Foundations Chapter 42 Fluid, Electrolyte & Acid-Base Balance – Flashcards
Unlock all answers in this set
Unlock answersquestion
The primary health care provider orders the nurse to infuse 500 mL normal saline over 4 hours to a patient with a blood pressure of 100/70 mm Hg. What is the flow rate of infusion? Record your answer in mL per hour. _________ mL/hr
answer
125 A patient with a blood pressure of 100/70 mm Hg is hypotensive. Normal saline solution is used to maintain the patient's sodium level. The formula used to calculate the flow rate is the total infusion volume (mL) divided by the hours of infusion. Therefore, 500 mL of normal saline is divided by 4 hours to calculate the infusion rate, which is 125 mL per hour.
question
A patient who is undergoing intravenous therapy develops redness, inflammation, and swelling at the catheter site. After further assessment, the nurse finds purulent drainage from the injection site. Which nursing interventions are useful in this situation? Select all that apply. 1 Elevating the extremity 2 Cleaning the skin with alcohol 3 Raising the head of the patient's bed 4 Applying a pressure dressing over the site 5 Inserting a new intravenous line in another extremity
answer
2, 5 Redness, inflammation, swelling at the catheter site coupled with purulent indicate an infection. Cleaning the patient's skin with alcohol helps to maintain asepsis. Inserting a new intravenous line in the other extremity helps to reduce the chance of infection. Elevating the patient's extremity helps to reduce infiltration and extravasation. Raising the head of the patient's bed helps to control extracellular volume excess. The application of a pressure dressing over the injection site helps to reduce bleeding.
question
A primary health care provider orders 2 L of intravenous fluid over 6 hours using gravity-flow tubing and a macrodrip with a drop factor of 10 for a patient who has been vomiting. Calculate the minute flow rate of the infusion in gtt/minute and record your answer as a whole number. _________ gtt/min
answer
56 The minute flow rate is calculated as (mL/hour)(drop factor/60 min) = gtt/min. The flow rate of the intravenous fluid is 2L or 2000 mL for 6 hours, and the drop factor is 10. Therefore, the minute flow rate is: (2000/6)(10/60) = 55.56. This number rounds up to 56 gtt/min.
question
Which electrolyte controls the function of neuromuscular junctions? 1 Calcium 2 Potassium 3 Phosphate 4 Magnesium
answer
4 Magnesium controls the function of neuromuscular junctions and is a cofactor for many enzymes. Calcium influences the excitability of nerve and muscle cells. Potassium maintains normal muscle function by stabilizing the resting membrane potential of skeletal, smooth, and cardiac muscles. Phosphate facilitates the production of adenosine triphosphate.
question
Which body fluid is considered an intravascular fluid? 1 Synovial fluid 2 Plasma of the blood 3 Fluid outside the cells 4 Fluid outside the blood vessel
answer
2 Blood plasma is considered an intravascular fluid. Synovial fluid is considered a transcellular fluid. Extracellular fluid is located outside the cells. Interstitial fluid is located outside the blood vessels.
question
The skin of a patient taking intravenous fluids appears blanched, cool to the touch, and edematous. Upon touch, the patient reports pain. Which complication does this represent? 1 Phlebitis 2 Extravasation 3 Local infection 4 Circulatory overload
answer
2 Extravasation and infiltration are manifested by painful and blanched skin that is cool to the touch and edematous. Phlebitis is manifested by redness, tenderness, pain, and warmth along the course of the vein starting at the access site. Redness, heat, and swelling indicate a local infection at the catheter entry site. Circulatory overload is manifested by crackles in the dependent parts of the lungs, shortness of breath, and dependent edema.
question
Which ion is an example of an anion? 1 Sodium 2 Calcium 3 Chloride 4 Potassium
answer
3 Positively charged ions are called cations. Negatively charged ions are called anions. A chloride (Cl-) ion is an anion. Sodium (Na+), calcium (Ca+), and potassium (K+) are cations.
question
The nurse is providing intravenous therapy to a 78-year-old patient. Which nursing action is appropriate in this condition? 1 Inserting the intravenous line on the back of the hand 2 Applying friction while cleaning the site 3 Placing the intravenous line in a superficial vein 4 Inserting the intravenous line at a 10 to 15 degree angle
answer
4 A 78-year-old patient may have a loss of supportive tissue and the veins appear to be superficial. Therefore, the nurse should lower the insertion angle for venipuncture to 10 to 15 degrees after penetrating the needle into the skin. Inserting the intravenous line into the back of the hand may compromise the patient's mobility and result in discomfort. Applying friction while cleaning the injection site may lead to shredding of the skin in older adults. Because older adults have less subcutaneous support tissue, the nurse should avoid placing lines in veins that are superficial.
question
Which ions are cations? Select all that apply. 1 Sodium 2 Calcium 3 Chloride 4 Potassium 5 Bicarbonate
answer
1, 2, 4 Positively charged ions are called cations. Negatively charged ions are called anions. Sodium (Na+), calcium (Ca+), and potassium (K+) are cations. Chloride (Cl-) and bicarbonate (HCO3-) ions are anions.
question
The primary health care provider ordered 2 L of saline over 10 hours to a patient with diarrhea. What should be the flow rate of infusion? Record your answer in mL/hour using a whole number. ____________mL/hour
answer
200 The flow rate is calculated by dividing the total infusion volume by the hours of administration. Therefore, 2 L or 2000 mL is divided by 10 hours to obtain the infusion flow rate: 2000/10 = 200 mL/hour.
question
A patient with a 3% sodium chloride intravenous line develops shortness of breath and edema in the extremities. Upon auscultation, the nurse hears crackling sounds in the dependent parts of the lungs. Which nursing interventions are beneficial in this condition? Select all that apply. 1 Discontinuing the infusion 2 Elevating the head of the bed 3 Notifying the health care provider 4 Starting a new line in another extremity 5 Removing the line and applying sterile dressing
answer
1, 2, 3 Extracellular volume (ECV) excess occurs in a patient with sodium (Na+)-containing isotonic fluid. The assessment finding of circulatory overload of intravenous fluids is ECV excess. A patient with ECV excess is likely to develop crackles in the dependent parts of the lungs, shortness of breath, and edema in the extremities. Appropriate interventions include discontinuing the intravenous infusion and notifying the health care provider. The nurse should also elevate the head of the patient's bed and administer oxygen and diuretics if ordered. Starting a new intravenous line in another extremity may aggravate the patient's condition. The removal of the catheter and application of a sterile dressing is done in the case of local infection
question
A nurse teaches a patient with dehydration about maintaining safe intravenous therapy at home. Which statement made by the patient indicates a need for further learning? 1 "I should perform isometric exercises daily for 30 minutes." 2 "I should cover the injection site with plastic to prevent the site from getting wet during a shower." 3 "I should apply pressure to the injection site with sterile gauze if the catheter falls out." 4 "I should immediately report inflammation and itching at the injection site."
answer
1 A patient who is undergoing intravenous therapy should not perform isometric exercises because it may lead to bleeding and injury at the injection site. During a shower, the patient should protect the injection site and dressing from getting wet by covering it with plastic. Applying pressure with sterile gauze at the injection site if the catheter falls out helps to reduce bleeding. Inflammation and itching at the injection site may be an indication of infection and phlebitis; the patient should report these manifestations immediately.
question
The primary health care provider ordered 6 L of 0.9% sodium chloride over 24 hours to a patient with diarrhea. What should be the flow rate of infusion? Record your answer in mL/hour as a whole number.____________ mL/hour
answer
250 A patient with diarrhea requires 0.9% sodium chloride isotonic solution or normal saline solution. The flow rate is calculated by dividing the total infusion volume by the number of hours of administration. Therefore, 6 L or 6000 mL of normal saline solution is divided by 24 hours to obtain the infusion flow rate. The flow rate of the infusion is 6000/24 = 250 mL/hour.
question
A patient with vomiting and diarrhea reports lightheadedness while standing from a sitting position. The patient's blood pressure is 90/58 mm Hg. Which intervention would best treat this patient? 1 Administering diuretics 2 Monitoring the patient's 24-hour fluid intake and urine output 3 Limiting the patient's intake of fluids and foods rich in sodium 4 Administering 1000 mL of 0.9% normal saline solution with 10 mEq of potassium chloride
answer
4 A patient with vomiting and diarrhea may experience lightheadedness due to fluid and electrolyte imbalance. The blood pressure may also be altered to 90/58 mm Hg while changing positions, resulting in postural hypotension. Administering 1000 mL of 0.9% normal saline solution with 10 mEq of potassium chloride may accelerate the improvement of the patient's condition. Diuretics such as furosemide and thiazide may lead to hyponatremia and hypokalemia, which may aggravate the patient's condition. Monitoring the patient's 24-hour fluid intake and urine output is important, but it may not directly comfort the patient. Limiting the patient's intake of fluids and foods rich in sodium may worsen the condition.
question
A patient with chronic diarrhea shows Chvostek's sign. What might be the reason behind the patient's condition? Select all that apply. 1 Hypokalemia 2 Hypocalcemia 3 Hyponatremia 4 Hypomagnesemia 5 Hypophosphatemia
answer
2, 4 A patient with chronic diarrhea who has hypocalcemia and hypomagnesemia may show Chvostek's sign which is contraction of facial muscles when the facial nerve is tapped. Hypokalemia, hyponatremia, and hypophosphatemia manifest in other signs and symptoms.
question
A patient with a head injury is admitted to the emergency unit. The laboratory test reports reveal the patient's sodium level as 90 mEq/L. Which condition does the patient have? 1 Diabetes insipidus 2 Fatal cardiac dysrhythmias 3 Type B chronic obstructive pulmonary disease 4 Syndrome of inappropriate antidiuretic hormone
answer
4 The normal range for the sodium level is from 136 to 145 mEq/L. A patient with a head injury may have syndrome of inappropriate antidiuretic hormone, which may result in excessive secretion of antidiuretic hormone, which causes hyponatremia by causing water retention. A head injury may also cause diabetes insipidus, which leads to hypernatremia due to dilution of the urine. Fatal cardiac dysrhythmias occur due to hyperkalemia. Type B chronic obstructive pulmonary disease leads to fluid, electrolyte, and acid-base imbalances.
question
What are examples of transcellular fluids? Select all that apply. 1 Synovial fluid 2 Peritoneal fluid 3 Cerebrospinal fluid 4 Fluid outside the cells 5 Fluid outside the blood vessels
answer
1, 2, 3
question
The primary health care provider orders the nurse to infuse 1,000 mL of intravenous fluid to a patient with diarrhea over 4 hours using gravity-flow tubing with a drop factor of 9. Calculate the minute flow rate in drops/minute. Record your answer to one decimal place. ____________ drops/minute
answer
37.5 The flow rate of the intravenous fluid is 1,000 mL over 4 hours, or 250 mL per hour. Then, 250 mL/hr divided by 60 min/hr to get 4.167 mL/minute. Therefore, the minute flow rate is 4.167 mL/min × 9 = 37.503 drops/min, which rounds to 37.5 drops/min.
question
What condition may be suspected in a patient with end-stage renal disease? 1 Hypokalemia 2 Hypercalcemia 3 Hypocalcemia 4 Hypermagnesemia
answer
4 Hypermagnesemia is an abnormally high magnesium concentration in the blood; this can be caused by end-stage renal disease. Excessive fluid loss can cause hypokalemia. Malignant neoplasms or increased levels of parathyroid hormone can cause hypercalcemia. Hypoparathyroidism can cause hypocalcemia.
question
Which conditions are common in a patient with chronic diarrhea? Select all that apply. 1 Hyperkalemia 2 Hypocalcemia 3 Hypernatremia 4 Hypomagnesemia 5 Hyperphosphatemia
answer
2, 3, 4 Chronic diarrhea may lead to hypernatremia and result in clinical dehydration. It also leads to hypocalcemia and hypomagnesemia because diarrhea decreases electrolyte absorption. Hypokalemia occurs due to an increase in fluid output, not hyperkalemia. Hyperphosphatemia is uncommon during chronic diarrhea.
question
The primary health care provider orders the nurse to administer potassium chloride to a patient with 10 episodes of vomiting in two days. Which complication does the nurse anticipate from the potassium chloride? 1 Cancer 2 Seizures 3 Respiratory acidosis 4 Cardiac dysrhythmia
answer
4 Potassium chloride is an intravenous solution that should be carefully administered to a patient with severe emesis because hyperkalemia may cause fatal cardiac dysrhythmias. Patients with cancer often develop hypocalcemia. Hyponatremia or hypernatremia may cause confusion and seizures. An increased partial pressure of carbon dioxide leads to respiratory acidosis.
question
A patient on intravenous fluids develops shortness of breath and edema of the extremities. Upon auscultation, the nurse hears crackles in the dependent parts of the lungs. Which nursing intervention is beneficial in this condition? 1 Reducing the flow rate 2 Starting a new line in another extremity 3 Applying a warm and moist compress at the site 4 Removing the catheter and applying sterile dressing
answer
1 A patient with a circulatory overload of intravenous fluids may develop crackles in the dependent parts of the lungs, shortness of breath, and edema of the extremities. Therefore, the nurse should reduce the intravenous flow rate and notify the health care provider. Starting a new line in another extremity may aggravate the patient's condition. The nurse should apply a warm and moist compress when the patient experiences phlebitis. Removal of the catheter and the application of a sterile dressing is suggested in the case of local infection.
question
While receiving a blood transfusion, a patient develops chills, tachycardia, and flushing. What is the nurse's priority action? 1 Notify a health care provider. 2 Insert an indwelling catheter. 3 Alert the blood bank. 4 Stop the transfusion.
answer
4 Development of chills, tachycardia, and flushing during a blood transfusion indicate an acute hemolytic reaction. The nurse should stop the transfusion immediately so no more of the incompatible blood reaches the patient.
question
The nurse understands that various mechanisms in the body help move fluid from one compartment to another. Which transport mechanism is governed by oncotic and hydrostatic pressures? 1 Osmosis 2 Diffusion 3 Filtration 4 Active transport
answer
3 A filtration process determines fluid movement in and out of capillaries and is governed by hydrostatic and oncotic pressure within the vascular and interstitial space. Osmosis is the movement of water molecules across semipermeable membranes. Diffusion is the passive movement of electrolytes down the concentration gradient. Active transport refers to the transportation of electrolytes against the concentration gradient via adenosine triphosphate (ATP).
question
A patient with cardiac failure is found to have excess extracellular fluid of normal tonicity. Which life-threatening complication is this patient most likely to suffer? 1 Coma 2 Seizures 3 Pulmonary edema 4 Hypovolemic shock
answer
3 The most likely life-threatening complication that can occur in a patient who has excess extracellular fluid of normal tonicity is pulmonary edema. The excess fluids may filter out of the pulmonary blood vessels and pool in the pulmonary tissue, causing pulmonary edema. Coma and seizures are likely complications of hypernatremia and hyponatremia. Hypovolemic shock is seen in conditions associated with extracellular fluid depletion.
question
Which condition may lead to an extracellular fluid volume deficit? Select all that apply. 1 Burns 2 Cirrhosis 3 Heart failure 4 Hemorrhage 5 Adrenal insufficiency
answer
1, 4, 5 An extracellular fluid volume (ECV) deficit occurs when there is insufficient isotonic fluid in the extracellular compartment. Burns, hemorrhage, and adrenal insufficiency will lead to an ECV deficit. Cirrhosis and heart failure will lead to an ECV excess.
question
How might sepsis manifest? 1 Cough 2 Crackles 3 Dyspnea 4 Circulatory shock
answer
4 Circulatory shock is a manifestation of sepsis. Cough, crackles, and dyspnea are manifestations of circulatory overload.
question
Which defining characteristics are consistent with fluid volume deficit? 1 A weight loss of 1 lb (0.5 kg) in 1 week, pale yellow urine 2 Engorged neck veins when upright, bradycardia 3 Dry mucous membranes, thready pulse, tachycardia 4 Bounding radial pulse, flat neck veins when supine
answer
3 A deficit of fluid volume includes a deficit of extracellular fluid volume (ECF), hypernatremia, and clinical dehydration. ECF deficit is characterized by dry mucous membranes, thready pulse, and tachycardia, among other indicators. Weight loss of 1 lb (0.5 kg) in 1 week could indicate fat loss instead of fluid loss. ECF deficit causes dark yellow urine rather than pale yellow urine, which is normal.
question
Which electrolyte abnormality is least likely to be caused by the use of laxatives? 1 Hyponatremia 2 Hypokalemia 3 Hypocalcemia 4 Hypomagnesemia
answer
1 Hyponatremia can be caused by the use of antidepressants. Hypokalemia, hypocalcemia, and hypomagnesemia can be caused by the use of laxatives. Therefore, in the patients with these conditions laxatives are contraindicated.
question
Which can cause an excess of extracellular fluid volume? 1 Vomiting 2 Diarrhea 3 Hemorrhage 4 Chronic heart failure
answer
4 Chronic heart failure results in an excess of extracellular fluid volume, because there is a decrease in urine output due to elevated aldosterone. Vomiting and diarrhea cause a loss of fluids and electrolytes, which results in extracellular volume deficit. Hemorrhage also decreases the extracellular volume due to loss of fluids.
question
Which electrolyte influences excitability of nerve and muscle cells and is necessary for muscle contraction? 1 Calcium (Ca2+) 2 Potassium (K+) 3 Phosphate (PO4) 4 Magnesium (Mg2+
answer
1 Calcium influences the excitability of nerve and muscle cells and is necessary for muscle contraction. Potassium maintains the resting membrane potential of skeletal, smooth, and cardiac muscle, allowing for normal muscle function. Electrolyte phosphate is necessary for the production of adenosine triphosphate (ATP), the energy source for cellular metabolism. Electrolyte magnesium influences the function of neuromuscular junctions and is a cofactor for numerous enzymes.
question
A patient with a cardiac history is taking the diuretic furosemide and is seen in the emergency department for muscle weakness. Which laboratory value should the nurse assess first? 1 Serum albumin 2 Serum sodium 3 Hematocrit 4 Serum potassium
answer
4 Potassium-wasting diuretics such as furosemide increase potassium urinary output and can cause hypokalemia unless potassium intake also increases. Hypokalemia causes muscle weakness.
question
Which fluid electrolyte imbalance may develop in a patient who consumes spironolactone? 1 Hypokalemia 2 Hyperkalemia 3 Hyponatremia 4 Hypomagnesemia
answer
2 Spironolactone is a potassium-sparing diuretic that may cause hyperkalemia. Hypokalemia and hypomagnesemia may be caused by potassium-wasting diuretics such as furosemide. Hyponatremia is caused by antidepressants such as fluoxetine.
question
A patient has extracellular volume deficit due to diarrhea. How should the nurse correct the volume deficit in the patient? 1 Provide caffeinated fluids. 2 Provide low-sodium fluids. 3 Provide fluids that contain lactose. 4 Provide fluids that contain sodium.
answer
4 The nurse should use fluids such as an electrolyte replacement, which contains sodium to correct extracellular volume deficit. The sodium in the fluids helps to prevent fluid loss through retention. Caffeinated fluids, low-sodium fluids, and fluids containing lactose are not ideal to correct the extracellular volume deficit of diarrhea. These fluids tend to promote fluid loss and cause dehydration.
question
Which physical findings can be seen in a patient with extracellular fluid volume (ECV) deficit? Select all that apply. 1 Edema 2 Thready pulse 3 Crackles in lungs 4 Postural hypotension 5 Dry mucous membranes
answer
1, 4, 5 A thready pulse, postural hypotension, and dry mucous membranes are the physical findings of an extracellular fluid volume deficit. Edema in dependent areas and crackles in the lungs are the physical findings of extracellular fluid volume excess.
question
A patient with blood type A is in need of packed red cells on an emergency basis, but none of the donors of this type are available. How can the nurse provide better health care to the patient? 1 Arrange to provide red blood cells of group O. 2 Arrange to provide red cells of group AB. 3 Arrange for an autologous blood transfusion. 4 Wait until the donor of blood type A becomes available.
answer
1
question
As the nurse is assessing the caseload of patients for the day, which patient would the nurse expect to be at the highest risk of developing dehydration? 1 A 78-year-old patient with dementia 2 A 47-year-old patient with hyperthyroidism 3 A 53-year-old patient with pulmonary embolism 4 A 32-year-old patient with a respiratory infection
answer
1 Older patients may become dehydrated because of altered responses to illness related to age. In addition, persons with dementia might not recognize the urge to drink. Patients who are in their 30s, 40s, or 50s with hyperthyroidism, pulmonary embolism, and respiratory infection are not at great risk for dehydration.
question
Which food item should the nurse include in the diet plan of a patient with magnesium deficiency? 1 Milk 2 Broccoli 3 Brazil nuts 4 Dark-green leafy vegetables
answer
4 Dark-green leafy vegetables are rich in magnesium. Milk is rich in phosphate and calcium, not magnesium. Broccoli is rich in calcium, not magnesium. Brazil nuts are rich in potassium, not magnesium.
question
Which patient is most at risk of developing hypokalemia? 1 Patient with cancer 2 Patient with oliguria 3 Patient with diarrhea 4 Patient with acute pancreatitis
answer
3 A patient with diarrhea loses fluids and potassium, which can lead to hypokalemia. A patient with cancer develops hypercalcemia because some cancer cells secrete chemicals into the blood that are related to the parathyroid hormone. Oliguria causes decreased potassium output resulting in hyperkalemia. A patient with acute pancreatitis develops hypocalcemia because calcium binds with the undigested fat in the feces and is excreted.
question
Which factor can be a risk for causing extracellular volume deficit (ECV)? 1 Hemorrhage 2 Sodium-rich diet 3 Intravenous therapy 4 Oliguric renal disease
answer
1 There are many risk factors for fluid, electrolyte, and acid-base imbalances. Hemorrhage causes a deficit in the ECV. A sodium-rich diet is an environmental factor that causes ECV excess. Intravenous therapy and oliguric renal disease also cause ECV excess.
question
After reviewing a patient's laboratory reports, the nurse instructs him or her to consume dairy products. Which electrolytic imbalance may have prompted this instruction? 1 Hypokalemia 2 Hyperkalemia 3 Hypocalcemia 4 Hypercalcemia
answer
3 Hypocalcemia is characterized by decreased calcium levels. Dairy products such as milk are rich sources of calcium; therefore, the nurse instructs the patient to consume dairy products. The nurse should instruct a patient with hypokalemia to consume a potassium-rich diet. The nurse would recommend a potassium-free diet to a patient with hyperkalemia. The consumption of dairy products can further increase the risk of hypercalcemia.
question
Which patient being cared for by the nurse is at the highest risk of developing respiratory acidosis? 1 A patient with hypokalemia 2 A patient with pulmonary fibrosis 3 A patient with salicylate overdose 4 A patient with chronic obstructive pulmonary disease (COPD)
answer
4 Chronic respiratory acidosis is most commonly caused by chronic obstructive pulmonary disease (COPD). Hypokalemia, pulmonary fibrosis, and salicylate overdose do not predispose a patient to respiratory acidosis. Hypokalemia can lead to cardiac dysrhythmias. Pulmonary fibrosis can result in respiratory arrest, and salicylate overdose results in central nervous system changes.
question
How much fluid is lost daily through feces in a healthy adult? Record your answer using a whole number. __________ mL
answer
100 The gastrointestinal system plays a major role in fluid and electrolyte balance in the body. Approximately 3 to 6 L of fluid enters the gastrointestinal system and is absorbed back into the body. Approximately 100 mL of fluid is excreted through feces daily.
question
The health care provider's order is 1000 mL 0.9% NaCl with 20 mEq K+ intravenously over 8 hours. Which assessment finding should cause the nurse to clarify the order with the health care provider before hanging this fluid? 1 Flat neck veins 2 Tachycardia 3 Hypotension 4 Oliguria
answer
4 Administration of KCl (increased K+ intake) to a person who has oliguria (decreased K+ output) can cause hyperkalemia.
question
While performing a general examination of a patient, the nurse finds that the patient has tetany and is positive for Chvostek's sign and Trousseau's sign. Which electrolyte disturbance is responsible for this clinical presentation? 1 Hypokalemia 2 Hyponatremia 3 Hypocalcemia 4 Hypermagnesemia
answer
3 Positive Chvostek's sign, Trousseau's sign, and presence of tetany indicate hypocalcemia. Low levels of calcium may affect the excitability of the nerve and muscle cells, causing cramps and abnormal muscle movements. Hypokalemia presents with muscular weakness and cardiac rhythm disturbances. Hyponatremia usually presents with nausea, vomiting, confusion, and seizures. Hypermagnesemia is an abnormally high magnesium concentration in the blood. Chvostek's sign and Trousseau's sign are associated with hypomagnesemia.
question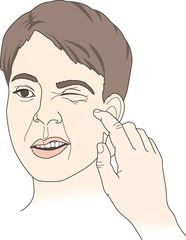
Clinical sign of existing nerve hyperexcitability or tetany seen in hypocalcemia. Refers to an abnormal reaction to the stimulation of the facial nerve. Low levels of calcium may affect the excitability of the nerve and muscle cells, causing cramps and abnormal muscle movements
answer
Positive Chvostek's Sign
question
Sign of latent tetany observed in patients with low calcium. Low levels of calcium may affect the excitability of the nerve and muscle cells, causing cramps and abnormal muscle movements.

answer
Trousseau Sign
question
The nurse finds redness, heat, and swelling at the catheter-skin entry point and purulent drainage in a patient on intravenous infusion. Which complication does the nurse suspect? 1 Phlebitis 2 Bleeding 3 Extravasation 4 Local infection
answer
4 A local infection is characterized by redness, heat, and swelling at the catheter-skin entry point, and possible purulent drainage. Fresh blood evident at the venipuncture site and sometimes pooling under the extremity are the assessment findings of bleeding at the venipuncture site. The assessment findings of phlebitis are redness, tenderness, pain, and warmth along the course of the vein. Edematous, blanched skin that is cool to the touch indicates extravasation.
question
What conditions place a patient at a higher risk for hypomagnesemia? Select all that apply. 1 Polyuria 2 Bone tumors 3 Steatorrhea 4 Chronic alcoholism 5 Hyperparathyroidism
answer
3, 4 Steatorrhea and chronic alcoholism place a patient at higher risk for hypomagnesemia. Polyuria may lead to hypokalemia. Bone tumors and hyperparathyroidism are associated with hypercalcemia.
question
Which symptom can be seen in a patient with phlebitis? 1 Blanched skin 2 Edematous skin 3 Purulent drainage 4 Redness of the skin
answer
4 Inflammation of the inner layer of a vein is known as phlebitis. In this condition, the patient will have redness of the skin. Blanched skin and edematous skin are associated with extravasation. Purulent drainage is a sign of a local infection.
question
Which laboratory finding is consistent with a diagnosis of milk-alkali syndrome? 1 Calcium level of 7 mg/dL 2 Calcium level of 15 mg/dL 3 Magnesium level of 1 mEq/dL 4 Magnesium level of 3 mEq/dL
answer
2 Milk-alkali syndrome is a condition where increased intake and absorption of calcium occurs in the body. The normal serum calcium level ranges from 8.4 to 10.5 mg/dL. A calcium level greater than 10.2 mg/dL indicates hypercalcemia. Therefore, a calcium level of 15 mg/dL would be found in a patient with milk-alkali syndrome. A calcium level of 7 mg/dL indicates hypocalcemia. Abnormal magnesium levels are not associated with milk-alkali syndrome.
question
Which activities can the nurse delegate to nursing assistive personnel (NAP)? Select all that apply. 1 Measuring oral intake and urine output 2 Preparing intravenous (IV) tubing for routine change 3 Reporting an IV container that is low in fluid 4 Changing an IV fluid container 5 Reporting an electronic infusion device alarm
answer
1, 3, 5 The nurse is able to delegate measuring oral intake and urine output, reporting an IV container that is low in fluid, and reporting an electronic infusion device alarm.The registered nurse cannot delegate working with intravenous (IV) tubing or changing an IV infusion to nursing assistive personnel (NAP).
question
Which drugs can cause hypokalemia? Select all that apply. 1 Captopril 2 Fluoxetine 3 Prednisone 4 Furosemide 5 Spironolactone
answer
3, 4 Furosemide and prednisone will cause hypokalemia. Captopril and spironolactone may cause hyperkalemia. Fluoxetine may cause hyponatremia.
question
What is the normal range of values of phosphate in human blood? 1 1.5 to 2.5 mEq/L 2 2.7 to 4.5 mg/dL 3 3.5 to 5.0 mEq/L 4 4.5 to 5.3 mg/dL
answer
2 The normal range of values of phosphate in human blood is 2.7 to 4.5 mg/dL. The normal value of potassium is 3.5 to 5.0 mEq/L, the normal value of ionized calcium is 4.5 to 5.3 mg/dL, and the normal value of magnesium is 1.5 to 2.5 mEq/L.
question
Which clinical criteria of phlebitis should receive a grade of 3? 1 Formation of streak 2 Pain at access site with only erythema 3 Palpable venous cord greater than 2.54 cm 4 Erythema at access site with or without pain
answer
1 According to the phlebitis scale, the nurse would give a grade of 3 if there is any streak formation or a palpable venous cord. The nurse would give a grade of 2 if there is only erythema. The nurse would grade give a grade of 4 if there is a palpable venous cord greater than 2.54 cm. Erythema at the access site with or without pain is grade 1.
question
The nurse is checking the order of intravenous flow rate. The total volume is 0.5 L per 4 hours. What is the hourly flow rate? Record your answer using a whole number._______ mL/h
answer
125 If the hourly rate is not provided in the order, the nurse must calculate it by dividing volume by hours. 0.5 L, or 500 mL, divided by 4 is 125 mL/h.
question
The nurse is assessing the clinical criteria for the infiltration scale. What would the grade be if there is 10.8 cm of edema in the infiltration? 1. 1 2. 2 3. 3 4. 4
answer
2 According to the infiltration scale, edema that is 2.54 to 15.2 cm is grade 2. Edema less than 2.54 cm, about an inch, is grade 1. Edema greater than 15.2 cm, or 6 inches, in any direction with mild to moderate pain is grade 3. Edema greater than 15.2 cm with moderate to severe pain is grade 4.
question
A nurse is assessing the clinical markers of vascular volume. Which patient may require intravenous (IV) therapy due to extracellular fluid volume deficit? 1 A patient with a full pulse rate 2 A patient with dark yellow urine 3 A patient with increased blood pressure 4 A patient with crackles in the lobe of the lung
answer
2 A dark yellow color indicates concentrated urine that may be caused by a decrease in the extracellular fluid volume; therefore, this patient may require IV therapy. An increase in the pulse rate indicates excess fluid volume. The blood pressure increases with excess extracellular fluid volume. Crackles indicate excess fluid volume.
question
Which grade on the phlebitis scale is given to a patient with pain at the infusion site and erythema? 1 Grade 1 2 Grade 2 3 Grade 3 4 Grade 4
answer
2 The clinical criteria for grade 2 on the phlebitis scale are pain and erythema at the infusion site. The clinical criterion for grade 1 is erythema at the infusion site. The clinical criteria for grade 3 are pain at the site, erythema, and streak formation or a palpable venous cord. The clinical criteria for grade 4 are pain at the site with erythema and streak formation along with purulent discharge.
question
Which immediate intervention would be beneficial in a patient who developed redness and pain at the infusion site? 1 Stopping the infusion 2 Elevating the extremity 3 Applying warmth to the site 4 Notifying the health care provider
answer
1 Redness and pain at an infusion site indicate phlebitis; therefore, the nurse should stop the infusion or start a new line if these symptoms occur in the patient. The extremities are elevated if symptoms of infiltration occur. Applying warmth to the site is an intervention for infiltration. The health care provider can be notified, but the immediate action is to stop the infusion.
question
Which action can be performed to prevent the risk of dislodging the catheter during intravenous (IV) therapy? 1 Inserting a volume-control device into the IV container 2 Curling the loop of short or long IV tubing alongside the arm 3 Instructing the patient to avoid raising the arm with the catheter 4 Attaching the distal end of the IV tubing to a needleless connector
answer
2 The nurse should curl the loop of the short or long IV tubing alongside the arm to prevent the risk of dislodging the catheter during IV therapy. Inserting a volume-control device into the IV container maintains a slow rate of infusion. Avoiding raising the arm may prevent the risk of discontinuity in the flow rate. Attaching the distal end of the IV tubing initiates the flow of fluid through the IV catheter and prevents the device from clotting.
question
Which saline solution draws water from cells into the extracellular fluid (ECF) by osmosis? 1 5% sodium chloride 2 0.9% sodium chloride 3 0.45% sodium chloride 4 0.225% sodium chloride
answer
1 Saline solution is sodium chloride in water. Sodium chloride 5.0% draws water from the cells into the ECF by osmosis. Sodium chloride 0.9% expands the ECV and does not enter the cells. Sodium chloride 0.45% and 0.225% expand the ECV and rehydrate cells.
question
Which complication of intravenous (IV) therapy indicates the need for pressure at the site? 1 Bleeding 2 Phlebitis 3 Infection 4 Fluid overload
answer
1 Bleeding may be a complication of IV therapy; applying pressure at the site can reduce bleeding. Phlebitis may indicate that the infusion should be stopped. The primary health care provider should be notified if symptoms of infection occur. Reduction in the IV flow rate may reduce circulatory overload.
question
The health care provider's order is 1000 mL 0.9% NaCl IV over 6 hours. Which rate should the nurse program into the infusion pump? 1 125 mL/hr 2 167 mL/hr 3 200 mL/hr 4 1000 mL/hr
answer
2 1000 mL divided by 6 hours is 166.7 mL/hr, which rounds to 167 mL/hr (if the infusion pump accepts decimals, it should be programmed to 166.7 mL/hr).
question
Arrange in order the steps performed for the insertion of a vascular access device (VAD). 1. Cleanse site with chlorhexidine. 2. Stabilize vein below insertion site. 3. Look for blood return in flashback chamber. 4. Palpate vein for resilience. 5. Advance catheter into vein until hub is near insertion site. 6. Puncture vein with catheter at a 10- to 30-degree angle.
answer
4, 1, 2, 6, 3, 5 When inserting a VAD, the nurse must first palpate the vein for resilience and find a venipuncture site. The nurse must then cleanse the site with an antiseptic such as chlorhexidine, and stabilize the vein by placing a thumb over it and stretching the skin against the direction of insertion. The vein is then punctured with a catheter at a 10- to 30-degree angle. If there is no evidence of blood flow back into the chamber, the catheter is advanced into the vein until the hub is near the insertion site.
question
A patient reports swelling at the incision site during administration of intravenous fluids. What should be the immediate nursing intervention? 1 Remove the catheter 2 Apply a sterile dressing 3 Use a skin protectant to wipe the area 4 Apply tape or gauze around the arm
answer
1 Swelling at the incision site during administration of intravenous fluids is due to infiltration, so removal of the catheter is indicated. A sterile dressing can be applied after securing the catheter, but the nurse must immediately remove the catheter. The area can be wiped with a skin protectant after the catheter has been removed. Applying tape and gauze may cause compression of the veins.
question
The registered nurse is reinforcing to a nursing student the teachings regarding the maintenance of intravenous (IV) flow rate when a polyvinyl chloride container is used for infusion. Which statements by the nurse indicate effective understanding? Select all that apply. 1 "I will monitor the drip rate every 3 hours." 2 "I will mark the date and time on the container." 3 "I will insert the volume-control device spike to the IV container." 4 "I will observe the patient for signs of overhydration and dehydration." 5 "I will instruct the patient to avoid raising the arm with the IV line."
answer
3, 4, 5 To maintain IV flow rate when a polyvinyl chloride container is used for infusion, the volume-control device should be inserted into the spike to deliver small amounts of fluid and prevent bolus administration. To prevent complications, the nurse should observe the patient for any signs and symptoms of overhydration or dehydration. Raising the arm may alter the fluid rate, so the nurse should instruct the patient to avoid raising the arm with the catheter. The drip rate should be monitored every hour to ensure IV administration as prescribed. The date and time should not be marked on the label of the polyvinyl chloride container because the ink may enter the container.
question
The nurse curls a loop of intravenous tubing alongside the arm of a patient on intravenous (IV) therapy. Which outcome can be expected with this nursing action? 1 Altered flow rate 2 Reduced risk of infection 3 Reduced risk of dislodging 4 Increased access to the tubing junction
answer
3 The nurse curls a loop of the intravenous tubing alongside the arm to reduce the risk of dislodging the catheter during IV therapy. Manipulation of the catheter dressing can cause alteration in the flow rate. The nurse uses a gauze pad over the insertion site to reduce the risk of infection. Applying tape to the gauze pad of the insertion site facilitates access to the tubing junction.
question
What are the nursing considerations while administering intravenous (IV) therapy in an elderly patient? 1 The nurse should use a small-gauge catheter. 2 The nurse should secure the catheter with tape. 3 The nurse should use the back of the hand for the intravenous line. 4 The nurse should use an insertion angle of 45 degrees for vein puncture.
answer
1 The nurse should use a small-gauge catheter for IV therapy in an elderly patient because their veins are very fragile and the smallest gauge allows better blood flow. The nurse should use a surgical stretch mesh to secure the catheter; tape is not used for fragile skin. The back of the hand should not be used for intravenous administration because it may interfere with mobility. Older adults have a loss of supportive tissue, and the veins tend to lie superficially; therefore, the nurse should lower the insertion angle to 10 to 15 degrees for vein puncture.
question
The registered nurse is instructing a nursing student about the interventions that must be performed when there is any evidence of complication due to infusion therapy. Which instruction would the nurse follow for a patient with circulatory overload? 1 "Reduce the intravenous (IV) flow." 2 "Elevate the extremity." 3 "Disconnect the IV tubing." 4 "Discontinue the IV infusion."
answer
1 If the nurse suspects circulatory overload in a patient, the immediate nursing intervention is to reduce the IV flow rate and notify the health care provider. The nurse must elevate the extremity when there is any evidence of infiltration near the infusion site; this helps the infiltration to subside. The nurse must disconnect IV tubing and discontinue the IV infusion when there is evidence of infiltration.
question
Which condition can be observed in a patient for whom intravenous (IV) therapy was suggested for excessive thirst? 1 Hyperkalemia 2 Hypercalcemia 3 Hypernatremia 4 Hypermagnesemia
answer
3 Hypernatremia, also known as water deficit, is caused by body fluids becoming too concentrated and results in excessive thirst, known as clinical dehydration; therefore, this condition may be observed in a patient for whom IV therapy was suggested. Hyperkalemia is abnormally high potassium ion concentration in the blood and can cause muscle weakness. Hypercalcemia is abnormally high calcium concentration in the blood and can cause constipation and reduced tendon reflexes. Hypermagnesemia is abnormally high magnesium concentration in the blood and may decrease tendon reflexes.
question
The nurse is initiating intravenous therapy. Arrange the actions to be performed by the nurse in sequential order. 1. Applying the end cap after attaching the catheter hub 2. Injecting saline solution into the short extension tubing 3. Preparing short extension tubing with a needleless connecter 4. Removing the protective cap from the needleless connector and attaching a syringe
answer
3, 4, 2, 1 While initiating intravenous therapy, the nurse must prepare the short extension tubing with a needleless connecter and attach it to the vascular access device (VAD). The nurse must then remove the protective cap from the needleless connecter and attach it to the syringe. Next the nurse must inject the saline solution into the short extension tubing. After injecting the saline solution, the nurse must close the end cap after attaching the catheter hub to maintain sterility.
question
While receiving blood, a patient has a transfusion reaction. Which action if performed by the nurse indicates a need for further teaching? 1 Keeping the intravenous (IV) line open 2 Notifying the emergency response team 3 Stopping the blood and continuing saline solution 4 Monitoring signs and symptoms every 30 minutes
answer
3 Performing prompt interventions in a patient who has an unexpected reaction during a blood transfusion restores the patient's physiological stability. The nurse must not turn off the blood and simply turn on the 0.9% sodium chloride, because this would cause the blood remaining in the IV tubing to infuse into the patient. The nurse must keep the IV line open by replacing the IV tubing down to the catheter hub with new tubing, and running normal saline solution. The nurse must notify the health care provider or emergency response team for further guidance. The nurse must monitor the patient's signs and symptoms and vital signs every 5 minutes.
question
A primary health care provider suggested home intravenous (IV) therapy for a patient who is taking anticoagulants. Which nursing actions signify effective understanding regarding intravenous therapy? Select all that apply. 1 Having the patient refrain from performing activities of daily living 2 Instructing the patient to report symptoms of infection 3 Teaching the safe disposal of intravenous materials exposed to blood 4 Advising the patient to report if the intravenous tubing and dressing become soiled 5 Instructing the caregiver to apply pressure for 5 min when the access device is removed
answer
2, 3 The nurse should explain to a patient who is taking anticoagulants about IV therapy and the symptoms of infection or infiltration and instruct the patient to report such symptoms. The nurse should instruct the patient regarding the safe disposal of containers exposed to blood. The nurse should teach the patient how to ambulate and allow the patient to perform activities of daily living. The nurse should teach the patient and caregiver how to change the intravenous tubing when required. Because the patient is on anticoagulant therapy, when the access device is removed, the pressure should be applied for 20 minutes to reduce the risk of bleeding.
question
The nurse is assessing a peripheral vascular access device (VAD) site. Which patient requires monitoring of the site every 5 to 10 minutes? 1 A neonate patient 2 A patient who is critically ill 3 An oriented adult patient 4 A patient with infusion of vasoconstrictors
answer
4 The INS Standard of Practice provides guidelines for assessment of a peripheral VAD site to determine whether replacement is clinically indicated. During infusions of vesicants or vasoconstrictors, the nurse must monitor the patient every 5 to 10 minutes. The nurse must monitor neonates and children who are on infusion at least every hour. The nurse must assess critically ill patients who are on infusion therapy at least every 1 to 2 hours. The nurse must assess oriented adults who are able to report problems at the VAD site at least every 4 hours.
question
A patient on intravenous (IV) therapy reports mild pain and numbness at the puncture site. The nurse finds edema 16 cm in size. Which grade according to the infiltration scale is given to the patient? 1 Grade 1 2 Grade 2 3 Grade 3 4 Grade 4
answer
3 The clinical criteria for grade 3 are edema greater than 15.2 cm, mild to moderate pain, and numbness. The clinical criteria for grade 1 are edema less than 2.54 cm with or without pain. The clinical criteria for grade 2 are edema 2.54 to 15.2 cm with or without pain. The clinical criteria for grade 4 are a leaky, discolored, swollen appearance of the skin and edema greater than 15.2 cm. Circulatory impairment and pain can occur.
question
Which transfusion reaction may include clinical manifestations such as dyspnea? 1 Mild allergic reactions 2 Anaphylactic reactions 3 Febrile nonhemolytic reactions 4 Acute intravascular hemolytic reactions
answer
2 Anaphylactic reactions may occur due to adverse transfusion reactions, and their clinical manifestations include dyspnea. Mild allergic reactions caused by transfusions may manifest clinically as flushing, itching, and urticaria. Febrile nonhemolytic transfusion reactions manifest clinically as anxiety and muscle pain. Acute intravascular hemolytic transfusion reactions manifest clinically as hemoglobinuria, circulatory shock, cardiac arrest, and death.
question
A patient has acute intravascular hemolysis as an adverse effect of transfusion reaction. Which nursing intervention will be beneficial? 1 Administration of diuretics 2 Administration of antibiotics 3 Administration of antihistamines 4 Administration of glucocorticoids
answer
1 To maintain the urinary flow rate, the nurse must administer diuretics to a patient with acute intravascular hemolysis as an adverse effect of transfusion reaction. Antibiotics are required if the patient develops sepsis. Administration of antihistamines is beneficial if the patient has an allergic reaction. Administration of glucocorticoids would be beneficial if the patient has sepsis.
question
Before initiating intravenous (IV) therapy, for which clinical markers of interstitial volume would the nurse assess? 1 Skin turgor 2 Urine output 3 Capillary refill 4 Auscultation of lungs
answer
1 Clinical markers of interstitial volume include skin turgor. The nurse pinches the skin over the sternum or the inside of the forearm; failure of the skin to return to its normal position within 3 seconds indicates extracellular volume deficit. Urine output is a clinical marker of vascular volume; decreased and dark yellow urine indicates extracellular volume deficit. The capillary refill time and auscultation of lungs are clinical markers of vascular volume.
question
The nurse is reinforcing to a nursing student the teachings regarding the management of transfusion reactions. Which statements by the nurse indicate effective understanding regarding a febrile nonhemolytic reaction in a thrombocytopenic patient? Select all that apply. 1 "I will adjust the transfusion volume." 2 "I will administer aspirin." 3 "I will stop the transfusion." 4 "I will administer antipyretics." 5 "I will restart the transfusion after some time."
answer
3, 4 When there is a nonhemolytic reaction in a thrombocytopenic patient, the transfusion should be stopped immediately to prevent deterioration of that patient's condition. Antipyretics can be administered to reduce the patient's symptoms. Adjusting the transfusion volume may cause the patient's condition to deteriorate; therefore, the transfusion should be stopped immediately. Aspirin should be avoided in thrombocytopenic patients. Restarting the transfusion is not indicated because it may worsen the patient's condition.
question
What are the typical signs of phlebitis in a patient with an intravenous line? Select all that apply. 1 Heat 2 Swelling 3 Paleness 4 Erythema 5 Tenderness
answer
1, 4, 5 Phlebitis is inflammation of the veins; it can have chemical, mechanical, or bacterial causes. Risk factors for phlebitis are acidic or hypertonic intravenous solutions. The typical signs of phlebitis include heat, erythema, and tenderness. Swelling and paleness are evident when there is infiltration.
question
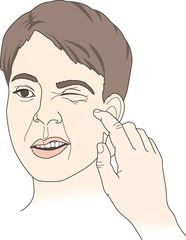
Which effect can be obtained by the action performed in the figure? 1 Provides a suction effect 2 Prevents touch contamination 3 Replaces air with normal saline solution 4 Allows accurate regulation of the flow rate
answer
3 The image indicates connecting the short extension tubing with a needleless connector to help prevent air from entering the patient's vein; normal saline solution replaces any air that is removed. Squeezing the drip chamber to fill it with fluid provides a suction effect. Maintaining the sterility of both ends of the tubing prevents contamination. Placing the roller clamp of the intravenous tubing below the drip chamber allows accurate regulation of the flow rate.
question
Which type of dextrose solution is considered isotonic? 1 Dextrose 5% in water 2 Dextrose 10% in water 3 Dextrose 5% in 0.9% sodium chloride 4 Dextrose 5% in 0.45% sodium chloride
answer
1 Dextrose 5% in water is an isotonic solution. Dextrose in 10% water is a hypertonic solution. Dextrose 5% in 0.9% sodium chloride and dextrose 5% in 0.45% sodium chloride are also hypertonic solutions.
question
After insertion of an intravenous catheter, the nurse places a gauze pad and secures the edges with tape. What is the rationale behind this nursing action? 1 To retain moisture in the skin 2 To prevent pressure on the skin 3 To reduce the entry of microorganisms 4 To prevent visualization of the insertion site
answer
3 The nurse secures the edges of the dressing with tape to prevent the entry of microorganisms into the insertion site. Wrapping the dressing materials around the arm causes the arm to compress the veins and prevent the visualization of the insertion site. The nurse secures the gauze pad with tape to help carry the moisture away from the skin to prevent contamination. Tape on the gauze elevates the hub and prevents pressure on the skin.
question
Which patient should be assessed for bleeding at the infusion site by pressing the site for 2 to 3 minutes after discontinuation of the infusion? 1 Normal patient 2 Patient taking heparin 3 Patient taking low-dose aspirin 4 Patient who has a low platelet count
answer
1 During an assessment of bleeding of a normal patient, pressure at the site of infusion should be applied for 2 to 3 minutes until hemostasis occurs. With patients who are on heparin or low-dose aspirin, or patients who have a low platelet count, this assessment time is prolonged to 5 to 10 minutes.
question
Which equipment is used to apply friction prior to inserting a vascular assistive device (VAD)? 1 Antiseptic swab 2 Sterile gauze pad 3 Adhesive remover 4 Skin protectant solution
answer
1 The nurse uses an antiseptic swab prior to inserting a vascular assistive device (VAD). The nurse should apply friction at the insertion site to penetrate the antiseptic into the layers of the skin. Skin protectant is applied over the area where the tape is applied or dressing is performed to maintain skin integrity. An adhesive remover is used to remove residue from the skin. A sterile gauze pad is placed on the intravenous site after the insertion of the catheter to secure the catheter hub.
question
A nurse performs intravenous tubing changes for four patients. Which patient is receiving a tubing change at the appropriate frequency? 1 Patient A 2 Patient B 3 Patient C 4 Patient D
answer
4 Due to the higher chances of bacterial growth in the tubing, the infusion of blood components requires more frequent changes of the tubing. Thus, a patient undergoing a blood components infusion is receiving the right frequency of tubing change (every 4 hours). Blood infusions tubing should be changed every 4 hours. Continuous infusions tubing should be changed every 96 hours. Intermittent infusion tubing should be changed every 24 hours.
question
The nurse is selecting venipuncture sites in four patients. Which of the following is a proper venipuncture site? 1 Foot vein of a child 2 Foot vein of an adult 3 Dominant hand vein of an ambulatory patient 4 Hand vein in the arm with a fistula of a dialysis patient
answer
1 The most common site for venipuncture in a child is the foot vein. Thus, the choice of foot vein as a site for venipuncture in the child is correct. Venipuncture in the foot vein of an adult can cause thrombophlebitis and should be avoided. The hand vein should not be used for an ambulatory patient. The use of any extremity with a graft or fistula should be avoided in dialysis patients.
question
Which of the nurse's actions helps cause less irritation at the puncture site when discontinuing the IV? 1 Closing the roller clamp 2 Cleaning the site with antiseptic swabs 3 Removing the tape securing the catheter 4 Placing sterile gauze over the puncture site
answer
4 Placing sterile gauze over the puncture site while withdrawing the catheter can cause less irritation at the puncture site. Closing the roller clamp prevents fluid spillage. Cleaning the site with antiseptic swabs can help reduce microbial growth. Removing the tape securing the catheter can expose the catheter with minimal discomfort.
question
When should the peripheral intravenous dressing be changed? 1 If the flow rate decreases 2 If the tubing gets dislodged 3 If the intravenous site becomes moist 4 If the patient experiences pain at the intravenous site
answer
3 Moisture causes the catheter to become loose and increases the risk of contamination. Therefore, the nurse should change the dressing to retain the catheter. Pain at the intravenous site is due to phlebitis and infiltration; this occurs due to vascular assistive device (VAD) displacement. Flow rate decreases if the VAD placement is altered. The nurse should change the tubing of the intravenous line if it gets dislodged.
question
The nurse is changing the solution from an intravenous container when 50 mL of the fluid is remaining in the container. What is the rationale for this nursing action? 1 To reduce the contamination 2 To prevent the drying of the solution 3 To prevent the entry of air into the vein 4 To reduce the irregular flow of the fluid into the tube
answer
3 The solution should be changed when approximately 50 mL of the fluid is remaining in the container to prevent the air from entering into the tube and vein and to prevent the vein from clotting. Performing hand hygiene prevents contamination. Removing the spike from an old container and inserting it into the new container can prevent the solution from drying up. Changing the fluid in the container will not prevent the irregular flow of fluid.
question
Which statement is true regarding the use of different types of dressings for maintaining IV or vascular access device (VAD) sites? 1 Gauze dressings should be changed twice a day. 2 Transparent dressings should be changed every 48 hours. 3 Gauze dressings help to secure the vascular access device. 4 Transparent dressings are preferred over gauze dressings.
answer
4 Transparent dressings are the most commonly used dressings because of the reduced risk of soiling and moistening of these types of dressings. Gauze dressings should be changed every 48 hours. Transparent dressings are not changed until the intravenous tubing needs to be replaced. Transparent dressings may be changed only when compromised. Transparent dressings are used to secure the vascular access device.
question
While assessing a patient who is on intravenous therapy, the nurse finds edema around the insertion site. Which complication will the nurse document? 1 Phlebitis 2 Infiltration 3 Local infection 4 Circulatory overload
answer
2 Infiltration is a condition in which the intravenous fluid enters the subcutaneous tissue, causing edema at the insertion site. The nurse should discontinue the IV and elevate the extremity to reduce the edema. Phlebitis causes pain and redness at the insertion site. The nurse may start a new intravenous line at the other extremity to reduce the symptoms of phlebitis. A local infection manifests as redness and swelling at the insertion site, and occurs due to the passage of infection from the catheter skin point into the skin. The nurse should clean the skin and apply a sterile dressing to reduce local infection. Circulatory overload occurs due to excess extracellular fluid, which causes shortness of breath. The nurse should elevate the head of the bed to reduce the symptoms of circulatory overload.
question
A registered nurse teaches a nursing student about changing the intravenous fluid container. Which of the nursing student's statements indicates understanding? 1 "I should prepare the solution just before changing the container." 2 "I should cool down the solution to 15 to 18° C before fixing the container." 3 "I should coordinate the tubing changes with the intravenous fluid container." 4 "I should inform the patient that there is a chance he or she may feel a burning sensation during the change of containers."
answer
3 Coordinating the tubing changes with an intravenous fluid container reduces the frequency of opening the intravenous system and helps promote patient safety. The solution needs to be prepared at least an hour before needed and should be brought to room temperature if the solution is refrigerated. A burning sensation may occur while removing the intravenous catheter but not while changing the container.
question
While removing the catheter, the nurse places a sterile gauze pad over the venipuncture site. What are the benefits of this intervention? Select all that apply. 1 To control bleeding 2 To avoid trauma to the vein 3 To prevents the formation of a hematoma 4 Minimizes irritation at the puncture site 5 Reduces transmission of microorganisms
answer
1, 3, 4, 5 The nurse places a gauze pad over the venipuncture site and applies pressure on the site to control bleeding. Placing the gauze pad over the venipuncture site reduces hematoma formation. The nurse places a dry gauze pad over the venipuncture site to minimize irritation at the puncture site. The nurse should secure the dressing with tape to reduce the transmission of microorganisms. While removing the catheter hub from the skin, the nurse should place the hub parallel to the skin to avoid trauma to the vein.
question
The nurse uses an antiseptic swab for dressing a patient's intravenous site. What is the rationale for this? 1 To maintain skin integrity 2 To promote adherence of the dressing 3 To prevent irritation from the adhesives 4 To reduce the microbial count at the insertion site
answer
4 The nurse uses an antiseptic swab to clean the intravenous insertion site and reduce the microbial count at the insertion site. The nurse applies skin protectant solution on the intravenous insertion site to provide a protective coat over the skin to maintain skin integrity. Skin protectant solutions promote the adherence of the dressing, which reduces the irritation caused by the adhesive tapes.
question
How frequently should the peripheral vascular assistive device (VAD) site be assessed in neonates? 1 Every 10 minutes 2 Every hour 3 Every 2 hours 4 Every 4 hours
answer
2 The vascular assistive device (VAD) site of neonates should be assessed at least every hour. The site should be assessed every 5 to 10 minutes if a patient is being given vesicants or vasoconstrictors. The site should be assessed every 1 to 2 hours in critically ill patients and patients who are taking sedatives including those patients that would not be able to report problems at the insertion site. The site should be assessed every 4 hours in patients who are not using vesicant infusions.
question
A registered nurse teaches a nursing student about recording and reporting related to a peripheral intravenous dressing. Which of the nursing student's statements indicates a need for further learning? Select all that apply. 1 "I should document the patient's complications." 2 "I should record the reason for changing the dressing." 3 "I should record the description of the venipuncture site." 4 "I should record the number of peripheral dressings that were changed." 5 "I should report a significant change in the integrity of the system."
answer
1, 4 The nurse should immediately report any patient complications to the health care provider before documenting the complications. The number of peripheral dressings changed does not need to be recorded. The nurse should document the reason for changing the dressing. The nurse should record the description of the venipuncture site. The nurse should report significant changes in the integrity of the intravenous system.
question
The primary health care provider suggests that a patient who has an intravenous infusion in his hand should walk. Which nursing instructions are appropriate in this situation? Select all that apply. 1 "You should push the intravenous pole while walking." 2 "You should hold the intravenous pole with the freehand." 3 "You should tell the nurse if you find blood in the tubing." 4 "You should inform the nurse if you experience discomfort." 5 "You should tap the tubing if you observe stoppage in the flow."
answer
1, 3, 4 While providing instructions to a patient who is advised to walk with an IV infusion in his hand, the nurse should instruct the patient to push the intravenous pole while walking. The nurse should instruct the patient to report any observations of blood in the tubing. The nurse should instruct the patient to inform a nurse immediately if he or she experiences any discomfort. The nurse should instruct the patient to hold the pole with the involved hand. The nurse should instruct the patient to report to a nurse immediately if there is stoppage in the flow. The patient should not tap the tubing.
question
Why should the roller clamp be closed while preparing tubing using existing intravenous infusion? 1 To permit the flow of fluid 2 To prevent the spillage of fluid 3 To remove air from the tube 4 To prevent the complete infusion of fluid
answer
2 The roller clamp is closed to prevent the spillage of fluid from the tube. Placing the incision spike into the new tubing allows the flow of the fluid. Closing the roller clamp when full prevents the air from entering into the tube. Infusion of the fluid at a slow rate can prevent complete infusion of the fluid.
question
A nurse turns off a patient's electronic infusion device (EID), removes the tubing from the device, and closes the roller clamp while discontinuing the peripheral access. What is the reason behind this action? 1 To prevent discomfort at the site 2 To prevent microbial contamination 3 To prevent the formation of a hematoma 4 To prevent spillage of the intravenous fluid
answer
4 Turning off the electronic infusion device (EID) and closing the roller clamp while discontinuing the peripheral access can prevent the spillage of the intravenous fluid. Closing the roller clamp and turning off the EID may not prevent discomfort at the site. The use of aseptic technique prevents microbial contamination. Withdrawing the catheter slowly by applying light pressure can prevent the formation of a hematoma.
question
A nurse opens the roller clamp on the new tubing to allow the solution to run rapidly for 30 to 60 seconds. Which positive effect can be obtained by this action during continuous infusion? 1 Smooth transition 2 Spillage prevention 3 Occlusion prevention 4 Catheter stabilization
answer
3 A rapid flow for a brief period ensures occlusion prevention. A smooth transition can be obtained by removing the manufactured catheter stabilization device or tape from the tubing. Spillage can be prevented by closing the roller clamp, rather than opening it. Catheter stabilization may be achieved by forming a loop of tubing and securing it to the patient's arm with tape.
question
The primary health care provider tells the nurse to observe the intravenous connections and patency of systems of a patient who is on intravenous fluids. What is the rationale behind this order? 1 Detecting bleeding 2 Ensuring proper fluid administration 3 Maintaining pressure to prevent bleeding 4 Reducing the transmission of microorganisms
answer
2 Observing intravenous connections and the patency of systems ensures proper fluid administration to the patient. Observing the puncture site detects bleeding. Applying sterile folded gauze helps to prevent bleeding. Discarding the used supplies and performing hand hygiene reduces the risk of infection.
question
A primary health care provider asks a nurse to continue intravenous therapy for a patient. Which of the nurse's actions can promote the patient's safety? 1 Explaining the procedure to the patient 2 Arranging the equipment at the patient's bedside 3 Collecting appropriate equipment before the procedure 4 Coordinating the tubing changes with container changes
answer
4 While continuing intravenous therapy, the nurse should coordinate the tubing changes with the intravenous fluid container changes to promote patient safety by reducing the number of times the intravenous system is opened. The nurse should explain the procedure to the patient to promote the patient's cooperation during the procedure and reduce the patient's anxiety. The nurse should arrange the equipment at the patient's bedside and collect the appropriate equipment before the procedure to keep the procedure organized and maintain the procedural flow without interruption.
question
What is the frequency of assessing the peripheral vascular access device site in order to check the need for replacement in oriented adult patients? 1 Every 10 minutes 2 Every hour 3 Every 2 hours 4 Every 4 hours
answer
4 Oriented adults may experience problems at the vascular access device site. Thus, they should be assessed every 4 hours to check the need for vascular access device replacement. Checking every 10 minutes, every hour, and every 2 hours is too frequent and unnecessary.



