BCH B – Flashcard
Unlock all answers in this set
Unlock answersquestion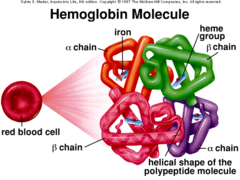
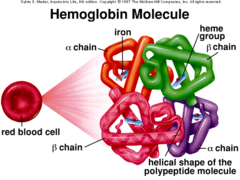
Hemoglobin
answer
A four-subunit protein found in red blood cells that binds oxygen. Each subunit contains a heme group, a large multi-ring molecule with an iron atom at its center. One hemoglobin molecule can bind four oxygen molecules in a cooperative manner
question
Molecular structure of hemoglobin
answer
1. Quaternary structure; 2 alpha chains (polypeptides), 2 non-alpha chains 2. Predominantly alpha helical 3. Four heme groups; one per subunit, planar porphyrin ring system
question
Heme
answer
The iron-containing nonprotein fraction of hemoglobin. Planar porphyrin ring system with ferrous iron (Fe2+) bound at center
question
What state must iron be in?
answer
Ferrous ion state or Fe2+. It is crucial that Fe2+ state because if it is at the Fe3+ (ferrite state) oxygen cannot bind
question
Free heme vs protein-bound (ligand binding)
answer
Another molecule that can bind to the Fe2+ is carbon monoxide. CO can bind 20000x more efficiently that O2. Another protein-bound molecule can sterically hinder CO and reduce the effectiveness to only 200x when compared to O2
question
Myoglobin and alpha & beta globins share _____ primary sequence identities
answer
Few. Very different at the primary structure
question
Secondary structure is _________ between alpha & beta globins
answer
Similar
question
Tertiary structure of hemoglobin is shaped very _____ to myoglobin
answer
Similarly
question
When does hemoglobin begin to look much more different than myoglobin?
answer
Quaternary (4th) structure
question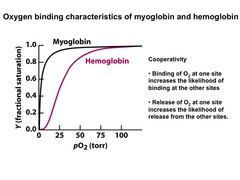
What is the shape of the oxygen-binding curve of myoglobin?
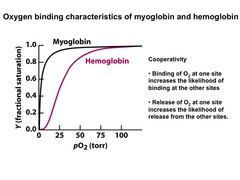
answer
Hyperbolic
question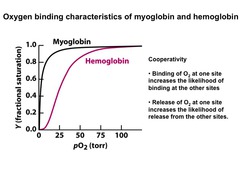
What is the shape of the oxygen-binding curve of hemoglobin?
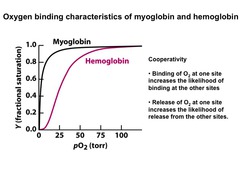
answer
Sigmoidal or "S-shaped" curve. Binding affinity of each heme group changes as the amount of oxygen is bound to the hemoglobin
question
Derivation of Hb oxygen-binding curve
answer
1. In high O2 conditions (lungs), Hb is in state to bind O2 2. In low O2 conditions (tissues), Hb is in state to release O2 We get this sigmoidal curve from the transition of the low and high-affinity curves
question
T state
answer
Tight/taut state is a low-affinity or deoxyHb (w/o oxygen). Is more open (looks like a doughnut) with salt bridges formed
question
R state
answer
Relaxed state is a high-affinity state with oxygen
question
Salt bridges
answer
Interactions with positive and negative charges. Salt bridges stabilize the structure of each polypeptide which does not favor the oxygen binding
question
Salt bridges stabilize what state?
answer
T State. O2 binding disrupts salt bridges
question
Transition from T to R state
answer
There are many transition states between the T and R states of hemoglobin
question
Biochemical basis of Bohr Effect
answer
In periphery we have a lower pH (more acidic). HHb+ + O2 HbO2 + H+
question
What contributes to salt bridge formation and favors T (deoxy) state
answer
Protonation
question
What decreases hemoglobin's affinity for O2?
answer
BPG
question
BPG
answer
Byproduct of glycolysis. Without BPG the hemoglobin begins to look more like myoglobin which helps shape the hemoglobin sigmoidal curve. More BPG shifts the curve to the right (right-shift) which can release more oxygen. Binding of BPG stabilizes T (deoxy) state; likes to bind to the "middle of the doughnut" to stabilize the T-state
question
Which of the following would be true for an acidemic patient? A. Their hemoglobin has an increased affinity for oxygen; B. Their hemoglobin has a decreased affinity for BPG; C. Their oxygen dissociation curve is shifted to the right; D. Their hemoglobin is more likely to be in the relaxed state
answer
C. Their oxygen dissociation is shifted to the right. Correct statements: A. Their hemoglobin has a decreased affinity for oxygen B. Their hemoglobin has an increased affinity for BPG D. Their hemoglobin is more likely to be in the T state
question
Right-shift favors . . .
answer
Increased H+, lower pH, decreased affinity for O2 - more like T-state
question
Left-shift favors . . .
answer
Decreased H+, higher pH, increased affinity for O2 - more like R-state
question
Chromosome 16

answer
Has alpha like genes. Genes on the left are expressed earlier and developmentally expressed later
question
Chromosome 11

answer
Has non-alpha like genes. Genes on the left are expressed earlier and developmentally expressed later
question
alpha2 and alpha1 duplication
answer
1. Differ only in promoters 2. Alpha2 promoter is stronger 3. Alpha2:Alpha1 expression is 2:1
question
Mutation in what alpha gene is more severe?
answer
Alpha2
question
Ggamma and Agamma duplication
answer
1. Gly and Ala substitution 2. Functionality, performance, expression level are identical 3. No biological or disease significance
question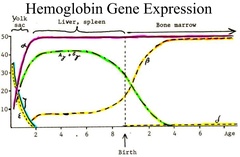
Developmental expression of heme genes
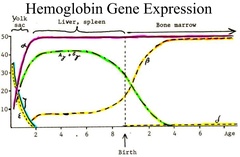
answer
Please see picture
question
Structure of HbA
answer
Alpha2Beta2. Percentage of normal hemolysate (individuals more than 8 months old) = 92.5%
question
Structure of HbA2
answer
Alpha2Delta2. Percentage of normal hemolysate = 2.5%
question
Structure of HbA1c
answer
Alpha2(Beta-N-glucose)2. Percentage of normal hemolysate = 4.0%
question
What is HbA1c increased in? Decreased in?
answer
Increased in DM. Decreased in hemolytic anemia
question
Structure of HbF
answer
Alpha2Gamma2. Percentage of normal hemolysate = less than 1%
question
What is HbF increased in?
answer
Increased in Beta Thalassemia
question
Structure of HbH
answer
Beta4. Percentage of normal hemolysate = 0%
question
What is HbH increased in?
answer
Increased in Alpha Thalassemia
question
Structure of Hb Bart's
answer
Gamma4. Percentage of normal hemolysate = 0%
question
What is Hb Bart's increased in?
answer
Increased in Alpha Thalassemia
question
Oxygen affinity of HbF (Alpha2Gamma2) vs. HbA (Alpha2Beta2)
answer
1. Gamma chain vs. Beta chain - 72% identical 2. One important difference is gamma chain has a Ser instead of His 3. Binds BPG with reduced affinity 4. Affinity for O2 is increased and HbF (fetal version) can take O2 from HbA (from mother)
question
Thalassemias
answer
Single most common defect - decreased production of a globin chain - "right protein, wrong amount"
question
Hemoglobinopathies
answer
"Wrong protein, right amount"
question
Alpha Thalassemias
answer
1. Decreased Alpha, surplus Beta (and Gamma) 2. Principal etiology is complete deletion of an alpha gene 3. More common, less dangerous Less dangerous because there are two alpha genes. HbH and HbBarts tend to resemble R-state and are unstable. Complete loss of alpha is fatal in the fetal stage
question
Fate of surpluse Beta and Gamma chains (Alpha Thalassemias)
answer
Form soluble tetramers Beta4 (HbH) or Gamma4 (Hb Bart's) - unstable 1. Can precipitate, forming insoluble inclusions (Heinz bodies) 2. High affinity, no cooperativity, poorly release O2 in tissue, P50 = ~2 mmHg
question
Beta Thalassemias
answer
1. Decreased Beta, surplus Alpha 2. Principal etiology is small substitution or deletion mutation of a Beta gene 3. Less common, more dangerous More dangerous because there is only a single Beta gene. Beta Thalassemias would be more apparent post-natal (after birth)
question
Fate of surplus Alpha chains (Beta Thalassemias)
answer
Cannot tetramerize - polymerize into tactoid structures (insoluble aggregates) which distort the erythrocyte and stress the membrane - severe hemolysis; extreme cases must be treated by transfusion therapy
question
Hemoglobin S - Beta-globin defect (Hemoglobinopathies)
answer
1. Substitution of Valine and Glutamate at the 6th position 2. Creates a hydrophobic "sticky patch" 3. Complementary sticky patch is exposed in deoxy state 4. Sticky patches interact to form fibrous aggregates (tactoids) at low PO2 5. Hemolytic and vaso-occlusive
question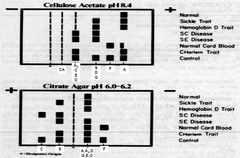
Hemoglobin Electrophoresis
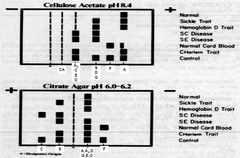
answer
Please see picture
question
Potential therapies for hemoglobin-related diseases
answer
1. Bone marrow transplant (cure) 2. Blood transfusions (and possibly iron chelation therapy) 3. Hydroxyurea treatment to stimulate synthesis of Gamma chains (and HbF) - for Beta globin diseases
question
How might synthesis of Gamma chains help a sickle cell patient?
answer
Formation of HbF helps prevent HbS formation
question
Characteristics of benign tumors
answer
1. Benign tumors are localized and encapsulated (not invasive) 2. Benign tumor cells are more differentiated than cells in malignant tumors; very easy to tell benign tumor cells from normal tissue
question
Characteristics of malignant tumors (cancers)
answer
Invasive and/or metastatic; very difficult to find border of malignant tumors with normal tissue. Locally invasive tumors are also cancers
question
Note on invasive tumors and surgery
answer
Invasive, invade into surrounding normal tissues, making boarders between cancer and normal tissue difficult to define. That is also the reason that sometime surgeons thought they removed all the tumor cells, but the tumor grew back later on or even spread to other places. Thus, in most cases, surgeons try to remove not onl y the tumor but also tumor's surrounding tissues as much as possible. Locally invasive tumors are cancers. All cancers are invasive but not all cancers are metastatic, brain cancer is usually nonmetastatic. Malignant tumors usually start as benign tumors, they become malignant only after they become invasive
question
What is cancer?
answer
A term for diseases in which abnormal cells divide without control and can invade nearby tissues. Cancer cells can also spread to other parts of the body through the blood and lymph systems (metastasis). An invasive growth or tumor that is likely to metastasize to other sites without surgery or treatment. 1. Uncontrolled growth and spread 2. Invasive growth that is likely to spread
question
Metastasis
answer
1. Is the spread of cancer from one organ or part to another NON-ADJACENT organ or part. 2. Cancer cells can break away, leak, or spill from a primary tumor, enter LYMPHATIC AND BLOOD VESSELS, circulate through the bloodstream, and be deposited within normal tissue elsewhere in the body 3. Is a complex MULTI-STEP process, usually at the LATE STAGE of cancer 4. Involves malignant cells break away, attach to and degrade proteins that make up the surrounding EXTRACELLULAR MATRIX (ECM), ESCAPE, AND ESTABLISH SECONDARY TUMORS
question
Stages in tumor growth and metastasis
answer
1. A single modified cell appears in a tissue 2. Division of the single modified cell. Tumor is still BENIGN AT THIS STAGE; As long as it is not invading its surrounding normal tissues, the tumor is still considered as benign 3. Invasion of the basal lamina by the tumor cells (may accompany with angiogenesis) 4. The tumor cells spread into blood vessels that will distribute cancer cells to other sites
question
Oncogenesis
answer
A multi-step, dynamic and evolutionary process, with each step corresponding to a different genetic mutation(s) in different genes
question
Angiogenesis
answer
Is the formation of new blood vessels in and around tumor. The purpose of angiogenesis is for tumor to obtain more nutrients for faster growth and proliferation
question
Carcinomas (types of cancers)
answer
Cancers of epithelial cells (~90%)
question
Sarcomas (types of cancers)
answer
Cancers of the supporting tissues such as bone, cartilage, fat, connective tissue, and muscle
question
Leukemias (types of cancers)
answer
Cancers of hemopoietic cells (in bone marrow)
question
Lymphomas and myelomas (types of cancers)
answer
Cancers that arise in the immune system
question
Central nervous system cancers (types of cancers)
answer
Cancers that begin in the tissue of the bran and spinal cord
question
Six hallmarks of cancer in 2000
answer
1. Sustaining proliferative signaling 2. Evading growth suppressors 3. Activating invasion and metastasis 4. Enabling replicative immortality 5. Inducing angiogenesis 6. Resisting cell death
question
Sustaining proliferative signaling (hallmarks of cancer in 2000)
answer
Oncogenic signaling
question
Evading growth suppressors (hallmarks of cancer in 2000)
answer
Loss of tumor suppression
question
Activating invasion and metastasis (hallmarks of cancer in 2000)
answer
Invasion and metastasis
question
Enabling replicative immortality (hallmarks of cancer in 2000)
answer
Telomere and telomerase
question
Inducing angiogenesis (hallmarks of cancer in 2000)
answer
New blood vessel formation
question
Resisting cell death (hallmarks of cancer in 2000)
answer
Resistance of apoptosis
question
Four emerging hallmarks of cancer since 2010
answer
1. Avoid immune destruction 2. Tumor-promoting inflammation 3. Genome instability and mutation 4. Deregulating cellular energetics
question
Avoiding immune destruction (hallmarks of cancer since 2010)
answer
Immuno-evasion
question
Tumor-promoting inflammation (hallmarks of cancer since 2010)
answer
Inflammation (enabling characteristics)
question
Genome instability an mutation (hallmarks of cancer since 2010)
answer
Cancer genomics (enabling characteristics)
question
Deregulating cellular energetics (hallmarks of cancer since 2010)
answer
Cancer metabolism
question
Cancer rates are genetically, environmentally, and culturally influenced
answer
You will find that different countries have different rates for different cancers and some cancers with low occurrence rates may be the cancer of highest occurrence rate in other countries. Skin cancer for Australia (sun and UV exposure), liver cancer in China due to large population of people infected with hepatitis B, Colon cancer in the US due to high consumption of meat and red meat
question
In addition to genetics, what other factors play significant roles in oncogenesis?
answer
Environment and culture (diet in this case). Take Japanese people and Americans as examples. Japanese people living in Japan have very low level of colon cancer. However, if they immigrate to the US, their colon cancer rate increases many fold, close to the rate of Americans. On the other hand, Japanese people living in Japan have very high rate of stomach cancer. Once they come and live in the US, their stomach cancer rate is significantly decreased. These changes are attributed to the diet changes. Thus, environmental and cultural factors either contribute or reduce cancer occurrence rates
question
Diet's role on certain cancers
answer
Diet and fat/calorie consumption play significant role in certain types of cancer (breast cancer is another example). For example, Americans eat significantly more meat than Japanese people and meat consumption has been well correlated to colon cancer rates. The higher the meat consumption rate, the higher the colon cancer rates. Breast cancer rates are also correlated with caloric intake
question
Cancer lag time
answer
1. There is a good correlation between smoking and lung cancer 2. There is a delay (lag time) of ~20-30 years between smoking and lung cancer
question
How many signaling pathways and processes are found to be mutated and disregulated in pancreatic caner? Mutations in more than how many genes are identified and involve?
answer
13 and 40 respectively. Similar results are also found in brain cancer, breast cancer, and colon cancer
question
Key information from genomic studies of cancer
answer
1. Multiple genetic mutations are needed for cancer to develop 2. Different cancer requires (contains) different number of genetic (gene) mutations 3. Mutations in both tumor suppressor genes and proto-oncogenes are needed for cancer to develop
question
What two types of cancers contain the most genetic mutations?
answer
Skin and lung cancer. Skin cancer and lung cancer can have more than mutations in more than 100 genes. This is not surprising because our skin and lung are exposed to most carcinogens . UV and air are the major causing factors
question
Driver genes
answer
The most important gene mutation(s) at a given stage for oncogenesis to proceed. Drivers may be (usually are) different at different stages of oncogenesis
question
Rider genes
answer
gene mutations that play a very small or no roles in oncogenesis at certain stages
question
Key importance of driver and rider genes
answer
Drivers can change into riders and riders can change into drivers at different stages of oncogenesis. Try always to target drivers. It also means that the treatment need to change if drivers are changed in the cancer
question
Effective anticancer therapies are those that target driver or rider genes?
answer
Driver genes
question
The development an metastasis of human colorectal cancer and its genetic basis
answer
1. Loss of APC tumor suppressor gene 2. Activation of K-ras oncogene 3. Loss of DCC tumor suppressor gene 4. Loss of p53 tumor-suppressor gene 5. Other changes in genes whose products are involved in assisting metastasis; same cancer from different people may have different mutations in different sets of genes (or different sequence of mutations)
question
Summary of the causes of cancer and oncogenic process
answer
1. By mutations in genes that are involved in various aspects (processes) of cell growth. 2. By oncogenes and mutations of tumor suppressor genes 3. Oncogenesis is a complex and multi-step evolving and dynamic process 4. Caused and maintained by genetic mutations and by altered cell metabolism (cancer metabolism)
question
Cancer stem cell hypothesis
answer
Hypothesis: Tumors often originate from the transformation of normal stem cells, similar signaling pathways may regulate self-renewal in stem cells and cancer cells, and cancer cells include 'cancer stem cells' — rare cells with indefinite potential for self-renewal that drive tumorigenesis Observations: Cancer cells are fast replicating and usually less-differentiated, and immortal cells
question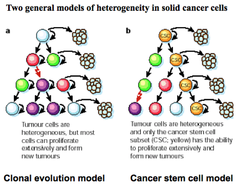
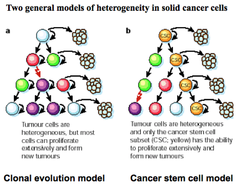
Cancer stem cell model
answer
Tumor cells are heterogeneous and only the cancer stem cell subset (CSC; yellow) has the ability to proliferate extensively and form new tumors. CSC model is well established
question
Clonal evolution model
answer
Tumor cells are heterogeneous, but most cells can proliferate extensively and form new tumors
question
Cancer stem cells (CSC)
answer
1. Cancers have cancer stem cells that are responsible for most of the cancer growth, metastasis, and drug resistance 2. Different cancers have different CSC (different cell surfacemarkers) 3. Different cancers have different percentage of CSC 4.. CSC has become a new therapeutic target in cancer treatment
question
Proto-oncogenes
answer
NORMAL CELLULAR GENES that encode proteins involved in various aspects of cell growth and cell proliferation
question
Oncogene
answer
Cancer-producing genes that are DERIVED FROM PROTO-ONCOGENES BY VARIOUS TYPES OF GENETIC MUTATIONS
question
Proto-oncogenes and oncogenes are . . .
answer
Growth (cell proliferation) promoting genes
question
Tumor suppressor genes are . . .
answer
Growth-suppressing (-decelerating or-inhibiting) genes
question
What are the seven types of proteins that participate in controlling cell growth (any may be involved in oncogenesis)
answer
1. Growth factors 2. Growth factor receptors 3. Intracellular transducers 4. Transcription factors 5. Pro- or Anti-apoptosis proteins 6. Cell-cycle control proteins 7. DNA-repair proteins Cancer results from expression of mutant forms of these proteins
question
Growth factors in cancer
answer
Normal growth factors (proteins) become oncogenic when they are OVER-EXPRESSED (over-produced)
question
Name two important proto-oncogene receptor proteins
answer
1. HER2 2. EGF Both are a receptor tyrosine kinase (RTK)
question
HER2
answer
The dimerized protein is constitutively active as a kinase - human breast cancer
question
What is an effective treatment for one type of breast cancer involving HER2 receptor?
answer
Herceptin is a very effective drug treating one type of breast cancer in which Her2 receptor gene is mutated into Neu gene
question
EGF receptor

answer
Dimerization of two receptor proteins in the absence of normal EGF-related ligand
question
What types of cancers is EGFR involved in?
answer
EGFR is involved in many types of lung cancers, drugs targeting different EGFR mutations are effective in treating lung cancers
question
Important of tyrosine kinases
answer
1. Mutated receptor tyrosine kinases and intracellular kinases are one type of key oncogenes 2. Many new targeted anticancer drugs target (inhibit) membrane bound tyrosine kinases or intracellular kinases - TKIs
question
Ras
answer
Is a GTP-binding protein. Constitutively active Ras protein leads to uncontrolled cell growth and cancer
question
Importance of Ras mutations (growth signal transducer)
answer
Ras mutations are found in more than 30% of all cancers. It is one of the most frequently mutated protooncogenes. Normal Ras can be in active and inactive states depending the cell needs. However, when Ras mutation occurs at aa position 12 or position 61, the Ras protein becomes active all the time - it is called constitutively active, transducing cell growth signal all the time, leading to cancer development
question
What are two important proto-oncogene products following serum stimulation of quiescent 3T3 cells?
answer
1. c-Fos 2. c-Myc One of the earliest effects of growth factors is to induce transcription of c-Fos and c-Myc proto-oncogenes
question
Fos and Myc
answer
Fos and Myc are two important transcription factors. Their activities are tightly controlled in normal cells and they are not in active state for long. However, in some cancer cells, you can find the Fos or Myc proteins are constitutively active, causing overexpression of genes involved in cell growth and lead to cancer
question
The types of genetic mutations in the gene mutations include (3)?
answer
1. Point or deletion mutations 2. Gene amplification 3. Chromosome rearrangement
question
A proto-oncogene can become an oncogene by?
answer
1. Mutations in the regulatory sequence; promoter 2. Mutations in the coding sequence in the gene 3. Chromosomal translocation 4. Gene amplification
question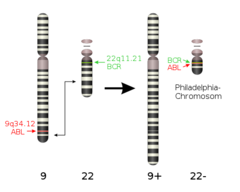
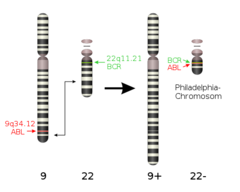
Philadelphia Chromosome
answer
Generated by the fusion or translocation of Ch 9 and Ch22, and the generation of a fusion gene of bcr and abl. Abl is a tyrosine kinase, the mutated bcr/able fusion protein becomes constitutively active, causing leukemia. Translocated chromosome in which part of chromosome 22 attaches to chromosome 9. Therefore, 22 becomes shorter and 9 becomes longer
question
What type of cancer is a result of the Philadelphia chromosome?
answer
CML
question
Tumor suppressor genes
answer
A tumor suppressor gene, or ANTI-ONCOGENE, is a gene that protects a cell from becoming cancerous. When this gene is mutated to cause a loss or reduction in its function, the cell can progress to become cancerous, usually in combination with other genetic changes
question
RB gene
answer
Is a tumor suppressor gene. Children wit hereditary retinoblastoma develop retinal tumors early in life and generally in both eyes. They inherit one mutant allele of the RB gene. Somatic mutation of the other allele coupled with oncogenic mutations in other genes leads to tumor development
question
Two-hit hypothesis
answer
Some forms of hereditary cancer might be initiated when a cell in a person heterozygous for a germline mutation undergoes a second, somatic mutation in the other allele of the same gene, thus rendering the cell homozygous for loss of function mutations in a tumor-suppressor gene and giving rise to a tumor
question
The two-hit origin of cancer theory applies only to what genes?
answer
Tumor suppressor genes, not oncogenes. It applies to the same tumor suppressor gene, not two different tumor suppressor genes
question
p53 gene
answer
1. Tumor suppressor, transcription factor 2. Mutated or deleted in > 50% of all human cancers 3. May be the most important gene in human cancer 4. Cause of the genetic diseases Li-Fraumeni Syndrome
question
The p53 gene is involved in (3)
answer
1. DNA damage repair 2. Cell cycle checkpoint control 3. Apoptosis
question
Normal function of oncogenes (proto-oncogene)
answer
Cell growth-promoting (proto-oncogene)
question
Normal function of tumor suppressor genes
answer
Cell growth-suppressing
question
Consequences of mutation/genetic trait of oncogenes (from proto-oncogenes)
answer
GAIN of function. Genetic trait: Dominant (one allele), somatic mutations
question
Consequences of mutation/genetic trait of tumor suppressor genes
answer
LOSS of function. Genetic trait: Recessive (both alleles) *but classified as dominant*, genetic inheritance
question
G1 phase
answer
Rapid growth and centriole replication. 8-10 hours
question
S phase
answer
Chromosome replication (DNA synthesis). 6-8 hours
question
G2 phase
answer
Growth and final preparations for cell division. 4 to 6 hours
question
Mitosis and Cytokinesis
answer
PMAT; Prophase, Metaphase, Anaphase, and Telophase followed by Cytokinesis
question
G1/S checkpoint of the mitotic cell cycle is controlled by what two genes?
answer
1. p53 2. RB
question
What proteins are used during the G2 phase of the mitotic cell cycle?
answer
Cyclins + CDKs; A group of proteins whose function is to regulate the progression of a cell through the cell cycle and whose concentrations rise and fall throughout the cell cycle
question
Telomere
answer
Is a region of repetitive DNA at the end of a chromosome, which protects the end of the chromosome from destruction (similar to the plastic caps at the ends of shoelace)
question
What replenishes telomeres after they are shortened during cell division?
answer
Telomerase
question
Senescence
answer
Aging of the cell. As telomeres grow shorter, eventually cells reach the limit of their replicative capacity and progress into senescence
question
What happens to the telomere in cancer cells?
answer
Cell would die when it telomere shortens and can no longer multiple; however telomere stays long in cancer cells. Telomere shortening can induce replicative senescence which blocks cell division. This mechanism prevents genomic instability and development of cancer in aged cells by limiting the number of cell divisions. Cancer cells which bypass this arrest become immortalized by telomere extension mostly due to the activation of telomerase, the enzyme responsible for synthesis of telomeres
question
Compared to normal cells, cancer cells' telomerase activity is ________ and telomeres are _________ - two of the key reasons that cancer cells are immortalized
answer
Higher, longer respectively
question
RNA and DNA viruses as cancer-producing agents
answer
1. Both RNA and DNA viruses can carry oncogenes 2. Both RNA and DNA viruses can induce cancer in animals and humans
question
Oncogenes that function in viral replication cycle are characteristic of what type of virus?
answer
DNA virus. Oncogenes carried by RNA viruses do not have functions in viral replication cycle, whereas oncogenes carried by DNA viruses do participate in the replication cycle of viral hosts. Oncogenic mechanisms of the oncogenes carried by RNA viruses are very different from those of the oncogenes carried by DNA viruses
question
Epstein-Barr virus can lead to what type of cancer?
answer
Burkitt's Lymphoma
question
HPV can lead to what type of cancer?
answer
Cervical cancer
question
Hepatitis B virus can lead to what type of cancer?
answer
Liver cancer
question
Human T-cell lymphotrophic virus can lead to what type of cancer?
answer
Adult T-cell leukemia
question
Kaposi's sarcoma-associated herpes virus can lead to what type of cancer?
answer
Kaposi's sarcoma
question
Genomic structures of retroviruses
answer
1. There are two mechanisms for retroviruses to cause cancer - FAST OR SLOW tumor-forming 2. The genome of fast tumor-forming retrovirus contains an oncogene (onc)
question
Fast tumor-forming retrovirus
answer
Contains an oncogene; onc
question
Slow tumor-forming retrovirus
answer
Activation of the c-myc proto-oncogene by retroviral promoter and enhancer insertions
question
HPV can cause cervical cancer, how?
answer
Once inside the cells of their host, HPV synthesizes a protein designated E7 - an oncogene product. E7 binds and inactivates p53 which causes E2F to start promoter "on" and cell begins mitosis
question
Carry oncogenes
answer
Both DNA and RNA viruses
question
Carry tumor suppressor genes
answer
Neither DNA or RNA viruses
question
Carry oncogene as part of a normal viral genome
answer
Only DNA viruses
question
Carry oncogene that has normal function in viral cycle
answer
Only DNA viruses
question
How many mutations are needed for developing cancer?
answer
Incidence of human cancers increases markedly with age. Assuming the rate of mutation is roughly constant during a life-time, incidence of cancer would be independent of age if only one mutation is required for malignancy. Therefore, multiple mutations are required for cancer to form. We know that the mutation rate for DNA is quite constant in our life time. If only one mutation is needed for getting cancer, the cancer rate should be quite constant over time or getting a horizontal line on this graph. However, occurrence rates for all cancers get higher over age, indicating that multiple mutations are needed for getting cancer.
question
Kinetics of tumor appearance in female transgenic mice carrying transgenes driven by the mouse mammary tumor virus (MMTV) breast-specific promoter
answer
Explanation: Females were studied because the hormonal stimulation of pregnancy activates expression of the MMTV-driven oncogenes. "Cooperativity" of oncogenic mutations and synergistic effects of oncogenes. Oncogenes work together to accelerate oncogenic process. Conclusion: I showed Ras oncogene and Myc oncogene. If there is only one mutation, either Ras or Myc in mice, it takes much longer for mice to develop cancer. However, if mice start with two mutated genes, both myc and Ras, they develop cancer at a much faster rate - this phenomenon is called cooperativity of oncogenes. One mutation leads to faster second mutation. Once first and second mutations occurs, subsequent mutations occur at faster and faster pace
question
If therapies can be targeted against cancer stem cells, then the might be more effectively kill the cancer stem cells
answer
Because we did not know the existence of cancer stem cells before and our anticancer drugs or therapies were developed for targeting regular cancer cells, not cancer stem cells. Cancer stem cells are more resistant to these drugs or therapies. You can kill all the regular cancer cells, which is usually more than 90 to 95% of all cancer cells in a tumor nodule, and you will observe an initial shrinking of the tumor, only to witness the comeback of the tumor because cancer stem cells are resistant to the drug. If we target cancer stem cells, the efficacy of the drug should be higher
question
Most tumor suppressors are involved in . . .
answer
1. Cell cycle regulation 2. DNA repair 3. Apoptosis Several times more tumor suppressor genes are found mutated than proto-oncogenes
question
BRCA1 and BRCA2 are tumor suppressor genes involved in what type of familial cancer?
answer
Breast cancer
question
Most familial cancers are consequences of what type of gene mutations?
answer
Tumor suppressor genes