Surgery Final: group projects – Flashcards
Unlock all answers in this set
Unlock answersquestion
Coaxial Needle Biopsy: There are all types of needle biopsy units, but what is the basic premise for all of them?

answer
A large bore needle is used to get cells from the target tissue. (most clinics will use one type but the indications/contraindications and risks are the same) (from Dav's feedback)
question
What is the benefit of a coaxial bx needle compared to other modalities? (3)
answer
-extracts samples more effectively w/ less damage to sample -the inner stylet and external needle requires less force and allows for more accuracy -less pain (smaller needle but same sample size)
question
What are the 3 types of coaxial bx needle?
answer
Disposable, adjustable, and reusable
question
indications for use of coaxial bx needle (6 tissue sites and 1 indication)
answer
-bx of breast, kidney, liver, lung, prostate and thyroid -when you need multiple bxs from a site
question
what makes the coaxial needle so awesome? (5)
answer
-it has *echogenic markings* on the cannula for precise US placement/guidance -can take larger intact samples -needle tracts straighter, avoiding "drift" -The Coaxial Biopsy needle is quick and allows for easy penetration -Coaxial biopsy needle is easy, quick, and cost effective for outpatient
question
Contraindications for coaxial bx needle use (4)
answer
-coagulopathy, abn. prothrombin time, platelet function, bleeding time -uncooperative pt -thrombocytopenia -bleeding, bruising, infection, tumor at bx site (tumor... isn't that the whole point..? Maybe confirmed CA where you need to stick the needle into bx under it?)
question
complications from use of a coaxial bx needle (6 short term and 2 long term)
answer
*Short term*: gross bleeding, subQ bleeding, hematoma, hemo/pneumothorax, air embolism *Long term*: organ or vessel perforation
question
how do you use a coaxial needle bx?
answer
prep: sterile technique, cleanse area, stabilize nodule, inject anesthetic Bx: inster bx needle to level of mass and into the nodule, create suction on the syringe and briskly move needle back and forth w/ in the needle up to 10 times then release the suction/plunger -withdraw needle & apply firm pressure for 2 mins
question
Cost? (is this relevant?... idfk my bff Jill)
answer
$146.25 for a 5 pack $29.25 each
question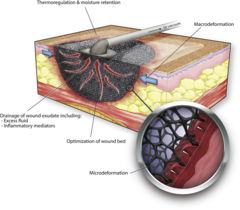
What is a wound vac?
answer
A negative pressure wound care system
question
What type of wounds should you use a wound vac on?
answer
acute, chronic, traumatic, subacute, and dehisced wounds, partial-thickness burns, ulcers, flaps and grafts
question
What are contraindications for use of a wound vac?
answer
Absolute contraindications for the use of a negative pressure wound therapy system include exposed vital structures, ongoing infection, devitalized tissue, malignant tissue, fragile skin, and adhesive allergies.
question
What should you do before using a wound vac on a wound?
answer
Debride devitalized tissue and treat infections
question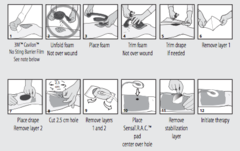
How is a wound vac used?
answer
The VAC system consists of a filler material that is placed into the wound, a drape that seals and insulates the wound, a tube that connects the wound to the fluid collection canister, and a vacuum. The negative-pressure system optimizes wound healing by creating a moist environment, increasing blood flow to the area and promoting the development of granulation tissue.
question
What are some complications of using a wound vac?
answer
Bleeding, especially in patients with blood vessel grafts, infections, and those who are on blood thinners. However, most complications resulted from dressings being left in the wound
question
How much does a wound vac cost?
answer
Market prices vary widely when any wound VAC system is ordered directly from the manufacturer ($457.17 -$3,600). However, the equipment is sometimes rented.
question
What is a catheter with two channels--one for injection and the other for removal of fluids.

answer
Double-Lumen Central Venous Catheter
question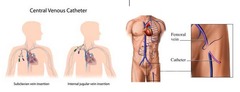
Where is the double-lumen central venous catheter inserted?
answer
Into a venous great vessels--subclavian/internal jugular/common femoral vein are most commonly used
question
Double-lumen central venous catheter indications (4)
answer
1. Inadequate peripheral venous access 2. Administration of noxious medications (e.g. vasopressors, chemotherapy or parenteral nutrition) that cannot be better tolerated when given in a peripheral IV catheter due to phlebitis 3. Hemodynamic monitoring (central venous access permits measurement of the central venous pressure, venous oxyhemoglobin saturation and cardiac parameters) 4. Extracorporeal therapies (e.g. hemodialysis, continuous renal replacement therapy and plasmapheresis)
question
Absolute Double-lumen central venous catheter contraindications (9)
answer
1. SVC syndrome 2. PTX/Hemothorax on contralateral side 3. Hypersensitivity to Chlorhexidine on contralateral side 4. Coagulopathies 5. Presence of newly inserted (4-6 weeks) pacemaker wire 6. Carotid disease 7. Diaphragmatic dysfunction 8. Thyromegaly 9. Previous neck surgery
question
Relative Double-lumen central venous catheter contraindications (5)
answer
1. Recent cannulation of the internal jugular vein 2. Skin infection over puncture site 3. Application of high positive end-expiratory pressure 4. Only one functioning lung 5. Burn scar on neck
question
Immediate complications of Double-lumen central venous catheter (7)
answer
1. Bleeding 2. Arterial puncture 3. Arrhythmia 4. Air embolism 5. Thoracic duct injury 6. Catheter malposition 7. PTX/hemothorax
question
Delayed complications of Double-lumen central venous catheter (6)
answer
1. Infection 2. Venous thrombosis 3. Pulmonary embolism 4. Catheter migration/embolism 5. Myocardial perforation 6. Nerve injury
question
How do you place a double-lumen central venous catheter? (9 steps)
answer
1. Place pt in a dependent position based on vein to be cannulated 2. Prep and drape the patient's (neck/shoulder/groin) in sterile fashion. 3. Anesthetize with 1% Lidocaine 4. Introduce the double lumen catheter using *Seldinger technique with U/S guidance* 5. Thread the catheter smoothly over the guide wire and obtain appropriate blood return. 6. Evacuate air from each lumen of the catheter and flush with sterile saline. 7. Suture catheter in place to the skin and apply sterile dressing 8. Check perfusion to the *extremity distal to the point of catheter insertion and confirm* that it is adequate. 9. A post procedure CXR typically done to confirm catheter position.
question
What is a BARD® DIGNISHIELD - Stool Management System?
answer
A series of devices that work together to ease the collection or disposal of fecal material in bed ridden patients as well as assist in medication administration
question
According to the National Institute for Health and Clinical Excellence, it is estimated that chronic fecal incontinence affects between _-__% of the adult population
answer
1; 10
question
What is the purpose of the BARD® DIGNISHIELD™ Stool Management System (SMS)?
answer
It was designed for managing fecal matter by re-routing and collecting liquid or semi-liquid stools to minimize skin contact in bedridden patients
question
What are contraindications to the BARD® DIGNISHIELD™ Stool Management System (SMS)?
answer
No patient should use this system for more than 29 days In addition, intra-anal devices should not be used in patients who have or had any of the following: sensitivity or allergies to components within the system, lower large bowel or rectal surgery in the last year, rectal or anal injury, severe rectal or anal stricture or stenosis, confirmed rectal or anal tumor, severe hemorrhoids, or fecal impaction, suspected or confirmed rectal mucosa impairment, indwelling rectal or anal devices, delivery mechanisms, or enemas in place
question
How do you use the Stool Management System?
answer
Attach the bag and deflate the cuff Next, position the patient on their left side (with knees bent) and perform a Digital Rectal Exam (DRE) to test for immediate contraindications and assess for tone Fold the cuff into a conical shape and apply lube generously prior to inserting the cuff into the anal sphincter Once in the rectal vault, the cuff will open and can be inflated with 45 mL of tap water Finally, gently pull on the catheter to be sure that the cuff is sitting on the rectal floor
question
How often should the device be checked for waste disposal and to ensure the system is working properly?
answer
Daily
question
What are the most common complications of the Stool Management System?
answer
Pressure ulcers from the tubing, loss of sphincteral tone, fecal impaction, rectal bleeding, and mucosal erosion
question
Skin should also be assessed daily for the presence of _________ ______ that could be occurring
answer
decubitus ulcers
question
The complication rate for longer duration use of more than __ days was significantly higher than in those who used the device for a shorter duration
answer
17
question
Many companies have wide price ranges for this system, however, we've found that the price of the Dignishield Stool Management System can range from ~$___ to ~$____ per case
answer
800; 2000 (each case contains 2 complete stool maintenance systems)
question
Unfortunately, rampant iatrogenic _ _________ has made this equipment standard in hospitals (from feedback)
answer
C. difficile
question
What is a PTA/PTCA Dilatation Catheter?
answer
A double lumen catheter with a balloon near its distal tip. One lumen is for the guide wire while the other lumen is for expansion of the balloon.
question
What are the indications for a PTA/PTCA Dilatation Catheter?
answer
1. Percutaneous transluminal angioplasty (PTA) of lesions (often atherosclerotic plaque) within peripheral arteries including renal, iliac, popliteal, infrapopliteal, femoral and iliofemoral as well as obstructive lesions of native or synthetic arteriovenous dialysis fistulae. -"PTCA" is essentially the same except for coronary vessels. 2. For post dilatation of balloon-expandable peripheral vascular stents.
question
What are the Relative contraindications for a PTA/PTCA Dilatation Catheter?
answer
1. severe uncontrolled hypertension 2. ventricular arrhythmias 3. acute stroke 4. severe anemia 5. active GI bleeding 6. allergy to radiographic contrast 7. acute renal failure 8. uncompensated heart failure 9. unexplained febrile illness/untreated active infections 10. electrolyte abnormalities 11. severe coagulopathy (No absolute CIs)
question
How are PTA/PTCA Dilatation Catheters used?
answer
1. insert a large, hollow needle into the vessel of choice (often femoral artery) through which a guide wire is introduced into the vessel 2. needle is then removed leaving the guide wire in place 3. A 5 or 6 French sheath is placed over the guide wire and inserted into the vessel 4. guide wire is removed leaving catheter in place 5. Using fluoroscopy guidance, the balloon is advanced to the lesion site and placement is confirmed using distal and proximal radiopaque balloon markers 6. a syringe attached to the "BALLOON" lumen is used to inject a mixture of contrast and normal saline until the desired amount balloon inflation is achieved 7. The balloon forces expansion of the stenotic lesion within the vessel and surrounding muscular wall opening it up for improved flow. Finally, the balloon is deflated and withdrawn.
question
What are the potential complications for PTA/PTCA Dilatation Catheters?
answer
1. air embolism 2. aneurysm, arrhythmias 3. AV fistula 4. reactions to contrast medium 5. hemorrhage or hematoma 6. hypo/hypertension 7. systemic embolization 8. vascular thrombosis 9. local infection 10. bacteremia 11. death 12. (in addition with PTCA) MI, CVA, hemodynamic complications, and perforation of heart chamber(s)
question
Cost of PTA/PTCA Dilatation Catheters?
answer
Apprx. $5.00 per catheter
question
What is a ureteral stent?
answer
a porous, hollow tube with curled "pigtail" like ends to prevent migration after insertion. The distal tail of the stent contains a string allowing for removal without cystoscopy
question
What materials may be used to make a ureteral stent?
answer
Stents come in a variety of materials, coatings, shapes and sizes. Silicone-based stents are flexible, but sometimes difficult to push and are subject to collapse. Metal stents are used to relieve ureteral obstruction, where force may be required to maintain patency. Additionally, coatings such as hydrogel, silver nitrate, heparin, and ofloxacin are aimed at improving function, tolerance and reducing complications.
question
Indications of Ureteral Stents (2)
answer
-Ureteral obstruction (which can be due to nephrolithiasis, tumor, or retroperitoneal fibrosis) -Conjuctional use with other therapies
question
What is the function of an ureteral stent?
answer
Reestablish or maintain the patency of the ureter
question
Contraindications of Ureteral Stents (6)
answer
-Active UTI with the prescence of increased WBC count, fever, chills -Diagnosis of two acute UTIs within 12 months, along with increased WBC count, chills, and fever -Individuals with hematuria that has not been evaluated or treated prior to insertion -Individuals who cannot receive antibiotic treatment -Iodine allergies -Individuals who have a history of illness, meds, or surgery that could effect the efficacy of the stent
question
What else is needed (in addition to the ureteral stent set) in performance of the procedure?
answer
Cystoscope
question
Explain the procedure.
answer
The provider will use the cystoscope to insert the guidewire through the ureter and into the renal pelvis. The stent must be wet to activate the coating, which prevents crusting, and it should be passed over the guidewire through the cystoscope. A positioner is used to advance the stent into the ureter until its end is located at the ureteral orifice. Once the stent is in place, the provider will cut one of the suture strands attached to the stent and gently pull on the suture to remove. The guidewire and positioner can then be removed. At this point, ureter patency should be established.
question
Complications of ureteral stents (10)
answer
-Ureteral reflux -Stent occlusion -Stent dislodgment -Bacterial infection -Peritonitis -Sepsis -Extravasation -Hemorrhage -Perforation of the kidney, renal pelvis, ureter, and/or bladder -Patient could experience incontinence, hematuria, and suprapubic pain
question
Pricing of the ureteral stent
answer
Varies largely Anywhere from $49-$115 Other manufacturers have stents for around $150
question
Dav's definition of what a ureteral stent does
answer
Based upon the same principle as cardiac stents, ureteral stents are designed to be inserted through a cystoscope and re-establish patency for drainage through a variety of obstructions. These devices must be placed in a relatively sterile environment, all bacterial activity within the renal system must be controlled before placement.
question
-Instrument that can *simultaneously cut & staple tissue during laparoscopic sgx.* -intended for transection, resection, and creation of anastomoses of various body tissue (i.e. liver, spleen, stomach)
answer
Endoscopic Linear Cutters
question
What is a PleurX Catheter System?
answer
Allows patients to manage symptoms of malignant ascites and pleural effusions by making it possible to drain excess fluid at home or in a care facility
question
What are the indications for a PleurX Catheter System?
answer
Management of recurrent pleural effusions and malignant ascites
question
What are the contraindications to a PleurX Cath system?
answer
1.Cannot provide adequate symptomatic relief in multi-loculated ascites 2. non-correctable coagulopathy 3. infected peritoneal cavity
question
How is the PleurX Cath system used?
answer
Similar to traditional paracentesis or thracentesis with major difference being suture at the incision site encircling and stabilizing the catheter in place. -drainage line attached -suction unit attached -when suction completed, occlude suction, lock catheter valve, remove adapter from drainage line. Clean with alcohol pad when done
question
complications of PleurX cath system?
answer
Short-term for palliative treament of malignant ascites: electrolyte imbalance, proetin depletion, ascites leakage, peritonitis, further loculations peritoneal cavity. Short-term complications for pleural effusions: oneumothorax, re-ex-pansion pulmonary edema, hypotension, circulatory collapse. Long-term: infection.
question
cost of PleurX cath system?
answer
$885.60 lets be honest, neither you or I really give a f**k about the cost :) or anything else in this class.
question
Dav's side notes about the PleurX Cath System?
answer
Amount of fluid removed should be limited to 1000cc from the chest or 2000cc from the abdomen at one time--> prevents circulatory collapse, re-expanion pulmonary edema, electrlyte impabance and protein depletion.



