Menopause – Flashcard
Unlock all answers in this set
Unlock answersquestion
Basic Overview
answer
-> Menopause occurs with the cessation of estrogen production -> Estrogen depletion leads to a constellation of symptoms that can significantly impact quality of life ->Management of these symptoms can be difficult with estrogen being the best therapy with concerns regarding long term risks ->Osteoporosis is the most important sequelae of long term estrogen deprivation.
question
Menopause
answer
12 months of amenorrhea after the final menstrual period. If reflects ovarian follicle depletion and absence of ovarian estrogen production
question
Perimenopause
answer
Period immediately before and after menopause. Starts with variation of menstrual cycle and ends at start of menopause.
question
Postmenopause
answer
Postmenopause - the first five years after the final period. Have ongoing symptoms and accelerated bone loss.
question
Progression
answer
Median age is 50 - 52 years of age Anovulation becomes more prevalent during perimenopause Ovary becomes more resistant to FSH FSH increases in order to maintain estrogen at steady state. Eventually follicles are depleted, and estrogen production ceases
question
Symptoms
answer
Short term -Vasomotor -Atrophic changes -Psychophysiological Long Term -Osteoporosis -Cardiovascular
question
Vasomotor
answer
The physiology is not clear -Related to estrogen withdrawl at level of hypothalamus -Hot flushes (head, neck, chest, intense body heat)
question
Atrophic
answer
-Thinning and inflammation of vaginal mucosa secondary to lack of estrogen -Can lead to secondary symptoms like bleeding and dysparunia -Can also develop burning with urination -Urgency
question
Psychophysiologic
answer
Unclear wether this is a lone entity or associated with vasomotor symptoms (sleep deprivation) -Depression, irritibility, memory, anxiety
question
Osteoporosis
answer
This occurs due to down regulation of osteoclasts and osteoblasts -The most important complication associated with fractures
question
Cardiovascular
answer
This is controversial!! -May benefit lipids, atherosclerosis, vasodilation -May increase stroke and MI
question
Management
answer
Symptom control and reduce risk of osteoporosis!!! Modalities: -HRT (very effective but symptoms need to be debilitating as it causes a small increase in risk similar to being obese) -HRT can be given orally (premarin), transdermally (patch or gel with theoretical benefit), or locally (reduces systemic effect as suppository, ring, cream) -HRT patients should be given progestin if they have a uterus -HRT Contraindications (Unexplained vaginal bleeding, acute liver disease, thrombus, known or suspected breast Ca, pregnancy) -effexor, clonidine -Life style + vitamin D
question
Osteoporosis
answer
Related to depletion of estrogen which can cause bone loss and increase risk of fracture Can screen using bone density (DEXA - dual energy absorbitometry) Measure hip and spine Change by as little as one standard deviation can lead to 3X increase risk of fracture Measured as T score (standard deviation) -> Lifestyle management is a great way to manage it -> Estrogen (not recommended for prevention), SERMS, bisphosphonates and calcitonin are good ways to
question
Postmenopausal Bleeding Keys
answer
Postmenopausal bleeding is very common problem (11%). The largest concern is excluding uterine cancer. Early diagnosis and management can lead to survival rates of up to 95%. Diagnostic modalities include ultrasound, endometrial biopsy and dilation and curettage. Remember biopsy, biopsy, biopsy as tissue sampling is the gold standard.
question
PMB Definition
answer
Any uterine bleeding in a menopausal woman other than expected cyclical bleeding in women on HRT
question
PMB Incidence
answer
Estimated as high as 10 -15% Higher in first year after one year of amenorrhea Falls significantly after third year
question
Etiology
answer
Think anatomically -Vulva -Vagina -Cervix -Uterus -Fallopian Tube
question
Vulvar Sources
answer
Atrophy Dystrophies Infectious causes Vulvovaginitis carcinoma
question
Vaginal Sources
answer
Atrophy Vaginal carcinoma Vulvovaginitis Infectious Trauma
question
Cervical Sources
answer
Polyps Ectropion Dysplasia Carcinoma
question
Uterine Causes
answer
Atrophy 59% -Hypoestrgenism causes atrophy -lack of fluid leads to friction... Polyps, fibroids 12% -benign endometrial or myometrial growths that have inflammatory processes going on around the growth -inflammation makes it friable which can subsequently bleed -fibroid in postmenopausal women = sarcoma!! Endometrial cancer 10% -fibroids in older women -always have it on the differential -Adenocarcinoma is the most common kind -First sign is often bleeding -Investigate with U/S (90% sensitive), Endometrial biopsy (95% sensitive), Dilation and curettage via hysteroscopy (95% sensitive) -Management includes avoiding unopposed estrogen and removing the tumor as soon as possible Hormonal effect 7% -Any woman can develop bleeding depending on how the hormones are taken so you can inform her Other (pyometra, hematometra) 2%
question
Menopause occurs Between ages 50-55. when is the average age?
answer
Average age is 51 years
question
What is considered "premature" Menopause?
answer
< 40 years
question
What is considered ealry menopause?
answer
between the age 40-45
question
What is considered late menopause?
answer
After age 55
question
What could cause "premature" Menopause?
answer
1) Karyotype abnormalities (Turner's XO) 2) Autoimmune disorders 3) Iatrogenic - Surgery—Bilateral Salpingo-oophorectomy (BSO) - Chemotherapy - Radiation (XRT)
question
Describe the process of Ovarian Senescence
answer
1) Begins with approximately 1.5 million eggs 2) Menarche: 400,000 eggs 3) 400 menstrual cycles 4) No eggs = no physiologic response to gonadotropins (FSH/LH)
question
Transition Stage -2
answer
Variable cycle lengths and greater than a 7 day difference of the cycles
question
Transition Stage -1
answer
> or equal to 2 skipped cycles and a period of amenorrhea for 60 days
question
Menopause- 0
answer
Menopause (No menstural cycle for 12 months)
question
Post Menopause Stage +1
answer
First 5 years after final period
question
Post Menopause Stage +2
answer
From first 5 years until death
question
What are the symptoms of perimenopause?
answer
1) Irregular menses 2) Endometrial hyperplasia 3) Mood/emotional changes 4) Hot flashes (flushes) 5) Night sweats
question
What causes perimenopause?
answer
1) Ovary function waxes & wanes - Irregular ovulation o Contraception required until amenorrhea X 1 yr - Fluctuating hormone production o Estrogen/Progesterone ultimately cease o Ovary still produces small amounts of androgens during menopause
question
In perimenopause there are Anovulatory cycles. What does this cause?
answer
1) Leads to irregular menses 2) Increased estrogen due to prolonged follicular phase - Exacerbated by obesity - Endometrial stimulation can lead to endometrial hyperplasia or cancer 3) Ultimately no more eggs--no more ovarian estrogen!
question
How is Menopause diagnosed?
answer
1) No menses x 1 yr 2) Serum FSH not necessary - levels will vary throughout perimenopause
question
During menopause, what is Androstenedione precursor in the adrenal gland converted to?
answer
ESTRONE in peripheral fat (which is less potent than estadiol which is produced by the ovaries prior to menopause)
question
What are the consequences of menopause?
answer
1) Vasomotor symptoms (which causes the hot flashes)/Mood symptoms 2) Vulvovaginal atrophy 3) Osteoporosis (The vast majority of bone loss is during the perimenopause period and the year after menopause) 4) Increased risk of CAD/CVA (?) 5) Increased risk of colon cancer (?) 6) Imapired balance (increased risk of colles fractures)
question
What is the treatment of vasomotor symptoms?

answer
1) Lifestyle 2) HRT (Hormone Replacement Therapy)--> The MAIN reason for HRT is to prevent hot flashes
question
What are the indications for Hormone Replacement Therapy (HRT)Estrogen Replacement Therapy (ERT)?
answer
1) Vasomotor sx 2) Vulvovaginal atrophy 3) Osteoporosis (*In women that also have vasomotor sx)
question
What are the ciontraindications for Hormone Replacement Therapy (HRT)Estrogen Replacement Therapy (ERT)?
answer
1) Pregnancy 2) AUB 3) Estrogen-sensitive CA (i.e. Breast cancer) 4) Thromboembolic disease or CVA 5) Liver disease 6) Coronary Artery Disease
question
What would I use for a women in menopause that still has a uterus and why?
answer
Hormone Replacement Therapy (HRT)because administering estrogen alone would cause estrogen to go unopposed and potentially cause endometrial hyperplasia/cancer
question
What would I use for a women in menopause that does not have a uterus and why?
answer
Estrogen Replacement Therapy (ERT) - no risk of hyperplasia/cancer if all the plumming is gone
question
This is the First PROSPECTIVE RANDOMIZED CONTROLLED trial evaluating estrogen therapy Sponsored by the National Institutes of Health (NIH) Women ages 50-79 scheduled to be completed in 2005
answer
Women's Health Initiative (WHI)
question
Based on WHI, what is the mosot effective "the bomb" for treating vasomotor symptoms?
answer
HRT most effective treatment for vasomotor sx (use the smallest does for the shortest period of time)
question
What does ACOG say about how to administer HRT?
answer
1. If HRT, then smallest dose for shortest time (preferably < 4 years) 2. Long-term rx should be stopped in asymptomatic pts (taper helps decrease rebound sxs)
question
What are alternatives to HRT?
answer
1) SSRIs (consider adding while HRT taper) - Venlafaxine (Effexor) 75-150mg po bid - Paroxetine (Paxil) 20mg po qd - Fluoxetine (Prozac) 20mg po qd - Sertraline (Zoloft) 50mg po qd 2) Gabapentin (Neurontin) 300-900mg po qd 3) Clonidine (Catapres) 0.05-2mg po qhs/patch
question
Do herbals have significant data for treatment of menopausal symptoms?
answer
NO
question
What are the herbals that are used?
answer
1) Phytoestrogens 2) Soy isoflavones 3) Red clover isoflavones 4) Black cohosh 5) Dong Quai 6) Evening primrose oil 7) Bellergal-S 10) Wild yam and progesterone creams
question
What are the Vulvovaginal symptoms associated with menopause?
answer
1) Dyspareunia 2) Atrophic vaginitis 3) Urinary symptoms - Frequency/dysuria - Incontinence - Frequent UTIs
question
What causes the vulvovaginal symptoms associated with menopause?
answer
Lack of estrogen results in vaginal atrophy with an alkaline pH
question
What is the best treatment for vulvovaginal symptoms?
answer
Vaginal estrogen as cream, suppository or ring
question
Can Oral estrogen/transdermal estrogen be used for the treatment of vulvovaginal symptoms?
answer
Yes, but topical is better
question
This is the Deterioration of trabecular bone tissue leading to decreased bone mass, fragility, and increased fracture risk
answer
Osteoporosis
question
How does the World Health Organization (WHO) define osteoporosis?
answer
1) Bone mineral density (BMD) >2.5 standard deviations (SD) below the mean is osteoporosis 2) Bone mineral density (BMD) >1.0 but <2.5 SD below the mean is osteopenia
question
When does bone grow?
answer
From birth until age 35
question
How long is bone mass preserved?
answer
Until Menopause
question
When is there rapid bone loss?
answer
In the first few years
question
Women live longer so what does this mean?
answer
1) 40% of women >50yo will fracture due to osteoporosis! - 2-3x higher than men 2) Vertebral fx 15 yr prior to hip—sentinel event Hip fx 20% mortality 1st yr
question
What are the three most common fracture locations in order of frequency?
answer
1) Vertebrae (Anterior) -MOST COMMON (90% will fracture again in 12 months) 2) Hip 3) Distal radius
question
What are the Clinical Risk Factors for Osteoporotic Fracture (independent of BMD)
answer
1) **Advancing age 2) **Previous history of fragility fracture as adult 3) History of fragility fracture in 1st degree relative 4) Low body weight (<127lb) 5) Current smoking 6) Glucocorticoid therapy 7) Excessive use of alcohol 8) Rheumatoid arthritis
question
How is a patient screened for osteoporosis?
answer
Dual-energy x-ray absorptiometry (DEXA)
question
What does the Dual-energy x-ray absorptiometry (DEXA) measure?
answer
Spine/Hip
question
Who should undergo a Dual-energy x-ray absorptiometry (DEXA)?
answer
1) 50 year-olds with 1 or more risk factors (besides menopause) - Advancing age - Previous history of fragility fracture as adult - History of fragility fracture in 1st degree relative - Low body weight (<127lb) - Current smoking - Glucocorticoid therapy - Excessive use of alcohol - Rheumatoid arthritis 2) All 65 year-olds
question
What are the two scores that come from a DEXA scan?
answer
1) T score 2) Z score
question
What does the T score measure?
answer
It compares Bone Mineral Density to "normal" young adult
question
What does the Z score measure?
answer
It compare Bone Mineral Density with same age and weight
question
Can a patient be diagnosed with osteoporosis without a DEXA scan?
answer
Yes. Fragility fracture regardless of BMD
question
What are the 2 indications for a DEXA scan?
answer
2 indications for DEXA scan include 1) Screening 2) Monitoring drug therapy
question
Accordinf to DEXA Scan, Osteopenic =
answer
Not severe enough to be called ostreoporosis Bone mineral density (BMD) >1.0 but <2.5 SD
question
Osteoporosis =
answer
>2.5 standard deviations (SD) below the mean is osteoporosis
question
How can my patient prevent osteoporosis?
answer
1) Nutrition - Calcium 1000-1500mg po daily - Vitamin D at least 800 IU po daily 2) Weight bearing exercise (also promotes balance) - 20-30 minutes 3x/wk 3) Avoid: Tobacco and ETOH
question
What are two ways to prevent fractures?
answer
1) Reduce Falls Risk 2) Treat Osteoporosis
question
What can my patient reduce fall risk?
answer
1) Vision assessment 2) Lighting 3) Clean, well-marked stairs and floors 4) Footwear 5) Hip pads
question
What are ways to prevent osteoporosis?
answer
1) Menopausal women T-score >-2.5 SD 2) Menopausal women T-score -2.0 to -2.5 SD (osteopenic) plus 1 additional risk factor for fracture
question
What are the drugs to treat osteoporosis?
answer
1) Hormone Replacement Therapy (HRT) 2) Estrogen Replacement Therapy (ERT) 3) SERMs 4) Bisphosphonates 5) PTH-Parathyroid Hormone 6) Calcitonin
question
This drug to treat osteoporosis is described as the following: 1) Agonist at bone 2) Antagonist at breast/endometrium 3) Worsens vasomotor symptoms (Because they act like estrogen) 4) Prevents vertebral fractures 5) Lack of data for hip fractures 6) Inhibit bone resorption
answer
Selective Estrogen Receptor Modulators(SERM)
question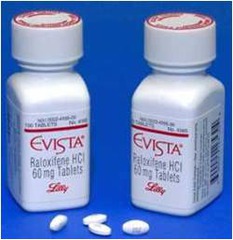
What is an example of Selective Estrogen Receptor Modulators(SERM)?
answer
Raloxifene (Evista)
question
What is the treatment of choice for osteoporosis?
answer
Bisphosphonates
question
What are the indications for Bisphosphonates?
answer
1) Osteoporosis prevention - Osteopenia + Risk factor 2) Osteoporosis treatment Treatment of choice
question
What are the contraindications for Bisphosphonates?
answer
1) Esophageal dysmotility 2) Inability to be upright x 30min 3) Hypersenstitivity 4) Hypocalcemia
question
Do Bisphosphonates build bone?
answer
Yes
question
What are the complications of Bisphosphonates?
answer
1) Erosive esophagitis 2) Jaw Osteonecrosis
question
Because of the risk of erosive esophagitis with Bisphosphonates, what must be done?
answer
Esophagitis—must administer medication in the AM, with water only, and remain upright for 30 minutes afterward.
question
What are the second line therapies for osteoporosis?
answer
1) Parathyroid hormone (PTH) 2) Calcitonin
question
This drug is described as the following: 1) Stimulates both osteoblasts & osteoclasts - Blasts>>Clasts resulting in improved bone mass 2) Convenient q28 day auto-injector 3) Only requires 18-24 months of therapy 4) Expensive
answer
Parathyroid hormone (PTH)
question
Parathyroid hormone (PTH) seems an unlikely candidate for the treatment of osteoporosis because of its well-described deleterious effect on bone. So why does it work?
answer
Intermittent administration of recombinant human PTH (both full-length 1-84 or fragment 1-34) stimulates bone formation more than resorption.
question
This drug is described as the following: 1) Inhibits osteoclasts 2) Unique indication as the most effective for osteoporosis fracture pain (vertebral) 3) Nasal spray 200 IU daily in alternate nostrils 4) Expensive
answer
Calcitonin - Not much effect on BMD - Doesn't decrease fracture risk
question
How is osteoporosis monitored?
answer
1) Repeat DEXA scans every 2 years 2) Bone metabolism markers at 6 months - Serum CTX (carboxy-terminal collagen crosslinks) - Urinary NTX (cross-linked N-telopeptides)
question
T or F. 15% of women continue to lose BMD despite therapy
answer
True
question
How is perimenopause defined?
answer
2-8yrs preceding menopause
question
Inhibin B concentrations increase or decrease due a decline in follicle number? What happens to FSH values?
answer
Inhibin decreases and FSH increases
question
High _____ and low ______ values are suggestive of menopause but not confirmatory
answer
High FSH and Low Estrogen
question
Why does the probability of having dizygotic twins peak around 37?
answer
b/c during perimenopause follicles develop more rapidly in response to increased FSH
question
At what age does fertility begin to decline?
answer
Age 29
question
What is the major source of estrogen in menopausal women?
answer
the conversion of androstendione to estrone (estrone is a less potent estrogen than estuarial)
question
Endometrial hyperplasia can be a prerequisite to what?
answer
endometrial cancer
question
What testing technique needs to be performed if you suspect endometrial hyperplasia?
answer
Endometrial biopsy
question
What diagnostic study is used to measure the thickness of the endometrium?
answer
transvaginal US (normal <5mm)
question
What is vaginal dryness/atrophy due to?
answer
an deficiency in estrogen which causes thinning of the vaginal epithelium
question
Estrogen therapy doe not appear to be effective for the treatment of......
answer
urinary incontinence
question
What are 3 common physical findings in a menopausal woman?
answer
1. pale vagina 2. loss of normal rugae 3. vaginal pH 6.0-7.5
question
What are 2 factors that are strong predictors if menopausal woman will experience depression?
answer
Prior hx of depression or PMS
question
What are the 3 long-term issues resulting from menopause?
answer
1. Osteoporosis 2. Cardiovascular disease 3. Dementia
question
Define Menopause
answer
12 months of amenorrhea in women over age 45 in the absence of other biological or physiological causes
question
What do follicles produce less of after age 40?
answer
Inhibin
question
_____ has an inverse relationship with ______
answer
FSH; Inhibin
question
What should always be included on the DDx in a women with amenorrhea?
answer
Hyperthyroidism/thyroid disorder
question
What is the best approach to diagnosing the menopausal transition?
answer
longitudinal assessment of menstrual cycle history and menopausal symptoms
question
Are serum FSH, estradiol, or inhibin levels useful for diagnostic purposes?
answer
NO!
question
What are the advantages of OCP with perimenopausal symptoms?
answer
Prevention of ovarian/endometrial cancer Reduction of benign breast disease Improved bone density Control of erratic vasomotor symptoms Stabilizing of irregular bleeding
question
Oral contraceptive SHOULD NOT be used in what population?
answer
Women over 35yrs who SMOKE
question
What are other contraindications of OCPs?
answer
Active liver disease/hepatitis Deep vein thrombophlebitis Breast Cancer
question
OCPs until age _____ if no contraindications
answer
51yrs
question
Check _____ on day 5-7 in pill free wk
answer
FSH
question
FSH >_____ = menopausal
answer
25 --> switch to HRT
question
4 indications for HRT
answer
1. osteoporosis prevention and treatment 2. urogenital atrophy/dryness 3. vasomotor symptoms 4. if symptomatic after oophorectomy
question
HRT is NO LONGER used for prevention of what?
answer
Coronary Artery Disease
question
Hormonal therapy should be limited to the __________ duration and __________ dose
answer
shorted duration and lowest dose
question
What are the 8 absolute contraindications to HRT?
answer
1. Endometrial carcinoma 2. Estrogen dependent tumor 3. Unexplained vaginal bleeding 4. Recent MI 5. Recent thromboembolic event 6. Stroke 7. Pancreatic disease 8. Active gall bladder disease
question
What are some relative contraindications to HRT?
answer
HTN atypical breast lesions DM Hx of gall bladder dz Migraines endometriosis Fibrocystic breast dz Uterine fibroids obesity seizures hx of DVT or PE
question
Vaginal Cream (Premarin, estrace, ogen), E-string, Vagifem, Femring are all examples of what?
answer
Vaginal estrogen
question
How often is the E-strong replaced?
answer
every 3 months
question
If using the femring what needs to occur id woman has intact uterus?
answer
need to add progesterone
question
When progestins are added to estrogen if uterus is intact what rates are lower?
answer
endometrial hyperplasia and carcinoma
question
What are the 6 contraindications to progestins?
answer
1. breast cancer 2. undx vaginal bleeding 3. chronic liver disease 4. thromboembolism 5. pregnancy 6. gall bladder disease
question
Prometrium is a type of what?
answer
Natural progesterone
question
What is important to know about pt if prescribing promethium?
answer
CHECK if have peanut allergy
question
Medroxypregesterone acetate (Provera), Northindrone, Levonorgesrol are examples of what?
answer
synthetic progestins
question
Name 2 non-systemic progestins
answer
Mirena IUD Crinone (suppositories)
question
Activella, Prempro, Climarapro Patch, Combipatch are examples of what?
answer
Low dose estrogen/progesterone combination product
question
Vivelle dots, Climara, Estraderm, Menostar patch, Femring, Divigel, Evamist are examples of what?
answer
Hormone patches, rings, gels, and sprays (bypass the liver when metabolized)
question
Name the 3 preventions for osteoporosis
answer
1. 1500mg Calcium daily 2. 800-1000IU Vit D daily 3. Weight bearing exercises
question
What are the 3 alternatives to hormone therapy for prevention/treatment of osteoporosis?
answer
1. SERMs (Selective Estrogen Receptor Modulators) 2. Bisphosphonates 3. Parathyroid hormone
question
Ralofexine is an example of?
answer
SERM
question
What are the 2 negative symptoms that SERMs cause?
answer
Hot flashes and increased risk of blood clots
question
Aledronate and Risedronate are examples of?
answer
Bisphosphonates
question
Bisphosphonates may cause...
answer
esophageal irritation
question
Estroven and Ramifemin are examples of what?
answer
Black Cohash
question
What is the only OTC FDA approved med for hot flashes?
answer
Black Cohash (Remifemin/Estroven) - 20mg bid
question
Red Clover, Mexican yam effect on hot flashes?
answer
no real good evidence
question
Freshly ground flaxseed or linseed is indicated in what 2 symptoms?
answer
Hypercholesterolemia Hot Flashes
question
Define post-menopausal bleeding
answer
bleeding that occurs after 12months of amenorrhea
question
Post-menopausal bleeding cannot be associated with ....
answer
HRT (or may be prolonged/heavy if associated with HRT)
question
All methods of HRT may yield....
answer
bleeding
question
How long will most women bleed when placed on HRT
answer
3mos
question
2 Population of pts using HRT that need evaluation...
answer
1. on HRT for 6mos and bleeding 2. Pts with intact uterus on unopposed estrogen
question
Menopause is the cessation of periods for how long?
answer
the cessation of menstrual periods for 12mos
question
at what age does our fertility start to decline?
answer
29yrs old
question
at about what age does menopause occur?
answer
51.4 years in normal women
question
By 2020, how many million women in US will be menopausal
answer
60M
question
Life expectancy is 84.5 yrs, women will live ? more years after menopause
answer
~30
question
When is perimenopause?
answer
Defined as the 2-8 years preceding menopause Ends one year after the last menstrual period
question
Can menstrual irregularities occur during perimenopause?
answer
Yes, Ovarian function waxes and wanes, Less frequent ovulation, Normal cycles are interspersed with anovulatory (estrogen-only) cycles [this is when women at 50 get prego by accident] Irregular menses, breakthrough bleeding, DUB
question
T/F, During perimenopause there are fluctuations in serum conc of FSH and estradiol
answer
True
question
During perimenopause, which out of the following rise? Inhibin B, FSH, progesterone
answer
FSH
question
T/F High FSH and low estradiol values may be suggestive of menopause but not confirmatory
answer
True also note: A single serum FSH value in the postmenopausal range, even with undetectable estradiol levels does not provide reliable evidence that menopause has occurred.
question
perimenopause follicular phase abnormalities are prevalent at what yr of age?
answer
40
question
perimenopause follicular phase abnormalities: does the phase shorten or lengthen?
answer
shorten
question
During perimenopause, follicular phase abnormalities such as irregular cycles, follicular phase shortening, and residual follicle units # only in thousands, are prevalent at what age?
answer
40yo
question
Follicles develop more rapidly in response to increased FSH, dizygotic twinning peaks at 37! So FSH is higher, what is going on w/ estradiol?
answer
It levels at mid cycle and in the luteal phase are lower
question
Ovarian follicles are depleted during perimenopause, and the ovary no longer secretes what hormone?
answer
Estradiol
question
During perimenopause, Ovarian production and secretion of androgens continue, and where is the major source of estrogen in menopausal women?
answer
conversion of androstendione to estrone. Estrone is a less potent estrogen than estradiol.
question
What kinds of disorders can declining ovarian function lead to?
answer
ovarian d/o: functional ovarian cysts, hemorrhagic cysts. (Diagnosis of these disorders may be achieved using ultrasound, laparoscopy or laparotomy.)
question
What are the symptoms of menopause?
answer
Breast pain Hot flashes Migraines -headaches may worsen in frequency and intensity during the menopausal transition Skin changes Joint pain or stiffness Impaired balance Or no symptoms at all!
question
What are Potential Clinical Manifestations of Menopause?
answer
Change in bleeding patterns Vasomotor symptoms [hot flashes, variable as well] Sleep disturbance [insomnia often earliest sx] Genitourinary symptoms -Vaginal dryness/urogenital atrophy-dyspareunia Sexual dysfunction Depression Long-term issues -Osteoporosis -Cardiovascular disease -Dementia
question
Potential Clinical Manifestations of Menopause: what are potential Changes in Bleeding Patterns?
answer
Anovulatory bleeding/Chronic anovulation Oligomennorhea (lasting 6mos or more) Heavy dysfunctional uterine bleeding (DUB)
question
What is the Anovulatory bleeding/Chronic anovulation d/t?
answer
-due to progesterone deficiency -long periods of unopposed estrogen exposure can cause anovulatory bleeding
question
What diagnostics should be performed for the changes in bleeding patterns?
answer
Endometrial biopsy should be performed for the above persistent conditions to rule out endometrial hyperplasia, which can be a prerequisite to endometrial cancer. Transvaginal ultrasound can also be performed to evaluate the thickness of the endometrium (normal thickness is < 5mm)
question
What is the most common acute change during menopause?
answer
vasomotor sx's: Sleep disturbance secondary to hot flashes. -fatigue, irritability, depression, difficulty concentrating
question
up to what percent of women in some cultures experience hot flashes?
answer
75%
question
What percent actually seek medical attention?
answer
20%
question
Are hot-flashes self-limited? whats the pathophys?
answer
yes; unknown
question
What is Vaginal dryness/urogenital atrophy d/t?
answer
Due to estrogen deficiency causing thinning of the vaginal epithelium and vaginal atrophy
question
Can yo do stuff about vaginal dryness/atrophy?
answer
Yes! [lubrication can be helpful. If lost rugae, have to put estrogen in there and using vaginal estrogen cream is very helpful and its localized (low systemic abs)! talk to women about these options in perimenopause yrs]
question
Atrophic Vaginitis, Atrophic Urethritis Symptoms=
answer
sx's can include itching ,irritation and dyspareunia (painful intercourse) [on exam, vagina will have lost its rugae, making sex uncomfortable, looking pale and dry]
question
what can Atrophic Vaginitis, Atrophic Urethritis predispose to?
answer
May predispose to both stress and urge urinary incontinence Although data are conflicting, estrogen therapy does not appear to be effective for the treatment of urinary incontinence.
question
Are recurrent UTI's a clinical manifestation of menopause?
answer
yes!
question
What do you see on exam of GU system?
answer
-Pale vagina -Lack of the normal rugae (vaginal folds) -Vaginal pH 6.0 to 7.5 (<4.5 in the reproductive years) -Increase in pH and vaginal atrophy may impair protection against vaginal and urinary tract infection
question
What are manifestations of menopause concerning sexual dysfxn?
answer
Decreased vaginal lubrication -Estrogen deficiency -Decrease in blood flow to the vagina and vulva -Vaginal dryness and dyspareunia Decrease in elasticity of the vaginal wall Shortening and narrowing of the vaginal vault Continuing sexual activity may prevent these changes! Responsive to estrogen therapy -? Decreased sensation in the clitoral and vulvar area
question
Is depression associated with menopause?
answer
Yes! Prior history of depression or PMS-strong predictor: Characterized by frequent mood changes, irritability, nervousness Depression during the perimenopausal years Nonhormonal events -aging parents -empty nest -chronic illness, and physical limitations
question
Long term issues of menopause
answer
-Osteoporosis [estrogen can be used to tx osteoporosis, not first line, but if have other indications it can improve menopause sx's too] -Cardiovascular disease [risk more than doubles at menopause] -Dementia [seen w/ inc freq. with low estrogen levels]
question
Woman over age 45 in the absence of other biological or physiological causes, do you want further diagnostic evaluation?
answer
No further diagnostic evaluation for women in this group! Measuring serum FSH, estradiol, or inhibin levels unnecessary
question
Women <45 years with irregular periods or amenorrhea, blood work? hx Q's?
answer
Blood work for HCG, prolactin, TSH, FSH Assessment/History- A good history is important -menstrual cycle history -menopausal symptoms vasomotor flushes, vaginal dryness -[wt changes will change period, stress levels will]
question
Making the dx of menopause, labs?
answer
FSH inverse relationship with Inhibin Follicles produce less Inhibin after age 40 FSH rises note: Postmenopausal response to hormone therapy cannot be monitored by measuring FSH Suppression of FSH persists due to lack of inhibin.
question
ddx of amenhorrhea?
answer
-Hyperthyroidism/ thyroid disease Irregular menses, sweats, mood changes -Pregnancy -Hyperprolactinemia -Atypical [more freq] hot flashes and night sweats -Medications -Malignancies -Carcinoid -Pheochromocytoma
question
Treatment of Perimenopausal Symptoms [anyone in 40s 50s]
answer
Oral contraceptives
question
What are advantages of using OCPs?
answer
Prevention of ovarian cancer and endometrial cancer Reduction of benign breast disease -30% reduction fibrocystic disease -60% reduction fibroadenomas, 40% other lumps Decrease dysmenorrhea, mittleschmertz [unilateral lower ovarian pain], menorrhagia and anemia Improved bone density - women lose 8-10% of bone mass from age 35-50, OC use counters the premenopausal losses Control of erratic vasomotor symptoms Stabilization of irregular bleeding
question
What is the big Oral contraceptives CAUTION (for tx of perimenopausal sx's)?
answer
Do not use use if over 35 years old and smoking [inc risk for DVT big time and coagulopathy in general] Contraindications including but not limited to: Active liver disease/hepatitis Deep vein thrombophlebitis Breast Cancer
question
Transitioning From OC's to HRT, what is basically the difference?
answer
the dose, [the dose of HRT is significantly smaller than OCP's]
question
What kinds of things are you looking at when switching from OCP's to HRT?
answer
OC's until age 51 if no contraindications Check FSH in day 5-7 of pill free week FSH over 25, probably menopausal Switch to HRT No data support risk benefit or cost benefit of this approach Can switch w/o testing at age 50
question
Indications for HRT
answer
Osteoporosis prevention and treatment Urogenital atrophy-vaginal dryness Vasomotor symptoms [estrogen is really the only thing that helps this] If symptomatic after oophorectomy, (removal of ovaries)
question
Benefits of Estrogen
answer
-Decreases hot flashes -Improves bone mineral density (BMD) -Decreases fracture risk -Improves sexual function -Improves symptoms of vaginal atrophy -Decreases risk of colon cancer Possible benefits -Improves mood, libido -Decreases skin aging -Decreases incontinence -Reduced osteoarthritis -Prevents cataracts -Prevents macular degeneration
question
What were the outcomes of the world health initiative study that investigated long-term benefits and risks of HRT? What was the major problem with the study?
answer
Primary : Coronary heart disease (CHD) and invasive breast cancer Secondary : stroke, pulmonary embolism, DVT, endometrial CA, colorectal CA, hip and vertebral fractures and death from other causes -potential risks outweighed benefits the prob: avg age at enrollment =63yo so that's one problem, on avg 12yrs postmenopausal when entrolled, most hadn't been put on estrogen previously and were put on it for first time and that ultimately was the problem.
question
What did follow up studies show?
answer
within 5yrs it is safe to use estrogen therapy as far as CV risk, but if farther out then if >5yrs out then higher CV risk. So it should be safe and actually be CV beneficial if women are within 5yrs of menopause and have no other significant risk factors for CV dz. [controversial topic, depends on doc, on pt]
question
**Hormone therapy should be limited to what duration and what dose? [shortest/longest and lowest/highest?]
answer
Shortest duration and Lowest dose
question
WHIMS: World health initiative memory study Designed to evaluate postmenopausal estrogen and progesterone and its effect on the reduction of the risk of dementia in women over age 65foudn what?
answer
HRT and cognitive function: no clinically significant difference in either group
question
What are Absolute Contraindications to HRT ?
answer
Endometrial carcinoma Estrogen dependent tumor Unexplained vaginal bleeding Recent myocardial infarction Recent thromboembolic event Stroke Pancreatic disease Active gall bladder disease
question
What are some relative contraindications to HRT? Things you have to consider benefits/risks for the pt
answer
Hypertension atypical breast lesions diabetes mellitus Hx of gall bladder disease or stones migraines endometriosis fibrocystic breast disease Uterine fibroids obesity seizures past history of deep venous thrombosis or PE
question
What's the perspective Tana wants us to remember in regards to breast cancer?
answer
The risk of breast cancer published by the WHI is smaller than with other risk factors known to be associated with breast cancer. The increased risk of breast cancer attributed to being overweight after menopause is greater risk. "We can say with confidence hormone users who develop breast cancer have better outcomes then those not on hormones". Leon Speroff M.D., Professor Ob/Gyn This may be due to the fact that they have yearly clinical breast exams and mammograms.
question
For many newly menopausal women with moderate to severe symptoms, do benefits will outweigh risks?
answer
Yes [they will get so much sx relief from hormones and the risks are low]
question
What are the diff types of Vaginal Estrogen? [for vaginal dryness, inc UTIs, etc] [Tana loves this!!]
answer
Vaginal cream- Premarin, Estrace, Ogen [can be messy] E-string-Estradiol ring inserted in the vagina Changed every three months [not as messy too] Vagifem-Preloaded applicator vaginal tabs [Tana uses this] Femring 0.05/0.1- Placed vaginally Systemic absorption, add progesterone with intact uterus
question
When is progestin added to estrogen? why?
answer
when uterus intact Lower rates of endometrial hyperplasia lower rates of endometrial carcinoma no increase in benign breast lesions
question
Contraindications to Progestins
answer
Breast cancer Undiagnosed vaginal bleeding Chronic liver disease Thromboembolism Pregnancy Gall bladder disease
question
Progestins: Systemic Preparations
answer
Natural Progesterone -Prometrium- micronized peanut oil base- check peanut allergy! -Crinone 4% and 8% suppositories, Common Synthetic -Medroxyprogesterone acetate (Provera) -Norethindrone -Mirena IUD- levonorgesrol [not typically used postmenopausally but perimenopausally is a nice option]
question
Progestational SE's
answer
BLEEDING Over progesteronization of uterine lining Atrophy Continuous spotting PMS SYMPTOMS Depression/ Anxiety Other mood changes Bloating HA MASTODYNIA Prometrium contraindicated if peanut allergy!
question
Progestin Non Systemic products that are available:
answer
Mirena IUD, Crinone (many combo products available as well)
question
Hormone Patches, Rings, Gels and Sprays.
answer
Provide other alternative Bypass the liver when metabolized Examples: Vivelle dots Climara/ ClimaraPro Estraderm .05, 0.1 mg/day estradiol Menostar patch 14 mcg/day estradiol Approved for the prevention of osteoporosis Combipatch Femring Divigel, EstraGel Evamist
question
Bioidentical hormones considerations?
answer
Custom-made by a compounding pharmacy Not FDA controlled Plant derived Identical safety issues to other prescription hormones No scientific evidence to support claims of increased efficacy or safety No Black box warning [a lot of variability in these]
question
T/F Postmenopausal hormone therapy (HT) should not be initiated or continued for the prevention of cardiovascular disease or other chronic diseases at any age
answer
True
question
T/F HT still has a clinical role in the treatment of moderate to-severe hot flashes and other menopausal symptoms. The lowest effective dose should be used for the shortest duration necessary.
answer
True
question
T/F Additional research on the benefits and risks of HT initiated early in menopause is not warranted.
answer
False
question
Preventative Health Care for women in perimenopause
answer
Pap smear, blood pressure, height Breast cancer screening (CBE, mammogram) Other health screenings as indicated, bone density, blood work Vision, heart disease and diabetes risk assessment Colon cancer screening Vaccinations as indicated
question
Lifestyle changes for perimenopausal women
answer
Addressing use of tobacco, alcohol and other substances Obesity and Physical Activity Adequate Sleep Nutrition Sexuality Spiritual Health
question
Alternatives to Hormone TherapyFor Prevention of Cardiac Disease
answer
Quit smoking Exercise High fiber/Low fat diet Control high blood pressure Manage coexisting medical problems like Diabetes Possibly Aspirin therapy
question
Alternatives to Hormone TherapyFor Prevention / Treatment of Osteoporosis
answer
-Calcium intake 1500 mg daily -Vitamin D 800-1000 IU daily. Enhances calcium absorption -Weight-bearing exercise regularly -SERMS [but do cause hot flashes so careful in perimenopausal women] -Bisphosphonates
question
Alternatives to Hormone Therapy: Prevention of Hot flashes
answer
Lifestyle changes -Avoid hot spicy foods -The layered look -Lower thermostat -Exercise -Relaxation, biofeedback Over-the-counter remedies -Soy [estrogenic, may improve bone density], Phytoestrogens [may help] -Dong Quai -Black Cohash -Remifemin, Estroven FDA approved, mildly effective for hot flashes -Red clover maybe, Mexican Yam?, Flaxseed [good for lowering cholesterol] or Linseed Prescription -Clonidine patch: blood pressure medicine [not best choice dont want to give orthostatic HoTN] -Antidepressants: SSRI's ie Effexor, Paxil -Neurontin (Gabapentin) [anecdotally not helpful or used really]
question
Is there convincing evidence that soy foods are connected to breast cancer?
answer
No
question
What is the one herb that's been tested and proven to be mildly effective in reducing hot flashes?
answer
Black Cohosh
question
Criteria for post menopausal bleeding
answer
-Bleeding that occurs after 12 months of amenorrhea (Excluding pregnant and breast-feeding women) - Post Menopausal Bleeding not associated with hormone replacement -Prolonged (10-14 days) or heavy bleeding associated with hormone replacement -Bleeding associated with non-phasic hormone replacement after 3-6 months
question
All methods of HRT may yield
answer
bleeding-Breakthrough bleeding ranges from 10-40%. Most women will bleed the first three months [should happen after 6mos] Vaginal administration of estrogen for urogenital symptoms of estrogen deficiency may rarely stimulate the endometrium Unopposed oral estrogen (without progesterone) in women with a uterus can cause hyperplasia and endometrial carcinoma
question
Post Menopausal Bleeding: Patients Using HRT Needing Evaluation
answer
-On hormones for 6 months or more and bleeding -Patients with intact uterus on unopposed estrogen Yearly endometrial biopsies Transvaginal ultrasounds check endometrial stripe
question
Cyclical Combined HRT: Bleeding OK if cyclic?
answer
Yes, Evaluate only if bleeding is irregular, prolonged or heavy
question
How do you evaluate pts using HRT on hormones for 6mos or more & bleeding, or pts with intact uterus on unopposed estrogen?
answer
Yearly endometrial biopsies Transvaginal ultrasounds check endometrial stripe
question
If a pt is on a cyclical combined HRT, is bleeding ok?
answer
Only if it is cyclic! Evaluate only if bleeding is irregular, prolonged or heavy
question
Case 1: 35 yo G1 P0101 female is here for her annual exam and c/o hot flashes and amenorrhea for 12 months. She doesn't know why she is not having periods and her hot flashes are disruptive to her sleep and daily activities. DDx Tests
answer
[pregnancy, early menopause, US?] [maybe we can just talk thru these?]
question
Case 2: 45 yo G2 P2002 female presents with c/o hot flashes and irregular menses (q 3-5 mos) for the past 9 months. She smokes ½-1 ppd cigarettes and would like to quit. DDx Tests
answer
...
question
Case 3: 65 yo Asian female presents to your office to start HRT. She heard it would help protect her heart, make her feel younger and help her memory. She went through menopause 10 years ago and has not had any problems except an occasional hot flash. She is 5'4", 108 lbs. Her history is significant for a wrist fx 2 yrs ago. She takes calcium faithfully.
answer
[no sx's and it only helps protect heart if taken within 5yrs of menopause..?]
question
Case 4: 49 yo female c/o unbearable hot flashes.. She can't sleep very well and wakes up 3 times a night drenched in sweat. She has a high power job as a CEO and symptoms are effecting her job performance. Her PMH is significant for breast cancer 2 years ago. How can you help alleviate her symptoms and improve her quality of life?
answer
...
question
Case 5: 53 yo began continuous HRT 4 wks ago. She is now having some vaginal spotting after being amenorrheic for 14 months. She is concerned. DDX Tests
answer
...
question
menopause occurance
answer
begins earlier for smokers, mean is age 51
question
risk assessments
answer
cardiovascular, osteoporosis
question
FSH
answer
over 40 =menopause
question
symptoms
answer
dry skin, dry eyes, dry vagina, irregular periods, hormonal instibility,
question
first risk of menopause
answer
cardiovascular risk d/t lipid solubility changes
question
second risk of menopause
answer
osteoporosis, loss of bone density, risk for fracture
question
highest risk for OP
answer
thin, white smoker lack of exercise, low calcium, high caffeine intake
question
PPI for gerd
answer
give Calcium Citrate
question
vitamin D
answer
recommendations: 800-1200units daily test vit d, 25 hydroxy vit d
question
OP labs
answer
serum ca, creatinine, 25hydroxy vit d, alk phos, celiac panel, TSH, testosterone, 24hr urine ca, na, cr.
question
Perimenopausal
answer
do not write for hormones- can still get pregnant! Enc mirena IUD, low dose OCP
question
prometrium (progestine)
answer
makes drowsy, so it treats insomnia, take with estrogen made from soy, not for pt with nut allergy
question
Menopause definition
answer
Permanent cessation of menses resulting from diminishing ovarian follicular function demonstrated by 12 consecutive months of amenorrhea.
question
Median age of menopause onset
answer
51 years (range 40 - 55)
question
Perimenopause definition
answer
AKA menopausal transition time - time before menopause and the first year following menopause
question
Symptoms of perimenopause related to declining estrogen
answer
Anovulation Dysfunctional uterine bleeding Extended menstrual cycle intervals Oligomenorrhea
question
Sx of menopause directly related to LACK of estrogen
answer
Vaginal dryness Vulvar/vaginal atrophy Vasomotor sx (night sweats, hot flashed)
question
Sx associated with menopause w/o a proven link to estrogen deficiency
answer
Arthralgia Depression Insomnia Migraines Mood swings Myalgia Urinary frequency Cognitive changes (memory, concentration)
question
During menopause FSH and LH INCREASE/DECREASE
answer
Increase
question
During menopause estradiol and progesterone INCREASES/DECREASES
answer
DECREASE
question
During menopause what is the primary estrogen available?
answer
Estrone not estradiol
question
How is estrone primarily made?
answer
Converted peripherally from andostenedione and is less potent
question
How must a menopausal woman with an intact uterus be treated?
answer
Estrogen+progestin to reduce the risk of endometrial hyperplasia and endometrial cancer
question
How must a menopausal woman who has had a hysterectomy be treated?
answer
Unopposed estrogen
question
Contraindications to estrogen replacement therapy (ERT)
answer
1. Abnormal / undiagnosed genital bleeding 2. Breast cancer (hx/suspected/known) 3. Hx of DVT or PE 4. Estrogen dependent neoplasia 5. Pregnancy 6. Stroke or MI in the past year 7. Liver dysfunction / disease
question
Estrogen and progestin MoA
answer
ERT, alone or w/progestin, replaces diminished levels of endogenous hormones Combined estrogen-progestin therapy includes progestin to prevent endometrial hyperplasia and cancer
question
When should a pt on HRT (hormone replacement tx) contact her dr.?
answer
1. Unusual vaginal bleeding 2. Abdominal tenderness, pain, swelling 3. Coughing up blood 4. Disturbances of vision or speech 5. Dizziness or fainting 6. Lumps in breast 7. Numbness or weakness in armo ro leg 8. Severe vomiting or HA 9. Sharp chest pain or shortness of breath 10. Sharp pain in the calves
question
Severe adverse drug events of HRT
answer
1. Risk of thromboembolism, stroke, coronary heart disease, breast cancer (identified by Women's Health Initiative Trial)
question
Benefits of HRT
answer
Reduced fractures Reduced colorectal cancer
question
Most common adverse drug events of estrogen
answer
1. Breast tenderness 2. Heavy / irregular bleeding 3. HA 4. N
question
Most common adverse drug events of progestin
answer
Depression HA Irritability
question
Estrogen drug-disease interactions
answer
Estrogen may make the following worse: 1. Depression 2. Hypertriglyceridemia (avoid TD product) 3. Thyroid disorder (increase in thyroid supplement) 4. Impaired hepatic function 5. CVD disorders 6. Colethiasis 7. GERD
question
Estrogen drug-drug interactions - drugs that DECREASE estrogen effect
answer
Decreases in estrogen effect caused by 1. CYP 3A4 inducers 2. Barbiturates 3. Rifampin 4. St. John's wort 5. Phenytoin
question
Estrogen drug-drug interactions - drugs that INCREASE estrogen effect
answer
Increases in estrogen effect caused by 1. 3A4 inhibitors 2. Azole antifungals 3. Macrolide antibiotics 4. Ritonavir
question
HRT monitoring
answer
Sx improvement Adverse effects Appropriate health maintenance (annual mammograms)
question
List the oral estrogen only products (brand)
answer
Premarin Cenestin, Enjuvia Estradiol, estrace, gynodiol Estropiptate, Ortho-Est, Ogen Estratab, Menest
question
Brand Premarin
answer
Generic conjugate equine estrogens (CEE)
question
Brand Cenestin, Enjuvia
answer
Generic synthetic conjugated estrogens
question
Brand Estradiol, estrace, gynodiol
answer
Micronized estradiol
question
Brand Estropiptate, Ortho-Est, Ogen
answer
Estrone sulfate
question
Brand Estratab, Menest
answer
Esterified estrogen
question
List the transdermal (TD) HRT products (brand)?
answer
Estraderm, esclim, Alora, Vivell Climara, Fempatch, Menostar Climara Pro Combipatch Estrasorb Estrogel Evamist
question
How often are patch HRT products applied?
answer
Once - Twice weekly.
question
Which vaginal estrogen product has systemic absorption?
answer
Femring vaginal ring
question
Which HRT products contain estrogen and progestin
answer
Climara Pro Combipatch
question
List the oral estrogen progestin HRT combo products
answer
Activella Femhrt Prempro Premphase
question
List the combination estrogen-androgen products
answer
Estratest HS, covaryx HS Estratest
question
Angrogen (testosterone) for menopause MoA
answer
Androgens = precursor to estrogen production by the ovaries and peripheral sites Androgens act at receptor sites or are converted to estrogen
question
Androgen replacement improves which menopausal sx?
answer
Decreased libido Decreased energy Diminished well-being
question
Who can receive testosterone therapy during menopause?
answer
Only women who are also receiving estrogen therapy
question
List the relative contraindications to andorgen therapy
answer
Androgenic alopecia Hirsutism Moderate - severe acne
question
What are testosterone ADE's?
answer
Fluid retention Decreased HDL and TGs Hepatic dysfunction Hepatocellular carcinoma (prolonged use @ high doses)
question
What are phytoestrogens?
answer
Plant compounds (isoflavones, lignans, and coumestans).
question
What are food sources of phytoestrogens?
answer
Soy, edamame, tofu, flaxseed, alfalfa sprouts
question
Evidence for phytoestrogens
answer
Improvement in vaginal sx, decrease loss in bone density, lipids, weight, blood pressure
question
Evidence lacking for which sx for phytoestrogens?
answer
All other symptoms.
question
def of natural menopause?
answer
12 consecutive mo of amenorrhea with no obvious pathologic cause (usu 50+ y.o.)
question
def of induced menopause?
answer
bilateral oophorectomy or iatrogenic ablation of ovarian function causes permanent cessation of menstruation
question
def of perimenopause?
answer
few years before to 12 mo. after FMP when menstrual cycle and endocrine changes occur
question
def of premature menopause?
answer
<40 y.o., whether natural or induced
question
def of premature ovarian insufficiency?
answer
<40 y.o. leading to permanent or transient amenorrhea
question
def of early menopause?
answer
well before 51 y.o. but usually under age 45
question
def of early postmenopause?
answer
time period within 5y after FMP
question
primary indication for systemic HT at menopause?
answer
vasomotor sx (hot flashes, night sweats)
question
most effective tx for vaginal sx of menopause?
answer
estrogen therapy (local if vaginal sx are sole indication, plus then don't need progesterone challenge)
question
sexual function problems of menopause?
answer
dyspareunia (painful intercourse), diminished libido
question
what meds are helpful for sexual function problems of menopause?
answer
HT for dyspareunia, not effective for diminished libido
question
effect of HT on urinary health?
answer
systemic ET may worsen or provoke urge incontinence; local ET may reduce recurrent UTI risk; unclear if ET is effective for overactive bladder
question
HT effect on psych?
answer
- can improve QOL (better mood, fewer menopause sx); but not approved for this goal - progesterone can worsen mood w/hx of PMS or MDD
question
effect of HT on bone health during menopause?
answer
reduces postmenopausal osteoporosis and fractures, esp if initiated early on after menopause
question
what meds for bone health during menopause?
answer
HT for postmenopausal osteoporosis and fractures; bisphosphinates can be used if pts don't want HT but might have worsened bone quality and risk of weird fractures
question
effect of HT on CVD risk?
answer
- reduces CHD risk if initiated in younger women; longer tx leads to lower risk and mortality (but not primary indication for HT) - increases risk of ischemic stroke (not hemorrhagic) - VTE risk increases after initiation then decreases over time
question
effect of HT on diabetes risk?
answer
decreases new DM onset but inadequate evidence
question
effect of HT on endometrial cancer?
answer
unopposed systemic ET leads to higher endometrial cancer risk; if woman has uterus give progesterone challenge; if no uterus better to give ET alone
question
effect of HT on breast cancer?
answer
HT increases risk if used more than 3-5 yrs; incresaes cell prolif, breast pain, mammo density (harder to find tumors)
question
effect of HT on ovarian cancer?
answer
conflicting evidence
question
what cancers are known to be more likely in women on HT?
answer
- endometrial (if unopposed sys estrogen) - breast (if >3-5 yrs of use) - ovarian (conflicting evidence) - lung (may promote growth if hx of lung cancer)
question
effect of HT on lung cancer?
answer
if hx of lung cancer, HT may promote growth
question
effect of HT on cognition?
answer
increases dementia incidence if HT started >65y.o.; unclear if started early
question
effect of HT on ovaries?
answer
may be protective against premature ovarian failure
question
effect of HT on overall mortality?
answer
may reduce total mortality if started early; not if started >60y.o.
question
how to dose HT?
answer
- lowest effective estrogen dose; can add local ET if persistent vaginal sx - lowest progesterone exposure
question
what are bioidentical hormones?
answer
- custom-made HT formulations compounded at pharmacy according to provider - dose based on salivary hormone testing (may be unreliable)
question
what should be done prior to HT initiation?
answer
mammography within 12 mo
question
what happens if women on HT discontinue meds?
answer
50% chance of vasomotor sx recurring (regardless of whether tapered or abruptly discontinued)
question
What is Lichen sclerosus?
answer
chronic vulvar disorder usually seen in 5th or 6th decade. Thought to be an autoimmune response. porcelain-white papules and plaques (cigarette paper). NEED biopsy to confirm
question
What is Lichen planus?
answer
Inflammatory disorder most likely related to cell-mediated immunity. Can lead to scarring. some will have oral lesions as well. Pruritic purple papules
question
How do you treat Lichen sclerosus?
answer
high-potency topical steroids (clobetasol) daily for 4 weeks then qod then twice weekly
question
How do you treat lichen planus?
answer
high-potency topical steroids. Must monitor for SCC
question
What other vulvar disease should you be aware of?
answer
Paget's - rare (adenocarcinoma) but if see it also think breast or colorectal
question
What medication is most commonly associated with sexual dysfunction
answer
SSRI
question
What medication is useful with hypoactive sexual desire disorder?
answer
transdermal testosterone short term (< 6 months)
question
UTI in non-pregnant females
answer
Bactrim DS bid x 3 days Cipro 250 bid x 3 days Marobid bid x 7 days
question
Natural HRT
answer
plants do not make Estrogen. they make sterols which have an estrogen-like effect →phytoestrogens soy and isoflavines → vasomotor for 2 yrs st. johns' wart→depression for 2 yrs black cohash→vasomotor for 6 months
question
HRT and Breast cancer
answer
EPT → small ↑ risk (RR1.24) most studies do not show ↑ risk with E use alone + fan history is NOT contraindication for HRT
question
HRT and heart disease
answer
should not use HRT for CHD prevention
question
HRT and VTE
answer
if have h/o vet, stroke, tia or immobilized then should discontinue HRT
question
Autonomy
answer
right of patient to make own choice
question
beneficence
answer
the welfare of the patient
question
justice
answer
avoid discrimination (race, religion)
question
veracity
answer
deal honestly with patients and colleagues
question
routine lab screenings for gyn patients
answer
glc/fbs →q 3 years at age 65 lipid→q 5 years at age 45 TSH →q 5 years at age 50 dexa→q 2 years at age 65 Ua→q year at 65
question
T score
answer
std deviation from mean bone density of a normal young adult population a decrease of 1 sd will double risk of fracture
question
Z score
answer
std deviation from mean bond density of a reference population of same age, sex and race
question
screening for osteoporosis
answer
every 5 years from age 65 on OR every 2 years if on treatment Treat if T is -2 without risk factors or if -1.5 with risk factors
question
Osteopenia
answer
T score -1 to -2.5 SD (50%)
question
Osteoporosis
answer
T score < -2.5 SD (15%) Dexa (hip and spine are best) peak age of bone is 30 coritcal is 75% and trabecular is 25% (more surface area though)
question
osteoporosis treatment
answer
bisphosphonates →inhibits osteoclasts and ↑ bone density 50%. take on empty stomach and stay upright SERM (reloxifene)→Pro estrogen effect on bone and anti estrogen effect on endometrium and breast
question
Lipid profiles
answer
Tc <200 Tg 60 LDL <130 (<100 if high rush, <70 if very high risk) check after 9-12° fast
question
When should bone mineral density testing start?
answer
age 65 young if + risk factors re-screen every 2 years
question
How much calcium should you take daily?
answer
1,000mg daily 1,500 mg daily if > 65
question
What causes SUI?
answer
impairment of the pubourethral ligaments.
question
How do you treat BV?
answer
Flagyl 500 mg bid x 7 days OR clindamycin 300 mg bid x 7 days
question
What do you use for failed yeast infections?
answer
boric acid 600 mg capsules daily for 14 days
question
What is a positive test for BV?
answer
Need 3 out of 4 1. gray discharge 2. pH > 4.5 3. + amine test 4. > 20% epithelial clue being clue cells
question
How do you treat Trichomoniasis?
answer
Flagyl 500 mg bid x 7 days
question
HRT risks
answer
Increased risk of clot 34 vs 16 per 10,000 woman-years, Increased risk of breast cancer 38 vs 30 per 10,000 women years decreased hip fracture 10 vs 16 per 10,000
question
What thickness of endometrium excludes endometrial cancer?
answer
less than or equal to 4 mm - does not require EMB
question
How do you assess PMD
answer
either with EMB or U/S do not need both
question
When does fecundity decline?
answer
age 32 more rapidly at age 37
question
when should you start screening for colorectal cancer?
answer
age 50 and every 10 years
question
What SERM can treat osteoporosis?
answer
raloxifene - prevent and treat decrease bone tissue resorption by osteoclasts and therefore inhibit bone loss
question
What thrombotic effects are associated with SERMs?
answer
raloxifene and tamoxifen are associated with increased risk. RR 3.1
question
What breast candidates are appropriate for SERMs?
answer
Should be at high risk of developing breast cancer (ductal ca in situ, lobular ca in situ, ductal hyperplasia with atypia, strong family history)



