Classic Plus DNB Anesthesia – Flashcards
Unlock all answers in this set
Unlock answersquestion
Q. Propofol is used as the drug of choice for inducing anesthesia in which of the following situation? a. Neurosurgery b. Day care surgery c. Cardiac surgery d. In neonates
answer
Day care surgery Description: It is the induction agent of choice in day care surgery. The half life is 100 minutes, but the clinical effects of a single dose of propofol lasts only for 10 minutes due to its @ rapid redistribution. It has minimal residual impairment, anti emetic and anti pruritic property, making it a suitable drug for day care surgery. Ref: Essentials of Medical Pharmacology By KD Tripathi, 5th Edition, Page 343 Propofol Propofol is used as an anaesthetic agent for induction and maintainance. It is the induction agent of choice in day care surgery or other short term care like in emergency departments. The half life may be a few hours but the clinical effects of a single dose of propofol lasts only a few minutes due to rapid redistribution. The additional advantage of propofol is its anti emetic and anti pruritic property Other Facts: Propofol has poor analgesic effects Propofol is a broncodilator Propofol can cause hypotension Propofol can be used to control status epilepticus Propofol has antioxidant properties Exam Detail: AIPGME 2004 Ref: Trauma: Emergency resuscitation, perioperative anesthesia, surgical management, William C. Wilson, 2007, Page 370.
question
Q. Which one of the following is the fastest acting inhalational agent? a. Halothane b. Isoflurane c. Ether d. Sevoflurane
answer
d. Sevoflurane Description: There are two important partition coefficients that describe solubility of volatile agents in body tissues. One is the blood:gas (B:G) partition coefficient and the other the oil:gas (O:G) partition coefficient. The value of the oil:gas partition coefficient is determined by the lipid solubility of the anaesthetic agent. The blood-gas partition coefficient is a measure of the solubility of the inhalation anesthetic in the blood relative to its solubility in the inspired air. Circulating blood provides the means of anesthetic delivery to the brain and the partial pressure determines the rate of transfer into the CNS. The solubility of an agent in blood determines how rapidly the partial pressure rises in the blood. The blood gas partition coefficient (B/G coefficeint) is the @ most important factor in determining the uptake of agent and so the speed of induction and recovery. Agents with high solubility (large blood-gas partition coefficients) require large amounts of the anesthetic to dissolve in the blood before the partial pressure in the blood increases enough to effectively deliver them to the brain. Thus, agents with lower blood solubilities (small blood-gas partition coefficients) have more rapid rates of onset of anesthesia Desirable properties for inhalation anesthetic agents include high potency and low blood solubility. The halogenated hydrocarbons, such as desflurane and sevoflurane, fit these criteria and are used extensively. Agents with low B/G cofficient will have high alveolar concentration. So the induction and recovery will be fast with agents with less B/G coefficient and induction and recovery will be slower with agents with high B/G partition coefficient. Agents in increasing order of B/G coefficient (or decreasing order of induction & recovery): Ist - Most rapid induction- Desflurane(0.42) Cyclopropane(0.44) N20(0.47) Sevoflurane(0.69) Isoflurane(1.38) Eenflurane(1.8) Halothane(2.4) Chloroform(8) Trielene(9) Ether(12) Methoxyflurane(15) Ref: Short Textbook of Anaesthesia By Ajay Yadav; Handbook of Ambulatory Anesthesia By Rebecca S. Twersky, Beverly K. Philip, 2008, Page 186 http://usmleaid.blogspot.com/2013/04/blood-gas-partition-coefficient.html https://www.uam.es/departamentos/medicina/anesnet/journals/ija/vol3n2/inhal1.htm http://www.anesthesia2000.com/physics/Chemistry_Physics/physics1.htm http://www.rahulgladwin.com/noteblog/pharmacology/blood-gas-partition-coefficient.php http://www.anaesthetist.com/index.htm http://www.e-safe-anaesthesia.org/sessions/16_02/d/ANAE_Session/350/tab_402.html http://etherweb.bwh.harvard.edu/education/PHILIP/index.php http://anesthesiamd.blogspot.com/ http://www.anaesthesiamcq.com/ http://anaesthesia-database.blogspot.com/ http://www.anaesthesiauk.com/
question
Q. The laryngeal mask airway used for securing the airway of a patient in all of the following conditions, EXCEPT: a. In a difficult intubation b. In cardiopulmonary resuscitation c. In a child undergoing an elective/routine eye surgery d. In a patient with a large tumour in the oral cavity
answer
Description: Oropharyngeal abscess or mass is a contraindication to the use of laryngeal mask airway. Ref: Short Textbook of Anaesthesia By Ajay Yadav, 2nd Edition, Page 36 Laryngeal Mask Airway Laryngeal Mask Airway is a special type of airway useful in difficult intubation. It is placed blindly in the oropharynx and the cuff is inflated with large volume of air inflated cuff seals the lateral and posterior pharyngeal walls and patient can be ventilated through ventilation parts. Indications: a. Difficult airway management during cardiopulmonary resuscitation b. Difficult intubation is anticipated Contraindications: a. Oropharyngeal abscess or mass b. Conditions with high risk of aspiration c. Hiatus hernia d. Pregnancy Ref: Short Textbook of Anaesthesia By Ajay Yadav, 2nd Edition, Page 36
question
Q. The following modes of ventilation may be used for weaning off patients from mechanical ventilation, EXCEPT: a. Controlled mechanical ventilation (CMV) b. Synchronized intermittent mandatory ventilation (SIMV) c. Pressure support ventilation (PSV) d. Assist-control ventilation (ACV)
answer
Controlled mechanical ventilation (CMV) Description: Controlled Mechanical Ventilation (CMV) is best reserved for patients capable of little or no ventilator support. Ref: Short Textbook of Anaesthesia By Ajay Yadav 2nd Edition, Pages 182-3. Anaesthetic Procedures Controlled Mode Ventilation In Controlled Mode Ventilation (CMV) patients own effort is nil. Only ventilator is delivering the present tidal volume. This mode therefore will play NO ROLE in weaning a patient from mechanical ventilation. VT and ventilator rate is fixed regardless of patient effort and so it is not used for weaning patients from mechanical ventilation. Weaning Modes: a. Synchronized intermittent mandatory ventilation (SIMV). b. Pressure support ventilation (PSV). c. Assist-control ventilation (ACV). Ref: Short Textbook of Anaesthesia By Ajay Yadav 2nd Edition, Pages 182-3
question
Which of the following induction agent may cause adrenal cortex suppression? a. Propofol b. Ketamine c. Etomidate d. Thiopentione
answer
Description: Etomidate is an induction anaesthetic which cause suppression of production of steroids from adrenals. It is therefore not suitable for continuous intravenous use. It has brief duration of action (5-10min) and produce @ little cardiovascular and respiratory depression. It produce prominent motor restlessness and rigidity. Use of etomidate should be restricted to clinical situations in which its @@ hemodynamic stability offers a distinctive advantage over the other available induction drugs (e.g. elderly outpatients with clinically significant coronary artery or cerebrovascular disease). Ref: Essentials of Medical Pharmacology By K D Tripathi, 5th Edition, Pages 342-4
question
In a patient with fixed respiratory obstruction, Helium is used along with Oxygen instead of plain oxygen because: a. It provides analgesia b. It decreases turbulence c. It decreases oxygenation d. It decreases the dead space
answer
Description: Heliox is a mixture of 80% Helium and 20% O2. Its density is about ⅓ rd of air and has a low Reynolds number and hence low turbulence. It reduces the workload of breathing, improves dyspnea, and arterial blood gases in patients with fixed respiratory obstruction. It also decreases the chance for pneumothorax. Indications of Heliox Indications of Heliox: @ It is the anesthetic of choice in patients with acute distress from fixed respiratory tract obstructing lesions such as subglottic edema, foreign bodies and tracheal tumors. @ Helium mixtures may also be used as the driving gas for small-volume nebulizers for bronchodilator therapy in asthma. Ref: Clinical Anesthesiology By G. Edward Morgan, 4th Edition, Chapter 49 ; Principles of Critical Care By Jesse B. Hall, 3rd Edition, Chapter 40 Heliox gas mixtures are known to be nontoxic, noncarcinogenic, and have no lasting effects on any human organs. Nitrogen and helium have comparable viscosity, but helium has higher thermal conductivity compared to nitrogen. As a result, when a heliox gas mixture (79% helium and 21% oxygen) is produced, it has a viscosity similar to, but a density nearly six times lowers than atmospheric air. Due to its lower density, inhalation of heliox results in significantly lower turbulence, particularly in the more distal portions of the lung The decreased turbulence effect results in increased flow rates by up to 50% during heliox inhalation. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4093964/
question
Train of four fade is a characteristic feature of: a. Depolarizing block b. Non depolarizing block c. Both depolarizing and non-depolarizing block d. Malignant hyperthermia
answer
Description: Train of four fade is a characteristic of a non-depolarizing block. The Train-of-four stimulation denotes the administration of four successive 200-ps stimuli in 2 seconds (2 Hz) and a series of patterns are produced and these patterns differ in a depolarizing block differs from that of a non-depolarizing block. In a non-depolarizing block there is progressive depression of height with each twitch (fade) and in a depolarizing block there is equal depression of all four twitches (No fade). Ref: Clinical Anesthesiology By G. Edward Morgan, 4th Edition, Pages 152, 209. http://tmedweb.tulane.edu/pharmwiki/doku.php/nicotinic_antagonists Train of four fade Muscle responses to different patterns of nerve stimulation used in monitoring skeletal muscle relaxation. The fade associated with Non -depolarizing block helps in quantitative assessment of the non-depolarizing block. Train of Four Count: Observe and count the sequential disappearance of twitches. Disappearance of 4th twitch implies 75% block. Disappearance of 3rd twitch implies80% block. Disappearance of 2nd twitch implies 90% block. Train of Four Ratio: This is the ratio of amplitude of the 4th response to that of the first expressed as the percentage. It provides an estimation of the degree of non-depolarizing neuromuscular blockage. Ref: Clinical Anesthesiology By G. Edward Morgan, 4th Edition, Pages 152, 209.
question
Which of the following is the muscle relaxant of choice in renal failure? Rapacurium Pancuronium Atracurium Rocuronium
answer
Atracurium Description: A non-depolarizing neuromuscular blocking agent with short duration of action. @@ Its lack of significant cardiovascular effects and its lack of dependence on good kidney function for elimination provide clinical advantage over alternate non-depolarizing neuromuscular blocking agents. @@ Muscle relaxant of choice in renal failure is atracurium, since it is not eliminated through the kidney. The duration of neuromuscular block produced by Atracurium is approximately one third to one half the duration of block by d-tubocurarine, metocurine, and pancuronium at initially equipotent doses It is inactivated in the plasma by spontaneous non enzymatic degradation @@ (Hofmann elimination) in addition to that by cholinesterase. Ref: Essentials of Medical Pharmacology By K D Tripathi, 5th Edition, Page 314. Pancuronium Pancuronium is the longest acting nondepolarizing neuromuscular blocker. @ It has modest histamine releasing properties and vagolytic effects that may cause @ tachycardia and hypotension. Elimination - 50% is excreted unchanged, of which 80% appears in the urine. Of it, 40% is deacetylated in the liver to 3-hydroxy, 17-hydroxy and 3,17-dihydroxy derivatives which are eliminated in the bile. Ref: Essentials of Medical Pharmacology By K D Tripathi, 5th Edition, Page 314; Fundamentals of Anaesthesia By Tim Smith, Colin Pinnock, Ted Lin, 3rd Edition, Pages 617-18.
question
Which one of the following local anesthetics belongs to the ester group? a. Procaine b. Lignocaine c. Bupivacaine d. Mepivacaine
answer
Description: Procaine is an ester linked local anaesthetic. Bupivacaine, Lignocaine and Mepivacaine are amide linked local anesthetics. Other ester linked anesthetics are cocaine, chloroprocaine, tetracine and benzocaine. Ref: Essentials of Medical Pharmacology By K D Tripathi, 5th Edition, Page 320. Classification of Local Anaesthetics : (A). Surface anaesthetics (I). Soluble a. Cocaine b. Lignocaine c. Tetracaine d. Benoxinate (II). Insoluble a. Benzocaine b. Butylaminobenzoate (B) Injectable (I). Low potency, short duration: Procaine Chloroprocaine (II). Intermediate potency and duration a. Lignocaine b. Prilocaine (III). High potency and long duration a. Tetracaine b. Bupivacaine c. Ropivacaine d. Dibucaine Ref: Essentials of medical pharmacology By K D Tripathi 5th edition page
question
A patient is on regular medications for medical illnesses. Which of the drugs can be safely stopped with least adverse effects before an abdominal surgery? a. Statins b. Steroids c. Beta blocker d. Angiotensin receptor blocker
answer
Description: ACE inhibitors and angiotensin receptor blockers are known to cause severe and refractory intraoperative hypotension under anaesthesia. These drugs can be safely stopped with least adverse effects before an abdominal surgery. Patients on Beta blockers are advised to continue the drug prior to surgery because of its tendency to cause rebound hypertension if stopped. Patients taking 20 mg/day of prednisone or its equivalent for more than 3 weeks, have their HPA suppressed, so it should not be stopped prior to surgery due to the risks of adrenal insufficiency. @@ Statins are associated with a risk of rhabdomyolysis after surgery, so should be stopped prior to surgery. Ref: Essential Anesthesia: From Science to Practice By T. Y. Euliano, 2nd Edition, Page 20; Principles and Practice of Gynecologic Oncology By Richard R. Barakat, Page 238; Weight Loss Surgery: A Lighter Look at A Heavy Subject By Terry Simpson, Pages 5-19.
question
Which fibers are affected earliest in spinal anaesthesia? a. Sensory b. Motor c. Sympathetic preganglionic d. Vibration
answer
Description: Local anaesthetic solution injected into the subarachnoid space blocks conduction of impulses along all nerves with which it comes in contact, although some nerves are more easily blocked than others. Stimulation of the motor nerves causes muscles to contract and when they are blocked, muscle paralysis results. Sensory nerves transmit sensations such as touch and pain to the spinal cord and from there to the brain, whilst autonomic nerves control the caliber of blood vessels, heart rate, gut contraction and other functions not under conscious control. @@ Generally, autonomic and sensory fibres are blocked before motor fibres. Sensory loss can best be assessed by testing temperature sensation using an alcohol swab. First touching the patient with the damp swab on the chest or arm (where sensation is normal), so that they appreciate that the swab feels cold. Then work up from the legs and lower abdomen until the patient again appreciates that the swab feels cold. The level of sympathectomy can be best assessed with light pin pricks moving from nipple line down. The primary afferent nerve fibres have been divided into seven different groups depending on their function. Aa - Somatic motor and proprioception Ab - Touch and pressure - circumvent the dorsal horn by giving off collaterals that ascend in the posterior columns Ag - Proprioception, motor to muscle spindles Ad - Pain, cold temperature and touch (pin prick) - synapse in Rexed's lamina I of the dorsal horn. B - Autonomic preganglionic C dorsal root - Pain, Temperature , mechanoreception and reflex responses - synapse in Rexed's lamina II (the substantia gelatinosa) of the dorsal horn. C sympathetic - Postganglionic sympathetics Peripheral nerve functions are not affected equally by local anestethics. Loss of sympathetic function usually occurs first, followed by loss of pin-prick sensation( A delta) , tough, and temperature, and lastly, motor function. This phenomenon is called differential blockade. Differential blockade may be due to a. the size of the nerve b. the presence or absence of myelin and c. firing frequency. a. Size of nerve. Local anesthetics preferentially block small fibers because the distance over which such fibers can passively propagate an electrical impulse (related to space constant) is shorter. During the onset of local anesthesia, when short sections of nerve are blocked, the small-diameter fibers are the first to fail to conduct. b. Presence or absence of myelin. For myelinated nerves, three successive nodes must by blocked to halt impulse propagation. The thicker the nerve fiber, the farther apart the nodes tend to be-which explains, in part, the greater resistance to block of large fibers (e.g., motor fibers to skeletal muscle). @@ Myelinated fibers tend to become blocked before unmyelinated fibers of the same diameter. For this reason, the PREGANGLIONIC B FIBERS may be blocked (i.e., sympathetic fiber block leading to vasadilation and hypotension) before the smaller unmyelinated C fibers (carrying pain sensation). c. Firing frequency. Another important reason for preferential blockade of sensory fibers follows directly from the state-dependent mechanism of action of the local anesthetics. Block by these drugs is more marked at higher frequencies of depolarization and with longer depolarizations. Sensory fibers, especially pain fibers, have a high firing rate and a relatively long action potential duration (up to 5 msec). Motor fibers fire at a slower rate and have shorter action potential duration ( B > C Sensitivity to Hypoxia : B > A > C Sensitivity to Local Anaesthetic : A gamma & A delta > A alpha & A beta > B > C Miller's Anaesthesia (7th ed , pg 921 , 922 ) "Different fiber types are differentially sensitive to local anesthetic blockade. In vivo experiments show unequivocally that small myelinated axons (Aγ motor and Aδ sensory fibers) are the most susceptible to impulse annihilation. Next in order of block are the large myelinated (Aα and Aβ) fibers, and the least susceptible are the small, nonmyelinated C fibers. In fact, in this last group, impulses in the slowest conducting population (conduction velocity of 0.5 to 0.8 msec) are the most resistant to local anesthetic. The generalized notion that local anesthetics block the smallest fibers first or most is clearly wrong. " - See more at: http://www.mediconotebook.com/2013/01/spinal-anaesthesia.html#sthash.cINvkng6.dpuf. http://www.pitt.edu/~regional/Spinal/Spinal.html https://www.openanesthesia.org/neuraxial_anesthesia_anesthesia_text/ http://www.anaesthetist.com/anaes/drugs/Findex.htm#locals.htm http://www.fastbleep.com/medical-notes/other/15/31/528 http://www.nysora.com/mobile/regional-anesthesia/foundations-of-ra/3492-local-anesthetics-clinical-pharmacology-and-rational-selection.html http://www.backtobackguidetospinalanaesthesia.com/drug-action/mechanisms-of-spinal-anaesthesia.html
question
All of the following are complications of epidural anesthesia EXCEPT: a. Headache b Hypotension c. DIC d. Epidural hematoma
answer
c. DIC Description: Minor adverse effects and complications of epidural nerve block include pain at the injection site, headache, hypotension, unintentional dural puncture, and vasovagal syncope. Major complications include damage to neural structures, epidural hematoma, and epidural abscess. DIC is not associated with epidural anaesthesia.
question
Which of the following intravenous induction agent is most suitable for day care surgery? Morphine Ketamine Propofol Correct Diazepam Description:
answer
Propofol is the most suitable intravenous induction agent for day care surgery, because it is associated with a faster recovery and early return of psychomotor functions. Propofol is primarily a @@ hypnotic. It acts by promoting the function of the b1 subunit of GABA through activation of the chloride channel and thereby enhancing inhibitory synaptic transmission. Propofol also inhibits the NMDA subtype of glutamate receptor through modulation of channel gating. This action may also contribute to the drug's CNS effects. The hypnotic action of propofol is @@ pressure reversible, and it adheres to the correlation exhibited by other general anesthetics between anesthetic potency and octanol/water distribution coefficient. @@ Unlike barbiturates, propofol is not antianalgesic. @ Propofol at subhypnotic doses helps in the diagnosis and treatment of central, but not neuropathic, pain.
question
Which of the following represents the concentration of adrenaline which is used with lidocaine ? 1:200 1:2000 1:20000 1:200000
answer
1:200000 Description: Lidocaine stabilizes the neuronal membrane by inhibiting the ionic fluxes required for the initiation and conduction of nerve impulses, thereby effecting local anesthetic action. Epinephrine, in concentrations of 5 mcg/ml, is commonly used to decrease the absorption of local anesthetics. A 5 mcg/ml (1:200,000) dose of epinephrine will significantly reduce the peak blood levels of @@ lidocaine and mepivacaine regardless of the site of administration. Epinephrine does not affect the vascular absorption of @@ etidocaine and bupivacaine in the epidural space. However, the addition of epinephrine does significantly reduce the vascular absorption of etidocaine and bupivacaine when utilized for peripheral nerve blocks. Benefits of decreased absorption include increased neuronal uptake, enhanced quality of analgesia/anesthesia, prolonged duration of action, and decreased risk of toxicity. A concentration of 1:200,000 (5 mcg/ml) is commonly used for peripheral nerve blocks to reduce vascular absorption. Use of Additives with Local Anesthetic Solutions : 1. @ Sodium bicarbonate raises the pH of local anesthetics (making it less acidic or closer to pKa) and increases the unionized form of local anaesthetic. This increases the rate of diffusion across the nerve sheath and the nerve membrane and increases the speed of onset of anaesthesia. It also prolongs the duration and intensity of block and @ reduces pain of injection (which is associated with low pH & cold solution). The recommended dose is 1 ml of 8.4% NaHC03 per 10 ml of LA. 2. Epinephrine (Adrenaline) increases speed of onset of epidural block, enhances both spread & quality of block. It also prolongs effect of lignocaine & reduces peak local anesthetic blood level & toxicity by reducing the local blood supply and delaying its uptake. 3. Dextrose 3 - 5% , is added to subarachnoid LA solutions to adjust the baracity of solution in relation to CSF. 4. Narcotics (opioids) are used in intraspinal solutions as analgesic agents. Ref: Miller's Anesthesia, 6th Edition, Pages 579-95; Katzung and Trevor's Pharmacology Examination and Board Review, 10th Edition, Page 419.
question
All of the local anaesthetics given below are amides, EXCEPT: a. Lignocaine b. Procaine c. Prilocaine d. Etidocaine
answer
b. Procaine The members of Amide group are: Articaine Bupivacaine Cinchocaine/Dibucaine Etidocaine Levobupivacaine Lidocaine/Lignocaine Mepivacaine Prilocaine Ropivacaine Trimecaine
question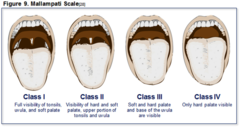
All of the following are related to difficult intubation, EXCEPT: Miller's sign TMJ ankylosis Increased thyromental distance Micrognathia
answer
Description: Tracheal intubation is best achieved in the classic "sniffing the morning air" position in which the neck is flexed and there is extension at the cranio-cervical (atlanto-axial) junction. This aligns the structures of the upper airway in the optimum position for laryngoscopy and permits the best view of the larynx when using a curved blade laryngoscope. Abnormalities of the bony structures and the soft tissues of the upper airway will result in difficult intubation. Signs of difficult intubation: Thyromental distance < 7 cms Mallampatti grade III or IV Micrognathia Macroglossia High arched palate with narrow dental arch TMJ limitation Limited cervical vertebrae extension Miller sign Growth in oral cavity The modified Mallampati, thyromental distance, ability to protrude the mandible and craniocervical movement are probably the most reliable.
question
Which of the following anaesthetic agent causes bone marrow supression? Halothane Ketamine Nitrous Oxide Isoflurane
answer
Nitrous Oxide Description: Nitrous oxide may cause bone marrow supression by interfering with the production of factors necessary for DNA synthesis. Nitrous oxide has few adverse effects, it is a mild @ cardiac depressant and @ pulmonary vasoconstrictor and is @@ relatively contraindicated in patients with pulmonary hypertension. It cause diffusional hypoxia. @ It inhibits folate metabolism and is contraindicated in pregnancy. @ It promote expansion of internal gas-filled structures, and is avoided in patients with pneumothorax, pneumocephalus, and vascular air embolism.
question
Which muscle is most resistant to neuromuscular blockage? Diaphragm Ocular Adductor pollicis Intercostal muscles
answer
Description: All muscles in the body do not have equal sensitivity to muscle relaxants. The diaphragm is most resistant to neuromuscular blockade. @@ Neck and pharyngeal muscles which support the airway are most sensitive to neuromuscular blockade. There is increasing evidence that residual neuromuscular block is common, and also that it may adversely affect patient outcome. Significant pulmonary morbidity has been demonstrated after using longer-acting agents such as pancuronium When neuromuscular monitoring is used, visual or tactile evaluation of the degree of neuromuscular block is unreliable. Even experienced anaesthetists are unable to detect fade when the TOF ratio is >0.4. It is now thought that significant residual curarization is still present if the TOF ratio is <0.97 (not 0.7 as previously suggested8). On recovery, the anaesthetist can assess muscle power by a variety of clinical tests, such as the ability to sustain head lift for 5 s,8 or the ability to hold a tongue depressor between the teeth The degree of neuromuscular block can be assessed by applying a supramaximal stimulus to a peripheral nerve, and then measuring the associated muscular response. During induction of anaesthesia and tracheal intubation, the muscles of the larynx and jaw must be paralysed as well as the diaphragm. @@ The orbicularis oculi is probably the ideal muscle to monitor at this time as it is more similar to a central muscle: onset of block will be similar to the laryngeal muscles and diaphragm. The following clinical signs are listed in order of increasing block: 1. Diplopia, weakness of extra-ocular muscles 2. Perception of weakness or heaviness 3. Difficulty swallowing 4. Inability to sustain headlift, decreased peak insp. force 5. Obvious weakness, poorly sustained grip 6. Decreased vital capacity, flow rates 7. Jerky movements Intercostal paralysis, respiratory failure 8. Diaphragmatic paralysis http://sydney.edu.au/medicine/anaesthesia/resources/lectures/
question
All are true about xenon anaesthesia, except Rapid induction and recovery Low potency Non explosive High blood solubility
answer
High blood solubility Description: Xenon is 4.5 times heavier than air. It is an inert gas. Blood gas partition coefficient is 0.14. It has low blood solubility.
question
Anesthesia of choice for induction in day care surgery is? Propofol Ketamine Halothane Pancuronium
answer
Propofol is a sedative-hypnotic intravenous anesthetic agent. It is the induction agent of choice in day care surgery. Properties include, Early induction Smooth recovery Decreased incidence of post operative nausea and vomiting



