absence seizures (petit mal)
answer
Absence seizures (also called petit mal) usually occur during childhood and typically last between 5 and 10 seconds. They frequently occur in clusters and may take place dozens or even hundreds of times a day. *Absence seizures cause sudden staring with impaired consciousness*
question
Absence Sz tx
answer
Ethosuximide, Valproic Acid
question
Partial Sz Tx
answer
Carbamazepine, 2nd line Valproic Acid
question
Generalized Sz Tx
answer
Valproic Acid
question
Phenytoin can be used for
answer
Partial and Generalized, but not Absence Sz
question
The most common medical neurologic emergency in childhood, ____________ is a serious and often life-threatening medical emergency
answer
status epilepticus (SE) Lasts for a sufficient length of time (30 minutes or longer in most studies) or is repeated frequently enough that the individual does not regain consciousness between seizures
question
Status epilepticus emergency due to
answer
permanent brain damage secondary to hyperthermia, circulatory collapse, or excitotoxic neuronal damage
question
Status Epilepticus
answer
Sz longer than 5-10 min.
question
Status Epilepticus Tx
answer
-Maintain ABCs; consider rapid intubation for airway protection. -Administer thiamine, followed by glucose and naloxone to presumptively treat potential etiologies. -Give an IV benzodiazepine (lorazepam or diazepam) plus a loading dose of fosphenytoin.
question
Status Epilepticus Caused by
answer
Decrease in K+, Na+, hypoglycemia
question
Neurogenic Syncope is due to
answer
reflex response Triggered by stress: Venipuncture, prolonged standing, heat, fear of injury, painful or noxious stimuli
question
Neurogenic Syncope Dx
answer
Check orthostatic , Glucose Tilt table test Holter monitor
question
Neurogenic Syncope Tx
answer
Avoid situation causing the trigger Pt education Proper Hydration
question
Concussion is
answer
is a closed head injury due to a direct blow to the head or deceleration of the head from an impulsive force that results in a change in mental status.
question
Diagnosis of concussion should be considered if 1 or more of the following are reported or observed:
answer
-Confusion or disorientation -Amnesia near the time of the injury (retro- or anterograde) -Loss of consciousness for up to 30 minutes -Neurologic or neuropsychological problems -Score 13 or higher on the Glasgow Coma Scale (GCS).
question
Concussion Symtoms and Sign
answer
-The hallmark symptoms of concussion are confusion and amnesia, sometimes with, but often without, preceding loss of consciousness. - Early symptoms of concussion (within minutes to hours) include headache, dizziness (vertigo or imbalance), lack of awareness of surroundings, and nausea and vomiting
question
How many min after injury can you do the Glasgow Coma Scale?
answer
30min after injury
question
Tremors: Resting
answer
Parkinson's disease Tremor at rest goes away with movement Tx: Dopamine agonist
question
Cantu Guidelines Grade 2
answer
+LOC 30mins but <1 week Anything less than that should be grade 1 Anything greater should be grade 3
question
Tremors: Action 2 kinds
answer
Physiologic: Due to caffeine, catecholamines, nicotine, anxiety. Tx with removal of offending agents Essential: Genetic Tx: Propranolol and primidone
question
Tremors: intention
answer
Tremor increase in severity as the hand moves closer to its target. Tx: no treatment
question
Parkinson's Treatment
answer
age 65: Levodopa, carbidopa Pt <65 taking Levodopa, this can cause dyskinesia
question
Parkinson's Disease S/S:
answer
shuffling stepping gait, cogwheel rigidity, pill-rolling, lack of facial expression.
question
Huntington' s disease
answer
is an inherited, autosomal dominant disorder that occurs throughout the world in all ethnic groups.
question
Huntington' s disease S/S
answer
a. The disease is characterized by progressive *chorea* and dementia; it is usually fatal within 15 to 20 years. b. The earliest mental changes often are behavioral, with irritability, moodiness, and antisocial behavior that generally progress to an obvious dementia. c. The earliest physical signs may be a mere restlessness or fidgetiness, but, eventually, *severe choreiform* movements and dystonic posturing occur.
question
Huntington' s disease Dx
answer
CT demonstrates cerebral atrophy as well as atrophy of the caudate nucleus. MRI and PET scans have shown decreased glucose metabolism in an anatomically normal caudate nucleus.
question
Huntington' s disease Tx:
answer
*Chorea: Tetrabenazine* Chore+psychosis: Olanzapine, risperidone, haloperidol Symptomatic treatment for the disease may include phenothiazines to control dyskinesia, and haloperidol or clozapine to control any behavioral disturbances.
question
Extrapyramidal syndrome is usually due to the intake of
answer
Haldol
question
Extrapyramidal syndrome
answer
movement disorders such as akathisia, dystonia, and parkinsonism, caused by antipsychotic drug therapy
question
What is akathisia?
answer
-The state of restlessness characterized by an urgent need for movement, usually as a side effect of medication.
question
What akathisia can be prevented by giving?
answer
Benzodiazepine medicationf
question
Extrapyramidal syndrome tx
answer
Diphenhydramine (Benadryl)
question
Tardive Dyskinesia
answer
A side effect of long-term use of traditional antipsychotic drugs causing the person to have uncontrollable facial tics, grimaces, and other involuntary movements of the lips, jaw, and tongue.
question
Guillain-Barre is an
answer
autoimmune neuropathies, are *predominantly demyelinating*, and a variety of clinical and experimental data have implicated both humoral factors and cell-mediated immune phenomena, which damage myelin and/or the myelin-producing Schwann cells.
question
Guillain-Barre PE
answer
Acute asymmetric ascending inflammatory neuropathy; Weakness begins in lower and ascends; respiratory failure can occur in sever cases; *reflexes invariably decreased or absents*; 2/3 of patient have respiratory or GI illness 1-3 weeks prior to onset; Albuminocytologic dissociation
question
Guillain-Barre
answer
Weakness of the legs to total paralysis of all four limbs, facial muscles, and eyes.
question
Initial diagnosis of Guillain-Barré syndrome (GBS) is based upon the clinical presentation.
answer
Cerebrospinal fluid analysis — In patients with GBS, lumbar puncture often reveals an *elevated CSF protein with a normal CSF white blood cell count. This finding, known as albuminocytologic dissociation*
question
Guillain-Barre can be cause by what...
answer
Campylobacter jejuni, CMV, HIV, or by recent immunization
question
Guillain-Barre Dx
answer
1st initial :Lumbar puncture Increase CSF protein, with normal WBC -Electromyography
question
Guillain-Barre Tx
answer
-1st Line IV Immune globulin -Plasma exchange (remove circulating antibodies) *Avoid Steroids*
question
Myasthenia Gravis
answer
autoimmune attack of acetycholine receptors in neuromuscular junction
question
Myasthenia Gravis Word breakdown
answer
My=Muscle A= Without Sthenos= Strength
question
Myasthenia Gravis Symptoms
answer
Proximal to distal weakness Eyes: bilateral Ptosis usually 1st The weakness is limited to the eyelids and extraocular muscles
question
Myasthenia Gravis
answer
DTR are intact, no sensory abnormalities, normal pupillary light relfex
question
Myasthenia Gravis Dx:
answer
Best initial test: Acetylcholine receptor antibody. *More reliable laboratory methods that aid in the confirmation are serologic tests for autoantibodies and electrophysiologic studies* (muscle fiber contraction on repetitive nerve stimulation) Edrophonium/Tensilon Test (Acetylcholinesterase inhibitor)
question
Myasthenia Gravis: Chest radiographs (CT or MRI should be obtained to rule out a coexisting _________.
answer
Thymoma
question
Myasthenia Gravis associated with
answer
High incidence of thymus abnormalities
question
Myasthenia Gravis tx
answer
Pyridostigmine (cholinesterase inhibitor) Thymectomy if < 60 y.o.
question
Myasthenia Gravis Alternative treatment
answer
-Corticosteroids, immunosuppressive agents. -If steroid fail- Azathioprine usually added. -IV immunoglobulin, and plasmapheresis are effective in patients with refractory disease.
question
Myasthenia Gravis can cause by medication:
answer
Magnesium Sulfate, pencillamine, *aminoglycoside*, interferon-Alpha
question
Myasthenia Gravis S/S
answer
ptosis, weak chewing, fatigue, weakness with everday activities (brushing hair, etc)
question
Multiple Sclerosis
answer
Distal to proximal weakness or or visual changes often over many years due to demyelination and inflammation on CNS not peripheral).
question
Patients with MS typically follow either a relapsing-remitting pattern of episodes or a primary progressive course.
answer
A secondary progressive form also is seen, in which the relapsing-remitting pattern changes to one of progressive degeneration.
question
Multiple Sclerosis Dx
answer
-diagnosis cannot be based exclusively on laboratory findings. *MRI with gadolinium is very effective for visualizing white matter lesions in the CNS.* 2nd: *Oligoclonal bands and elevated CSF IgG and IgG synthesis rates are present in 80% of MS cases*
question
Multiple Sclerosis MRI hints
answer
White matter changes/ T2 hyperintensity
question
Multiple Sclerosis Lab
answer
mild lymphocytosis or slight protein elevation, elevated immunoglobulin G index, oligoclonal bands, and increased myelin basic protein
question
Multiple Sclerosis S/S
answer
Optic neuritis & vision changes often 1st
question
Multiple Sclerosis Tx
answer
Acute: Glucocorticoids Long-term: Interferon Beta
question
The cerebral palsy (CP) syndromes are
answer
characterized by abnormalities of motor activity and posture.
question
Cerebral Palsy 3 Types Movement disorder classification
answer
Spastic Dyskinetic Ataxic
question
Cerebral Palsy: Spastic
answer
Spastic CP is an upper motor neuron syndrome. S/S: spastic hyperreflexia, extensor plantar, response, and clonus May be: Diplegia, asymmetric, Hemiplegia, Quadriplegia
question
Cerebral Palsy: Dyskinetic
answer
Involuntary, recurring, and occasionally stereotyped movements with a varying muscle tone. Subgroups include: Dystonia: characterized by involuntary, sustained contractions resulting in twisting and abnormal postures. Chorea: rapid, involuntary, jerky, and fragmented motions; tone is usually decreased but fluctuating. Athetosis: slower, constantly changing, writhing, or contorting movements.
question
Cerebral Palsy: Ataxic
answer
Loss of muscular coordination with abnormal force and rhythm, and impairment of accuracy. Commonly presents with gait and trunk ataxia, poor balance, past pointing, terminal intention tremor, scanning speech, nystagmus and other abnormal eye movements, and hypotonia.
question
Cerebral Palsy due to
answer
The multifactorial etiology was illustrated in a series of 213 children diagnosed with CP in Australia. Major CP-associated pathologies other than acute intrapartum *hypoxia were identified in 98 percent of cases*
question
Cerebral Palsy Diagnostic test:
answer
MRI periventricular leukomalacia, congenital malformation, stroke or hemorrhage, cystic lesions
question
Cerebral Palsy Treatment:
answer
Treatment is supportive, with the goal of attaining maximum function and potential in physical, occupational, and speech ability
question
Meningitis aseptic meningitis:
answer
-Viral or other cause -Most common cause is enterovirus (Coxsackie A and B viruses, Echoviruses, and Polioviruses) - Additional etiologies include other infections, (mycobacteria, fungi, spirochetes), parameningeal infections, medications, and malignancy
question
Meningitis Bacteria
answer
S. Pneumonia N. Meningitis (Look for rash)
question
Meningitis aseptic Presentation
answer
headache, nausea and vomiting, photophobia, neck stiffness (nuchal rigidity), fever
question
Meningitis Daignostic
answer
Examination of the cerebrospinal fluid (CSF) is crucial for establishing the diagnosis of bacterial meningitis, identifying the causative organism, and performing in vitro susceptibility testing . Indications for CT scan before LP — Every patient with suspected meningitis should have CSF obtained unless lumbar puncture (LP) is contraindicated.
question
What is the rational for dosing dexamethasone prior to or along with the first dose of antibiotics for empiric treatment of bacterial meningitis?
answer
Dexamethasone when given with or prior to the first dose of antibiotic reduces the risk of *Hearing losss* in children with meningitis, especially in the cases of Influenza B, TB, meningitis.
question
Meningitis Bacteria Tx
answer
Dexamethasone (used to minimize adema within the CNS) Ceftriaxone, Macrolides, Penicillin
question
In adults with bacterial meningitis, dexamethasone reduces both morbidity and mortality especially in the case of
answer
Strept Pneumo
question
Meningitis Bacteria look for increase in intracranial pressure
answer
Do fundascopic exam to r/o papillaedma
question
Most common Meningitis Bacteria in the 1st month of life
answer
Group B strep and E.Coli
question
In the adult with rash, which of the following is the most likely organism to cause bacterial meningitis?
answer
N. Meningitis
question
What is the treatment for viral meningitis?
answer
-Acetaminophen for pain -IV Fluid -Empiric antibiotics Until viral is confirmed -Acyclovir if suspicion of HSV
question
In the adult neutropenic (immunocompromised) patient, which of the following is the most likely organism to cause bacterial meningitis?
answer
Listeria
question
What is Encephalitis?
answer
is a pathologic state of brain parenchymal dysfunction demonstrated by an altered state of consciousness and/or signs of neurologic dysfunction (e.g., seizures, personality changes, cranial nerve palsies, speech problems, and motor and sensory deficits).
question
Encephalitis organisms:
answer
HSV and arboviruses are the most common causes of encephalitis. Rarer etiologies include CMV, toxoplasmosis, West Nile virus, VZV, Borrelia, Rickettsia, Legionella, enterovirus, Mycoplasma, and cerebral malaria. Children and the elderly are the most vulnerable
question
Encephalitis presentation
answer
-markedly altered consciousness, seizures, personality changes, or other focal neurologic signs. -Lethargy, confusion, coma, and focal neurologic deficits (cranial nerve deficits, accentuated DTRs) may also be present.
question
Encephalitis Diagnostic Test
answer
initial diagnostic step in the patient with suspected viral encephalitis is analysis of the CSF; lumbar puncture
question
Encephalitis treatment
answer
-HSV encephalitis: Requires immediate IV acyclovir. -CMV encephalitis: Treat with IV ganciclovir +/? foscarnet. -Give doxycycline for suspected Rocky Mountain spotted fever, Lyme disease, or ehrlichiosis.
question
Rabies S/S
answer
Hydrophobia, aerophobia, pharyngeal spasms, and hyperactivity
question
Rabies Tx
answer
Rabies Immunoglobulin
question
Encephalopathy: vomiting, confusion, Sz, coma in child after exposure to
answer
Saliccylates (ASA), Pept-Bismol Condition called *Reye's Syndrome*
question
What is Reye's Syndrome?
answer
Reye's Syndrome, or fatty liver encephalopathy, has been associated with ASA use in children with viral infections, including influenza.
question
Reye's Syndrome treatment
answer
-Ondansetron may be given to decrease vomiting. -Seizure: phenytoin
question
Dementia with Lewy Bodies:
answer
-Visual hallucinations -Progressive dementia -Spontaneous motor features of Parkinsonism
question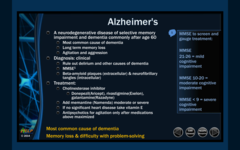
Alzheimer's Disease
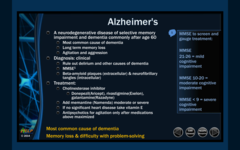
answer
-Age >60 -MMSE -Memory loss
question
Alzheimer's Disease Treatment
answer
Donepezil, rivastigmine, and galantamine.



