Step 1 First Aid – Biochemistry Mock Board – Flashcards
Unlock all answers in this set
Unlock answersquestion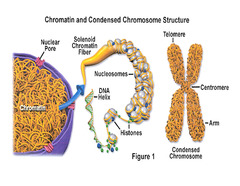
Chromatin structure
answer
Negatively charged DNA loops twice around histone octamer (2 each of the positively charged H2A, H2B, H3, and H4) to form nucleosome bead. H1 ties nucleosomes together in a string. (Think of "beads on a string"; H1 is the only histone that is not in the nucleosome core.) In mitosis, DNA condenses to form mitotic chromosomes.
question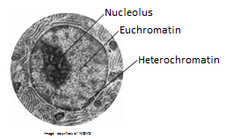
Heterochromatin
answer
Condensed, transcriptionally inactive ("H eteroC hromatin = H ighly C ondensed.")
question
Euchromatin
answer
Less condensed, transcriptionally active (Eu = true, "truly transcribed")
question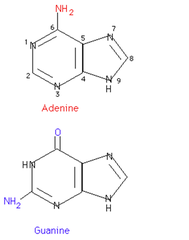
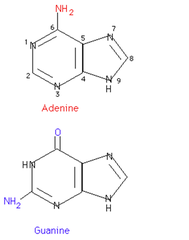
Purines
answer
A, G 2 Rings ("PUR e A s G old = PUR ines")
question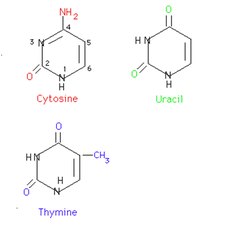
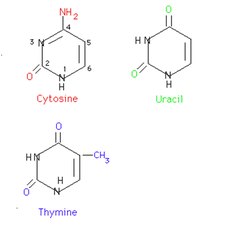
Pyrimidines
answer
C, T, U 1 ring ("CUT the PY (pie): PY rimidines")
question
Functional groups of the nucleosides
answer
Guanine has a ketone. Thy mine has a methy l. Deamination of cytosine makes uracil.
question
Base differences btw RNA and DNA
answer
Uracil is found in RNA; Thymine in DNA
question
Base pair bonds
answer
G-C bond (3 H-bonds) is stronger than A-T bond (2 H-bonds). Incr G-C content --< higher melting temperature.
question
AA's necessary for purine synthesis
answer
Glycine Aspartate Glutamine
question
Nucleoside
answer
Base + ribose
question
Nucleotide
answer
Base + ribose + phosphate; linked by 3'-5' phosphodiester bond.
question
Purines are made from...?
answer
IMP precursor
question
Pyrimidines are made from...?
answer
Orotate precursor, with PRPP added later.
question
Deoxyribonucleotide synthesis

answer
Ribonucleotides are synthesized first and are converted to deoxyribonucleotides by ribonucleotide reductase.
question
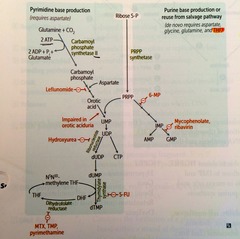
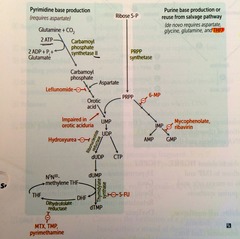
ABX and anti-neoplastic drugs that function by interfering w/ nucleotide synthesis (list)
answer
Hydroxyurea 6-mercaptopurine 5-fluorouracil Methotrexate Trimethoprim
question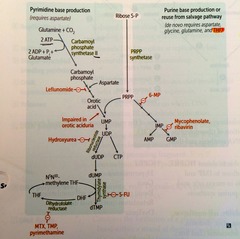
*Hydroxyurea*
answer
Inhibits ribonucleotide reductase.
question
*6-mercaptopurine (6-MP)*
answer
Blocks de novo purine synthesis.
question
*5-Fluorouracil (5-FU)*
answer
Inhibits thymidilate synthase (decr dTMP).
question
*Methotrexate*
answer
Inhibits dihydrofolate reductase (decr dTMP)
question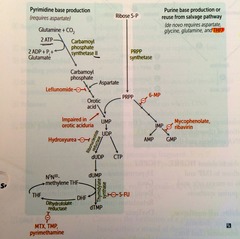
*Trimethoprim*
answer
Inhibits bacterial dihydrofolate reductase
question
Genetic code: unambiguous
answer
Each codon specifies only 1 AA.
question
Genetic code: degenerate/redundant
answer
; 1 codon may code for the same AA. (Methionine is encoded by 1 codon: AUG)
question
Genetic code: Commaless, nonoverlapping
answer
Read from a fixed starting point as a continuous sequence of bases. *some viruses are an exception.
question
Genetic code: universal
answer
Genetic code is conserved throughout evolution. *exceptions include mitochondria, archaebacteria, Mycoplasma , and some yeasts
question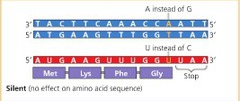
Silent mutation
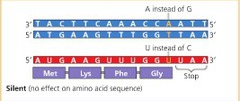
answer
Same AA, often base change in 3rd position of codon (tRNA wobble)
question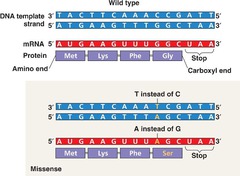
Missense mutation
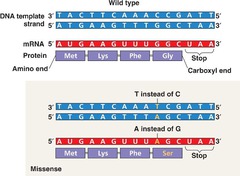
answer
Changed AA (conservative -- new AA is similar in chemical structure)
question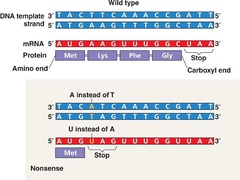
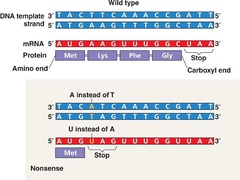
Nonsense mutation
answer
Change resulting in early stop codon ("Stop the nonsense !")
question
Frame shift mutation
answer
Change resulting in misreading of all nucleotides downstream, usually resulting in a truncated, nonfunctional protein.
question
Severity of damage in DNA mutations
answer
1. Nonsense 2. missense 3. silent
question
What direction is DNA/RNA made?
answer
They are both synthesized in the 5'--<3' direction. Remember that the 5' of the incoming nucleotide bears the triphosphate (energy source for bond). The 3' hydroxyl of the nascent chain is the target.
question
What direction is mRNA read?
answer
5'--<3'.
question
What direction is protein synthesized?
answer
N--<C
question
3 Types of mRNA
answer
rRNA is the most abundant mRNA is the longest tRNA is the smalles ("R ampant, M assive, T iny")
question
mRNA start codon
answer
AUG (or rarely GUG) ("AUG inAUG urates protein synthesis") In eukartyotes, codes for methionine, which may be removed before translation is completed. In prokaryotes, codes for formyl-methionine (f-Met).
question
mRNA stop codons
answer
UGA, UAA, UAG UGA = U G o A way UAA = U A re A way UAG = U A re G one
question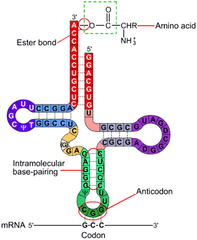
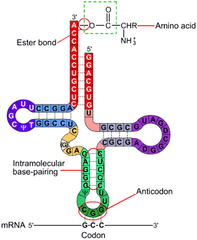
tRNA structure
answer
secondary structure, cloverleaf form, anticodon end is opposite 3' aminoacyl end. All tRNAs, both eukaryotic and prokaryotic, have CCA at 3' end along w/ a high percentage of chemically modified bases. The AA is covalently bound to the *3'* end of tRNA. *CCA* *c*an *c*arry *a*mino acids
question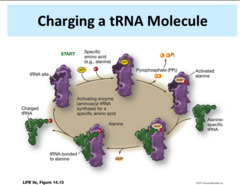
Charging of tRNA
answer
Aminoacyl-tRNA synthetase (1 per AA, "matchmaker," uses ATP) scrutinizes AA before and after it binds to tRNA. If incorrect, bond is hydrolyzed. The aa-tRNA bond has energy for formation of peptide bond. A *mischarged tRNA reads usual codon but inserts wrong AA.*
question
What is responsible for the accuracy of AA selection?
answer
Aminoacyl-tRNA synthetase AND binding of charged tRNA to the codon
question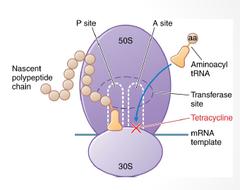
Mechanism of *tetracyclines*
answer
Bind 30S subunit, preventing the attachment of aminoacyl-tRNA.
question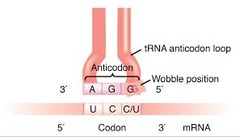
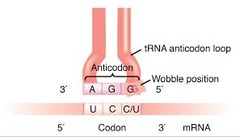
tRNA wobble
answer
Accurate base pairing is required only in the first 2 nucleotide positions of an mRNA codon, so codons differing in the 3rd "wobble" position may code for the same tRNA/aa (due to degeneracy of genetic code).
question
Protein synthesis: *Initiation*
answer
Activated by *GTP hydrolysis*, initiation factors (eIFs) help assemble the 40S ribosomal subunit w/ the initiator tRNA released when the mRNA and the ribosomal subunit assemble w/ the complex. *E*ukaryotes: 40S + 60S = 80S (*Even*) Pr*O*karyotes: 30S + 50S = 70S (*Odd*)
question
Protein synthesis: *Step 1 in Elongation*

answer
*Aminoacyl-tRNA* binds to *A site* (except for initiator methionine)
question
Protein synthesis: *Step 2 in Elongation*
answer
*Peptidyltransferase* catalyzes *peptide bond formation*, transfers growing polypeptide to amino acid in A site.
question
Protein synthesis: *Step 3 in Elongation*
answer
Ribosome advances 3 nucleotides toward the 3' end of RNA, moving *peptidyl RNA to P site* (*translocation*)
question
*Mnemonic* for the *3 sites* in the ribosome (translation)
answer
"going *APE* " *A* site = incoming *A*minoacyl tRNA *P* site = accommodates growing *P*eptide *E* site = holds *E*mpty tRNA as it Exits
question
Protein synthesis: *Termination*

answer
-Stop codon recognized by release factor -Completed protein is released from ribosome thru simple hydrolysis and dissociates.
question
*Aminoglycosides* as protein synthesis inhibitors

answer
Inhibit formation of the initiation complex *30s* and cause misreading of mRNA.
question
*Chloramphenicol* as a protein synthesis inhibitor
answer
Inhibits *50S peptidyltransferase*.
question
*Macrolides* as protein synthesis inhibitors
answer
Bind *50S*, *blocking translocation*
question
*Clindamycin* as a protein synthesis inhibitor
answer
Binds *50S*, blocking translocation.
question
Energy requirements of translation
answer
tRNA aminoacylation: ATP --< AMP (2 phosphoanhydride bonds) Loading tRNA onto ribosome: GTP --< GDP Translocation: GTP --< GDP Total energy expenditure = 4 high-energy phosphoanhydride bonds
question
Posttranslational modifications: *Trimming*
answer
*Removal of N- or C-terminal propeptides* from zymogens to generate mature proteins.
question
Posttranslational modifications: *Covalent Alterations*
answer
Phosphorylation, glycosylation, and hydroxylation.
question
Posttranslational modifications: *Proteasomal Degradation*
answer
*Attachment of ubiquitin* to defective proteins to tag them for breakdown.
question
Enzyme regulation methods
answer
Enzyme concentration alteration (synthesis and/or destruction) Covalent modification (e.g., phosphorylation Proteolytic modification (zymogen) Allosteric regulation (e.g., feedback inhibition) pH Temperature Transcriptional regulation (e.g., steroid hormones)
question
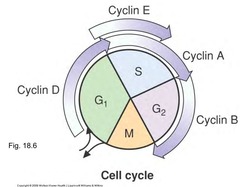
Order (and important lengths) of *cell cycle phases*
answer
Mitotis (shortest phase): prophase - metaphase - anaphase - telophase. G1 and G0 are of variable duration.
question
Cell Cycle *Regulation*
answer
CDK Cyclin Tumor Suppressors
question
*CDKs*

answer
Cyclin-dependent kinases; constitutive and inactive.
question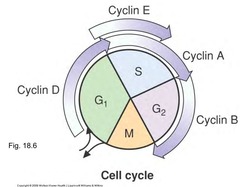
*Cyclins*
answer
Regulatory proteins that control cell cycle events; phase specific; *activate CDKs*
question
Cyclin-CDK complexes

answer
Must both be activated and inactivated for cell cycle to progress.
question
Tumor suppressors (and the cell cycle)

answer
*Rb and p53 normally inhibit G1-to-S progression*; mutations in these genes result in unrestrained cell growth.
question
Cell Types: *Permanent cells*
answer
Remain in *G0*, regenerate from stem cells. (e.g., neurons, skeletal and cardiac muscle, RBCs)
question
Cell Types: *Stable (quiescent) cells*
answer
Enter *G1 from G0* when stimulated (e.g., Hepatocytes, lymphocytes)
question
Cell Types: *Labile cells*
answer
*Never go to G0*, divide rapidly w/ a *short G1* (e.g., Bone marrow, gut epithelium, skin, hair follicles)
question
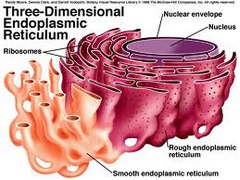
*Rough Endoplasmic Reticulum (RER)*
answer
Site of synthesis of secretory (exported) proteins and of N-linked oligosaccharide addition to many proteins. (Goblet cells are abundant with RER)
question
*Nissl bodies*

answer
RER in *neurons* -- synthesize enzymes (e.g., ChAT) and peptide neurotransmitters.
question
*Free ribosomes*
answer
unattached to any membrane; site of synthesis of cytosolic and organellar proteins.
question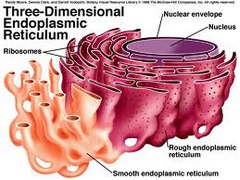
Smooth endoplasmic reticulum (SER)
answer
Site of *steroid synthesis* and *detoxification* of drugs and poisons.
question
2 important examples of *cells rich in SER*
answer
1. Liver hepatocytes 2. Steroid hormone-producing cells of the adrenal cortex
question
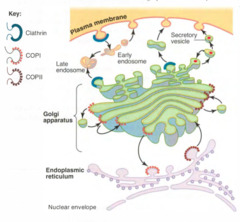
Golgi apparatus: distribution center of ____ from ___ to ____?
answer
proteins and lipids __*from*__ER__*to*__ the plasma membrane, lysosomes, and secretory vesicles .
question
Golgi apparatus: modifies *N-oligosaccharides* on ____?
answer
Asparagine
question
Golgi apparatus: adds *O-oligosaccharides* on ____?
answer
Serine and threonine.
question
Golgi apparatus: adds *mannose-6-phosphate* to ____? What does this do?
answer
Specific *lysosomal proteins* --< targets protein to the lysosome.
question
Golgi apparatus: assembles ___ from ____?
answer
Assembles *proteoglycans* from *core proteins*
question
Golgi apparatus: sulfation of ____ and ____?
answer
sulfation of *sugars in proteoglycans* and *selected tyrosine* on proteins .
question
Vesicular trafficking proteins: *COPI*
answer
*Retrograde*: cis-Golgi --< ER
question
Vesicular trafficking proteins: *COPII*

answer
*Anterograde*: RER --< cis-Golgi
question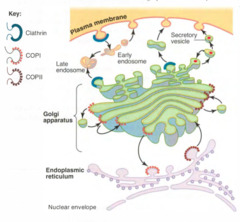
Vesicular trafficking proteins: *Clathrin*
answer
*Receptor-Mediated Endocytosis*: trans-Golgi --< lysosomes, plasma membrane --< endosomoes Example: LDL receptor
question
*I-cell disease* (inclusion cell dz): genetic/molecular *basis*?
answer
Inherited *lysosomal storage disease*; failure of addition of *mannose-6-phosphate* to lysosome proteins (enzymes are secreted outside the cell instead of being targeted to the lysosome).
question
*I-cell dz* (inclusion cell dz): *Results*?
answer
Coarse facial features, clouded corneas, restricted joint mvmt, and high plasma levels of lysosomal enzymes. Often fatal in childhood.
question
Microtubules

answer
Cylindrical structure composed of a helical array of polymerized *dimers of alpha- and beta-tubulin* Each dimer has *2 GTP bound* Incorporated into *flagella, cilia, mitotic spindles*. Grows slowly, collapses quickly. Also involved in *slow axoplasmic transport in neurons*
question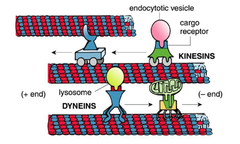
Molecular motor activity of Microtubules
answer
Transport cellular cargo twd opposite ends of MT tracks. 1. *Dynein* = retrograde to microtubule (+ --< -) 2. *Kinesin* = anterograde to MT (- ---< +)
question
*Drugs* that act on microtubules
answer
1.) Mebendazole/thiabendazole (antihelminthic) 2.) Griseofulvin (antifungal) 3.) Vincristine/vinblastine (anti-cancer) 4.) Paclitaxel (anti-breast cancer) 5.) Colchicine (anti-gout)
question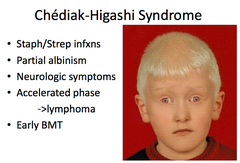
*Chédiak-Higashi syndrome*
answer
Microtubule polymerization defect resulting in *decreased phagocytosis*. Results in *recurrent pyogenic infections, partial albinism, and peripheral neuropathy*
question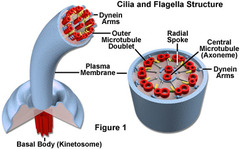
*Cilia* structure
answer
*9 + 2* arrangement of *MT*'s.
question
Axonemal *dynein*
answer
*ATPase* that links *peripheral 9 doublets* and causes *bending* of cilium by differential sliding of doublets.
question
*Kartagener's syndrome*
answer
*Immotile cilia* due to a *dynein arm defect*. Results in male and female *infertility* (sperm immotile), *bronchiectasis*, and *recurrent sinusitis* (bacteria and particles not pushed out); associated w/ situs inversus.
question
*Actin and myosin*

answer
1. *Microvilli* 2. Muscle contraction 3. Cytokinesis 4. Adherens jxn
question
Microtubules (what *structures* are they found in?)
answer
Cilia Flagella Mitotic spindle Neurons Centrioles
question
*Intermediate filaments*
answer
Vimentin Desmin Cytokeratin Glial fibrillary acid proteins (GFAP) Neurofilaments
question
Plasma membrane *composition*
answer
Asymmetric bilayer. Contains XOL (~50%), phospholipid (~50%), sphingolipids, glycolipids, and proteins. High XOL or long saturated FA content --< incr melting temp, decr fluidity.
question
Western blot.
answer
Sample protein is separated via *gel electrophoresis* and transferred to a filter. *Labeled Ab is used to bind to relevant protein*
question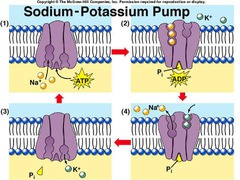
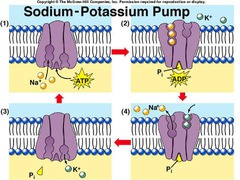
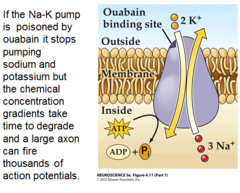
Sodium pump
answer
Na+/K+ ATPase is located in the plasma membrane w/ *ATP site on cytoplasmic side* For each ATP consumed, 3 Na+ go out and 2 K+ come in. During cycle, pump is phosphorylated.
question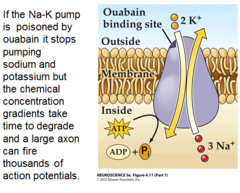
*Ouabain*
answer
Inhibits sodium pump (Na+/K+) by *binding the K+ site.*
question
*Cardiac glycosides (digoxin and digitoxin)*
answer
*Directly inhibit Na+/K+ ATPase*, which leads to indirect *inhibition of Na+/Ca2+ exchange*. *Incr Ca2+* --< incr cardiac contractility.
question
Collagen (generally)
answer
Most abundant protein in the human body. Extensively modified. Organizes and strengthens extracellular matrix.
question
*Type I collagen* Where is this type of collagen found?
answer
90% Bone, skin, tendon, dentin, fascia, CORNEA, late wound repair *Type I = bONE*
question
*Type II collagen* Where is this type of collagen found?
answer
Cartilage (including hyaline), VITREOUS HUMOR, nucleous pulposus. *Type II = carTWOlage*
question
*Type III collagen* Where is this type of collagen found?
answer
(*Reticulin*) Skin, blood vessels, uterus, fetal tissue, granulation tissue
question
*Type IV collagen* Where is this type of collagen found?
answer
Basement membrane or basal lamina *Type IV = Under the floor (basement membrane)*
question
Collagen *Synthesis*

answer
Involves: Synthesis in RER Hydroxylation of Proline and Lysine Glycosylation of lysine of procollagen chain Exocytosis Procollagen-->Tropocollagen Cross-linking of tropocollagen by covalent lysine-hydroxylysine bonds
question
*Ehlers-Danlos syndrome*: what is it basically? what are the signs/sx?
answer
*Type III collagen is most frequently affected.* Faulty collagen synthesis in *cross linking in ECM* of lysine-OHlysine causing: 1.) Hyperextensible skin 2.) Tendency to bleed (easy bruising) 3.) Hypermobile joints
question
*Osteogenesis imperfecta* (generally)
answer
Genetic bone d/o (brittle bone dz) *Problems forming triple helix - procollagen in RER* 1.) Multiple fractures w/ minimal trauma; may occur during the birthing process. 2.) Blue sclera due to the translucency of the connective tissue over the choroid. 3.) Hearing loss (abnormal middle ear bones) 4.) Dental imperfections due to lack of dentin
question
Osteogenesis imperfecta: most common form
answer
autosomal dominant, abnormal *type I collagen*
question
Type II osteogenesis imperfecta
answer
Fatal in utero or neonatal period.
question
*Alport's syndrome* Due to....? Most common form...?
answer
*abnormal type IV collagen* (type IV collage is an imp. component of the basement membrane of the kidney, ears, and eyes) Most common form is X-linked recessive.
question
*Scurvy*
answer
- Deficiency in *vitamin C* resulting in defected collagen synthesis - No *hydroxylation of Proline and Lysine in RER*
question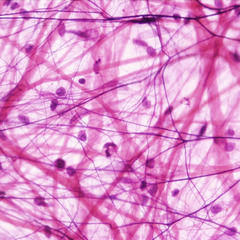
Elastin
answer
Stretchy protein w/in lungs, large arteries, elastic ligaments, vocal cords, ligamenta flava (connect vertebrae --< relaxed and stretched conformations) Rich in proline and glycine, nonglycosylated forms. Tropoelastin w/ fibrillin scaffolding. Broken down by elastase, which is normally inhibited by alpha1-antitrypsin.
question
Marfan's syndrome (cause)
answer
Caused by a *defect in fibrillin*
question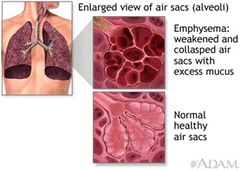
*Emphysema* (one cause)
answer
Can be caused by *alpha1-antitrypsin deficiency*, resulting in *excess elastase activity*.
question
*Fat-soluble* Vitamins (list + their basic fxns)
answer
*Vitamin A* - vision *Vitamin D* - bone calcification, Ca2+ homeostasis Vitamin E - antioxidant *Vitamin K* - clotting factors *Vitamin E*
question
*Fat-soluble* vitamins: absorption?
answer
(A, D, E, K) Absorption dependent on gut (*ileum*) and pancreas. Malabsorption syndromes (*steatorrhea*), such as cystic fibrosis and sprue, or mineral oil intake can cause fat-soluble vitamin deficiencies.
question
*Water-soluble* vitamins (list and basic fxns)
answer
*Vitamin C* - antioxidant, collagen synthesis *Vitamin B's*: *Thiamine (B1) Riboflavin (B2) Niacin (B3) Pantothenic acid (B5) Pyridoxine (B6) Biotin (B7)* *Folate* - blood, neural development *Cobalamin (B12)* - blood, CNS
question
Water-soluble vitamins: list with alternative names and related enzymes/cofactors?
answer
B1 (thiamine: TPP) B2 (riboflavin: FAD, FMN) B3 (niacin: NAD+) B5 (pantothenic acid: CoA) B6 (pyridoxine: PLP) B12 (cobalamin) C (ascorbic acid) Also: Biotin, folate
question
Water soluble vitamin *deficiencies*
answer
All wash out easily from body *except B12 and folate* (stored in liver). *B-complex deficiencies* often result in dermatitis, glossitis, and diarrhea.
question
*Vitamin A (retinol)*: fxn? use? where is it found?
answer
Antioxidant; constituent of visual pigments (retinal). Retinol is vitamin A , so think Retin-A (used topically for wrinkles and acne). Found in liver and leafy vegetables.
question
Vitamin A (retinol) *deficiency?*
answer
-Night blindness, - dry skin
question
Vitamin A (retinol) *excess?*
answer
Arthralgias, fatigue, HAs, skin changes, sore throat, alopecia. Teratogenic (cleft palate, cardiac abnormalities).
question
*Vitamin B1 (thiamine):* fxn?
answer
In thiamine pyrophosphate (*TPP*), a cofactor for several enzymes: 1.) Pyruvate dehydrogenase (*glycoslysis*) 2.) alpha-ketoglutarate dehydrogenase (*TCA cycle*) 3.) Transketolase (*HMP shunt*) 4.) Branched-chain AA dehydrogenase (*AA metabolism*)
question
Vitamin B1 (thiamine) *deficiency*: causes what? Where do you see this?
answer
*Wernicke-Korsakoff syndrome* and *beriberi* (both neurologic and cardiac manifestations). Seen in malnutrition as well as *alcoholism* (secondary to malnutrition and malabsorption).
question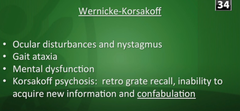
*Wernicke-Korsakoff syndrome*
answer
Due to *Vitamin B1 (thiamine)* deficiency. confusion, ophthalmoplegia, ataxia + memory loss, confabulation, personality change.
question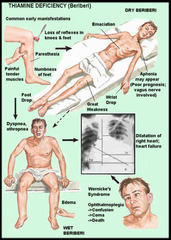
*Beri-beri*
answer
Due to Vitamin B1 (thiamine) deficiency. (spell it *B er1-B er1* ) 1. *Dry* beriberi - polyneuritis, symmetrical muscle wasting. 2. *Wet* beriberi - high-output cardiac failure (dilated cardiomyopathy), edema.
question
*Vitamin B2* (riboflavin) fxn?
answer
*Cofactor* in oxidation and reduction (e.g., FADH2) *FAD and FMN* are derived from *riboflavin* (*B2 = 2 ATP*)
question
Vitamin B2 (riboflavin) *deficiency*?
answer
Cheilosis (inflammation of lips, scaling and fissures at corners of mouth), Corneal vascularization. "*The 2 C 's*"
question
*Vitamin B3 (niacin)* fxn?
answer
Constituent of *NAD+, NADP*+ (used in redox rxtns). Derived from *tryptophan*. Synthesis *requires vitamin B6*. *NAD derived from Niacin (B3 = 3 ATP)*
question
Vitamin B3 (niacin) *deficiency*?
answer
Glossitis. Severe deficiency leads to pellagra, which can be caused by Hartnup dz (decr tryptophan absorption), malignant carcinoid syndrome (incr tryptophan metabolism), and INH (decr vitamin B6) *The 3 D's of pellagra: D iarrhea, D ermatitis, D ementia.*
question
Vitamin B3 (niacin) *excess*?
answer
Facial flushing (due to pharmacologic doses for Tx of hyperlipidemia)
question
*Vitamin B5 (pantothenate)* deficiency?
answer
Dermatitis, enteritis, alopecia, adrenal insufficiency
question
*Vitamin B6 (pyridoxine)* fxn?
answer
Converted to pyridoxal phosphate, a *cofactor used in transamination* (e.g., ALT and AST), decarboxylation rxtns, glycogen phosphorylase, and heme synthesis. Required for the synthesis of niacin from tryptophan.
question
Vitamin B6 (pyridoxine) *deficiency*?
answer
Convulsions, hyperirritability, peripheral neuropathy (deficiency inducible by INH and oral contraceptives)
question
*B12 (cobalamin)*: fxn?
answer
*Cofactor for homocysteine methyltransferase* (transfers CH3 groups as methylcobalamin) and methylmalonyl-CoA mutase.
question
B12 (cobalamin): *Deficiency*?
answer
*Macrocytic, megaloblastic anemia*; neurologic Sx (paresthesias, subacute combined degeneration) due to abnormal myelin. Prolonged deficiency leads to irreversible nervous system damage.
question
B12 (cobalamin): *found* where?
answer
Found in animal products. *Only synthesized by microorganisms*.
question
B12 (cobalamin): *etiology of deficiency*?
answer
Very large reserve pool (several yrs) stored primarily in liver. Deficiency is usually caused by malabsorption (sprue, enteritis, Diphyllobothrium latum ), lack of intrinsic factor (pernicious anemia, gastric bypass surgery), or absence of terminal ileum (Crohn's dz).
question
*Folic acid:* fxn?
answer
Converted to tetrahydrofolate (THF), a coenzyme for 1-carbon transfer/methylation rxtns. Important for the synthesis of nitrogenous bases in DNA and RNA.
question
Folic acid: deficiency?
answer
Macrocytic, megaloblastic anemia; no neurologic Sx (as opposed to vitamin B12 deficiency). Most common vitamin deficiency in the USA. Seen in alcoholism and pregnancy.
question
Folic acid: where is it found?
answer
FOL ate is from FOL iage (green leaves)
question
Etiology of folic acid deficiency?
answer
Small reserve pool stored primarily in liver (eat green leaves!) Deficiency can be caused by several drugs (e.g., phenytoin, sulfonamides, MTX).
question
Folic acid and pregnancy
answer
Supplemental folic acid in early pregnancy reduces neural tube defects.
question
S-adenosyl-methionine (SAM): formation?
answer
ATP + methionine --< SAM
question
S-adenosyl-methionine (SAM): fxn?
answer
SAM transfers methyl units. Regeneration of methionine (and thus SAM) is dependent on vitamin B12 and folate. ("SAM the methyl donor man")
question
Biotin: fxn?
answer
Cofactor for carboxylation enzymes: 1.) Pyruvate carboxylase : Pyruvate --< oxaloacetate 2.) Acetyl-CoA carboxylase : Acetyl-CoA --< malonyl-CoA 3.) Propionyl-CoA carboxylase : Propionyl-CoA --< methylmalonyl-CoA
question
Biotin: deficiency?
answer
Relatively rare. Dermatitis, alopecia, enteritis. Caused by ABX use or excessive ingestion of raw eggs. "AVID in in egg whites AVID ly binds biotin."
question
Vitamin C (ascorbic acid): fxn?
answer
Antioxidant. Also: 1.) Facilitates iron absorption by keeping iron in Fe2+ state (more absorbable) 2.) Necessary for hydroxylation of proline and lysine in collagen synthesis. 3.) Necessary for dopamine Beta-hydroxylase, which converts dopamine to NE
question
Vitamin C (ascorbic acid): deficiency?
answer
Scurvy: swollen gums, bruising, anemia, poor wound healing.
question
Vitamin C (ascorbic acid): where is it found?
answer
Found in fruits and vegetables. British sailors carried limes to prevent scurvy (thus the origin of the word "limey")
question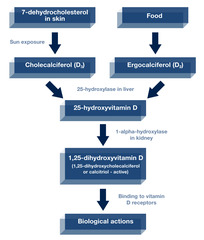
Vitamin D: forms?
answer
D2 = ergocalciferol -- ingested from plants, used as pharmacologic agent. D3 = cholecalciferol -- consumed in milk, formed in sun-exposed skin. 25-OH D3 = storage form. 1,25-(OH)2-D3 (calcitriol) = active form
question
Vitamin D: fxn?
answer
Incr intestinal absorption of calcium and phosphate, incr bone resorption
question
Vitamin D: deficiency?
answer
Rickts in children (bending bones), osteomalacia in adults (soft bones), hypocalcemic tetany. Drinking milk (fortified w/ vitamin D) is good for bones.
question
Vitamin D: excess?
answer
Hypercalcemia, hypercalciuria, loss of appetite, stupor. Seen in sarcoidosis (incr activation of vitamin D by epithelioid macrophages)
question
Vitamin E: fxn?
answer
Antioxidant (protects erythrocytes and membranes from free-radical damage). "E is for E rythrocytes"
question
Vitamin E: deficiency?
answer
Incr fragility of erythrocytes (hemolytic anemia), muscle weakness, neurodysfxn.
question
Vitamin K: fxn?
answer
Catalyzes gamma-carboxylation of glutamic acid residues on various proteins concerned w/ blood clotting. "K for K oagulation." Necessary for synthesis of factors II, VII, IX, X, and protein C and S.
question
Vitamin K: synthesis?
answer
Synthesized by intestinal flora.
question
Vitamin K antagonist?
answer
Warfarin.
question
Vitamin K: deficiency?
answer
Neonatal hemorrhage w/ incr PT and incr aPTT, but normal bleeding time (neonates have sterile intestines and are unable to synthesize vitamin K). Neonates are give vitamin K injection at birth to prevent hemorrhage. Can also occur after prolonged use of broad-spectrum ABX.
question
Zinc: fxn?
answer
Essential for the activity of 100+ enzymes. Important in the formation of Zinc fingers (a transcription motif)
question
Zinc: deficiency?
answer
Delayed wound healing, hypogonadism, decr adult hair (axillary, facial, pubic). May predispose to alcoholic cirrhosis.
question
Ethanol metabolism: kinetics?
answer
NAD+ is the limiting reagent. Alcohol dehydrogenase operates via zero-order kinetics.
question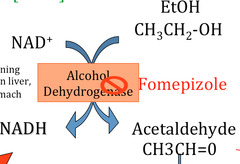
Fomepizole
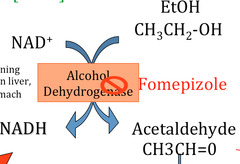
answer
Inhibits alcohol dehydrogenase
question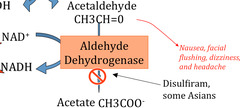
Disulfiram (antabuse)
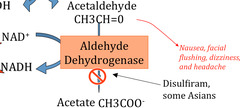
answer
Inhibits acetaldehyde dehydrogenase (acetaldehyde accumulates, contributing to Sx of hangover)
question
Ethanol hypoglycemia
answer
Ethanol metabolism increases NADH/NAD+ ratio in liver, causing a diversion of pyruvate to lactate and OAA to malate, thereby inhibiting gluconeogenesis and stimulating FA synthesis. Leads to hypoglycemia and hepatic fatty change (hepatocellular steatosis) seen in chronic alcoholics.
question
Kwashiorkor
answer
Protein malnutrition resulting in skin lesions, edema, liver malfxn (fatty change). Clinical picture is small child w/ swollen belly. "Kwashiorkor results from a protein-deficient MEAL : M alnutrition, E dema, A nemia, L iver (fatty)"
question
Marasmus

answer
Energy malnutrition resulting in tissue and muscle wasting, loss of subcutaneous fat, and variable edema. "M arasmus results in M uscle wasting"
question
Metabolism sites: Mitochondria
answer
Fatty acid oxidation (beta-oxidation) Acetyl-CoA production TCA cycle Oxidative phosphorylation
question
Metabolism sites: cytoplasm
answer
Glycolysis Fatty acid synthesis HMP shunt Protein synthesis (RER) Steroid synthesis (SER)
question
Metabolism sites: both mitochondria and cytoplasm
answer
H eme synthesis U rea cycle G luconeogenesis "HUG s take two "
question
Process: Glycolysis What is the rate-limiting enzyme?
answer
Phosphofructokinase-1 (PFK-1)
question
Process: Gluconeogenesis What is the rate-limiting enzyme?
answer
Fructose bisphosphatase-2
question
Process: TCA cycle What is the rate-limiting enzyme?
answer
Isocitrate dehydrogenase
question
Process: Glycogen synthesis What is the rate-limiting enzyme?
answer
Glycogen synthase
question
Process: Glycogenolysis What is the rate-limiting enzyme?
answer
Glycogen phosphorylase
question
Process: HMP shunt What is the rate-limiting enzyme?
answer
Glucose-6-phosphate dehydrogenase (G6PD)
question
Process: De novo pyrimidine synthesis What is the rate-limiting enzyme?
answer
Aspartate transcarbamoylase (ATCase)
question
Process: De novo purine synthesis What is the rate-limiting enzyme?
answer
Glutamine-PRPP amidotransferase
question
Process: Urea cycle What is the rate-limiting enzyme?
answer
Carbamoyl phosphate synthetase
question
Process: Fatty acid synthesis What is the rate-limiting enzyme?
answer
Acetyl-CoA carboxylase (ACC)
question
Process: Fatty acid oxidation What is the rate-limiting enzyme?
answer
Carnitine acyltransferase I
question
Process: Ketogenesis What is the rate-limiting enzyme?
answer
HMG-CoA synthase
question
Process: Cholesterol synthesis What is the rate-limiting enzyme?
answer
HMG-CoA reductase
question
Rate-limiting enzyme: HMG-CoA reductase What is the process?
answer
Cholesterol synthesis
question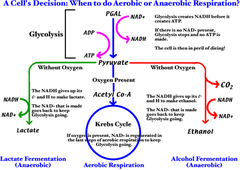
Glycolysis/ATP production
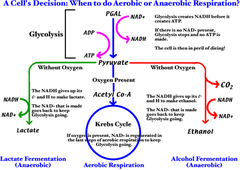
answer
Aerobic metabolism of glucose produces 32 ATP via malate-aspartate shuttle (heart and liver), 30 ATP via glycerol-3 phosphate shuttle (muscle) Anaerobic glycolysis produces only 2 net ATP per glucose molecule. ATP hydrolysis can be coupled to energetically favorable rxtns.
question
Subtance: Electrons-->What is the activated carrier for this substance?
answer
NADH, NADPH, FADH2
question
Subtance: Acyl-->What is the activated carrier for this substance?
answer
Coenzyme A, lipoamide
question
Subtance: CO2-->What is the activated carrier for this substance?
answer
Biotin
question
Subtance: 1-carbon units-->What is the activated carrier for this substance?
answer
Tetrahydrofolate
question
Subtance: CH3 groups-->What is the activated carrier for this substance?
answer
SAM
question
Subtance: Aldehydes-->What is the activated carrier for this substance?
answer
TPP
question
Universal electron acceptors (list)
answer
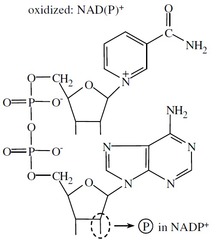
Nicotinamides (NAD+, NADP+) and flavin nucleotides (FAD+)
question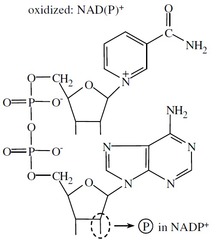
NAD+ vs. NADP+
answer
NAD+ is generally used in catabolic processes to carry reducing equivalents away as NADH. NADPH is used in anabolic processes (steroid and FA synthesis) as a supply of reducing equivalents.
question
NADPH: Product of...? Used in... (3 things)?
answer
Product of the HMP shunt. Used in: 1.) Anabolic processes 2.) Respiratory burst 3.) P-450
question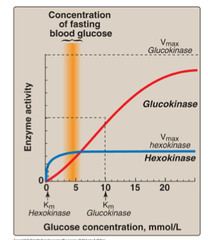
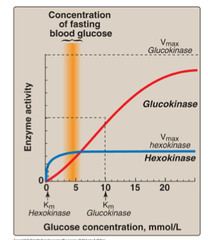
Hexokinase vs. glucokinase: why are the 2 enzymes similar?
answer
Phosphorylation of glucose to yield glucose-6-phosphate serves as the 1st step of glycolysis (also serves as the first step of glycogen synethsis in the liver). Rxtn is catalyzed by either hexokinase or glucokinase
question
Hexokinase vs. glucokinase: Location?
answer
Hexokinase: ubiquitous. Glucokinase: Liver and Beta-cells of pancreas only.
question
Hexokinase vs. glucokinase: Affinity / Capacity?
answer
Hexokinase: high affinity (low Km), low capacity (low Vmax) Glucokinase: Low affinity (high Km), high capacity (high Vmax)
question
Hexokinase vs. glucokinase: response to insulin?
answer
Hexokinase: uninduced by insulin Glucokinase: induced by insulin
question
Hexokinase vs. glucokinase: Feedback?
answer
Hexokinase: Feedback inhibited by glucose-6-phosphate. Glucokinase: No direct feedback inhibition.
question
Hexokinase vs. glucokinase: Role in blood sugar hemostasis?
answer
Glucokinase phosphorylates excess glucose (e.g., after a meal) to sequester it in the liver. Allows liver to serve as a blood glucose "buffer".
question
Net glycolysis rxtn (cytoplasm)
answer
Glucose + 2 Pi + 2 ADP + 2 NAD+ --> 2 pyruvate + 2 ATP + 2 NADH + 2 H+ + 2H2O
question
Regulation of glycolysis

answer
Hexokinase (ubiquitous)/glucokinase (liver) -- (-) feedback from Glucose-6-Phosphate Phosphofructokinase 1 (rate limiting step): (-) feedback from ATP , citrate (+) feedback from AMP, fructose-2,6-bisphosphate
question
Steps in glycolysis that produce ATP: Regulation?
answer
Pyruvate kinase: (-) feedback from ATP, alanine (+) feedback from fructose-1,6-bisphosphate
question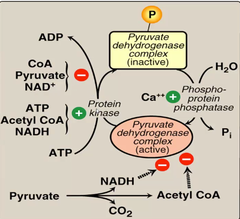
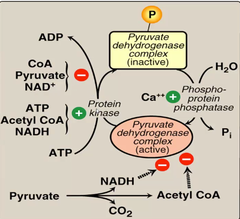
Pyruvate dehydrogenase
answer
Takes pyruvate (the product of glycolysis) and produces Acetyl-CoA, which can enter TCA/Krebs cycle. (-) feedback from: ATP, NADH, Acetyl-CoA
question
Regulation by fructose-2,6-bisphosphate

answer
F2,6BP is the most potent activator of PFK-1 (overrides inhibition by ATP and citrate) and is a potent regulator of glycolysis and gluconeogenesis
question
Glycolytic enzyme deficiency: Associated with...? Why? Due to deficiencies in...?
answer
Associated w/ hemolytic anemia . Inability to maintain activity of Na+/K+ ATPase leads to RBC swelling and lysis. (RBCs metabolize glucse anaerobically - no mitochondria - and thus depend solely on glycolysis. Due to deficiencies in pyruvate kinase (95%), phosphoglucose isomerase (4%), and other glycolytic enzymes.
question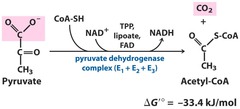
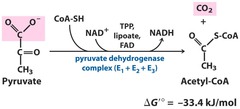
Pyruvate dehydrogenase: net rxtn?
answer
Pyruvate + NAD+ + CoA --> acetyl-CoA + CO2 + NADH
question
Pyruvate dehydrogenase complex: 3 enzymes that require what 5 cofactors?
answer
1.) Pyrophosphate (B1, thiamine; TPP) 2.) FAD (B2, riboflavin) 3.) NAD (B3, niacin) 4.) CoA (B5, pantothenate) 5.) Lipoic acid
question
How does exercise active the pyruvate dehydrogenase complex?

answer
Incr NAD+/NADH ratio Incr ADP Incr Ca2+
question
Pyruvate dehydrogenase complex vs. alpha-ketoglutarate complex
answer
PD complex is similar to the a-KG complex (same cofactors, similar substrate and action), which converts alpha-ketoglutarate --< succinyl-CoA (TCA cycle)
question
Arsenic: inhibits...? Findings w/ poisoning?
answer
Inhibits lipoic acid (cofactor for pyruvate dehydrogenase complex and alpha-KG complex) Findings: vomiting, rice water stools, garlic breath.
question
Pyruvate dehydrogenase deficiency: Causes...? Etiology?
answer
Causes backup of substrate (pyruvate and alanine), resulting in lactic acidosis. Can be congenital or acquired (as in alcoholics due to B1 deficiency).
question
Pyruvate dehydrogenase deficiency: findings?
answer
Neurologic defects
question
Pyruvate dehydrogenase deficiency: Tx?
answer
Incr intake of ketogenic nutrients (e.g., high fat content or incr lysine and leucine) *L ysine and L eucine are the only purely ketogenic amino acids.
question
Pyruvate metabolism: Alanine?
answer
Alanine (made via ALT): carries amino groups to the liver from muscle [#1 above]
question
Pyruvate metabolism: oxaloacetate?
answer
OAA (formed via PC) can replenish TCA cycle or be used in gluconeogenesis [#2 above]
question
Pyruvate metabolism: Acetyl-CoA
answer
#3: transition from glycolysis to the TCA cycle
question
Pyruvate metabolism: Lactate?
answer
#4: End of anaerobic glycolysis (major pathway in RBCs, leukocytes, kidney medulla, lens, testes, and cornea)
question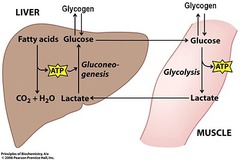
Cori cycle
answer
Allows lactate generated during anaerobic metabolism to undergo hepatic gluconeogenesis and become a source of glucose for muscle/RBCs. This comes at a cost of a net loss of 4 ATP/cycle. Shifts metabolic burden to the liver.
question
Pyruvate --< acetyl-CoA produces what?
answer
1 NADH + 1 CO2
question
The TCA cycle (Krebs) produces what?
answer
3 NADH, 1 FADH2, 2 CO2, 1 GTP per acetyl-CoA = 12 ATP/acetyl-CoA (2x everything per glucose).
question
Where does the TCA cycle rxtn take place?
answer
In the mitochondria.
question
alpha-ketoglutarate dehydrogenase complex
answer
Part of TCA cycle. Requires the same cofactors as the pyruvate dehydrogenase complex (B1, B2, B3, B5, lipoic acid)
question
Enzymes of TCA (Krebs cycle) + schematic

answer
"C itrate I s K rebs' S tarting S ubstrate F or M aking O xaloacetate."
question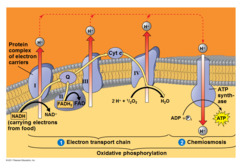
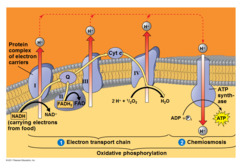
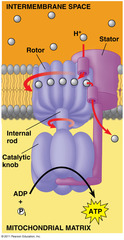
What does the ETC do, and how does it relate to oxidative phosphorylation?
answer
NADH electrongs from glycolysis and the TCA cycle enter mitochondria via the malate-aspartate or glycerol-3-phosphate shuttle. FADH2 electrons are transferred to complex II (at a lower energy level than NADH). The passage of electrons results in the formation of a proton gradient that, coupled to oxidative phosphorylation, drives the production of ATP.
question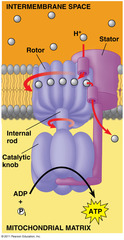
ATP produced via ATP synthase
answer
1 NADH --< 3 ATP 1 FADH2 --< 2 ATP
question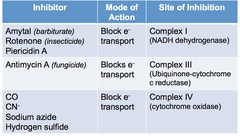
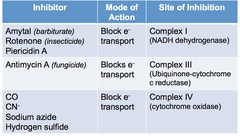
Oxidative phosphorylation poisons: ETC inhibitors?
answer
Directly inhibit electron transport, causing a lower proton gradient and block of ATP synthesis. E.g., Retenone, CN-, antimycin A, CO
question
Oxidative phosphorylation poisons: ATPase inhibitors

answer
Directly inhibit mitochondrial ATPase, causing an incr proton gradient. No ATP is produced b/c electron transport stops. E.g., Oligomycin
question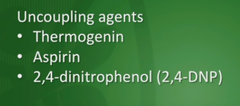
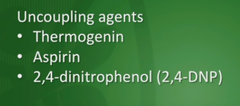
Oxidative phosphorylation proteins: uncoupling agents
answer
Incr permeability of membrane, causing a decr proton gradient and incr O2 consumption. ATP synthesis drops, but electron transport continues. E.g., 2,4-DNP, aspirin, thermogenin in brown fat.
question
Gluconeogenesis, irreversible enzymes: Pyruvate carboxylase Location? Rxtn? Requires...?

answer
In mitochondria. Pyruvate --< Oxaloacetate. Requires biotin, ATP. Activated by acetyl-CoA.
question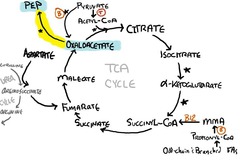
Gluconeogenesis, irreversible enzymes: PEP carboxykinase Location? Rxtn? Requires...?
answer
In cytosol. Oxaloacetate --< phosphoenolpyruvate. Requires GTP.
question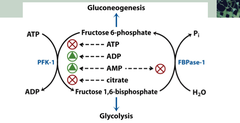
Gluconeogenesis, irreversible enzymes: Fructose-1,6-bisphosphatase Location? Rxtn? Requires...?
answer
In cytosol. Fructose-1,6-bisphosphate --< fructose-6-phosphate
question
Gluconeogenesis, irreversible enzymes: Glucose-6-phosphatase Location? Rxtn? Requires...?
answer
In ER. Glucose-6-P --< glucose.
question
Mnemonic for the irreversible enzymes of gluconeogenesis?
answer
"P athway P roduces F resh G lucose" P yruvate carboxylase P EP carboxykinase F ructose-1,6-bisphosphatase G lucose-6-phosphatase
question
Where does gluconeogenesis occur (anatomically)?
answer
Occurs primarily in liver. Enzymes also found in kidney, intestinal epithelium.
question
Deficiency of gluconeogenesis enzymes causes...?
answer
Causes hypoglycemia. (Muscle cannot participate in gluconeogenesis.)
question
Fatty acids and gluconeogenesis
answer
Odd-chain FA's yield 1 propionyl-CoA during metabolism, which can enter the TCA cycle, undergo gluconeogenesis, and serve as a glucose source. Even-chain FA's cannot produce new glucose, sine they yield only acetyl-CoA equivalents.
question
HMP shunt (pentose phosphate pathway): What does it do? Where does it occur (in the cell)? What is the net ATP requirement or yield?
answer
Produces NADPH, which is req'd for FA and steroid biosynthesis and for glutathione reduction inside RBCs. 2 distinct phases (oxidative and non-oxidative), both of which occur in the cytoplasm. No ATP is used or produced.
question
HMP shunt (pentose phosphate pathway): Where does it occur (anatomically)?
answer
Lactating mamary glands, liver, adrenal cortex (sites of FA or steroid synthesis), RBCs
question
HMP shunt (pentose phosphate pathway): Oxidative rxtns (irreversible) -- key enzymes? products?
answer
Key enzymes: Glucose-6-phosphate dehydrogenase (rate-limiting step) Products: NADPH (for FA and steroid synthesis, glutathione reduction, and cytochrome P-450)
question
HMP shunt (pentose phosphate pathway): Nonoxidative (reversible) -- key enzymes? products?
answer
Key enzymes: Transketolases (require thiamine). Products: Ribose-5-phosphate (for nucleotide synthesis); G3P, F6P (glycolytic intermediates)
question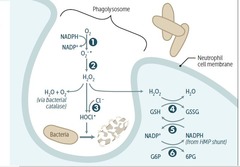
Respiratory burst (oxidative burst)
answer
Involves activation of membrane-bound NADPH oxidase (e.g., in neutrophils, macrophages). Plays an important role in the immune response --< results in the rapid release of reactive oxygen species.
question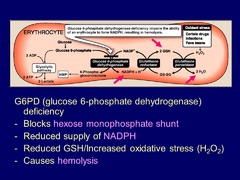
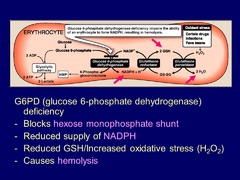
Glucose-6-Phosphate dehydrogenase deficiency: molecular explanation?
answer
NADPH is necessary to keep glutathione reducced, which in turn detoxifies free radicals and peroxides. Decr NADPH in RBCs leads to hemolytic anemia due to poor RBC defense against oxidizing agents (e.g., fava beans, sulfonamides, primaquine, antituberculosis drugs).
question
Glucose-6-phosphate dehydrogenase deficiency: Genetics? Findings in blood?
answer
X-linked recessive d/o; most common human enzyme deficiency; more prevalent among blacks. Incr malarial resistance.
question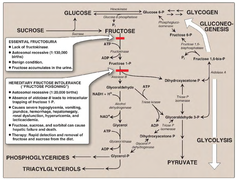
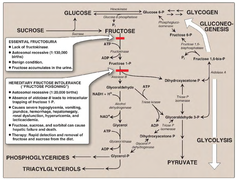
Hereditary Fructose intolerance: Deficiency? Genetics? Biochem/molecular problem?
answer
Hereditary deficiency in aldolase B . Autosomal recessive. Fructose-1-phosphate accumulates, causing a decr in available phosphate, which results in inhibition of glycogenolysis and gluconeogenesis.
question
Fructose intolerance: Sx?
answer
Hypoglycemia, jaundice, cirrhosis, vomiting.
question
Fructose intolerance: Tx?
answer
Decr intake of both fructose and sucrose (glucose + fructose)
question
Essential fructosuria: Defect? Genetics? Biochem/molecular problem?
answer
Involves a defect in fructokinase . Autosomal recessive. A benign, asymptomatic condition, since fructose doesn't enter cells.
question
Essential fructosuria: Sx?
answer
Fructose appears in blood and urine (benign)
question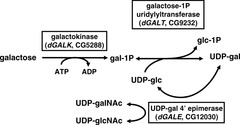
Classic galactosemia: Deficiency? Genetics? Biochem/molec problem?
answer
Absence of galactose-1-phosphate uridyltransferase. Autosomal recessive. Damage is caused by accumulation of toxic substances (including galactitol, which accumulates in the lens of the eye).
question
Classic galactosemia: Sx?
answer
Failure to thrive, jaundice, hepatomegaly, infantile cataracts, mental retardation.
question
Classic galactosemia: Tx?
answer
exclude galactose and lactose (galactose + glucose) from diet.
question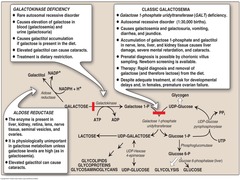
Galactokinase deficiency: Deficiency? Genetics? Biochem/molec problem?
answer
Hereditary deficiency of galactokinase . Autosomal recessive. Galactitol accumulates if galactose is present in diet. Relatively mild condition.
question
Galactokinase deficiency: Sx?
answer
Galactose appears in blood and urine, infantile cataracts. May initially present as failure to track objects or to develop a social smile.
question
Lactase deficiency: what is it?
answer
Age-dependent and/or hereditary lactose intolerance (blacks, Asians) due to loss of brush-border enzyme.
question
Lactase deficiency: Sx? Tx?
answer
Bloating, cramps, osmotic diarrhea. Tx by avoiding dairy products or adding lactase pills to diet.
question
Amino acids: which form is found in proteins?
answer
Only L-form AA's are found in proteins.
question
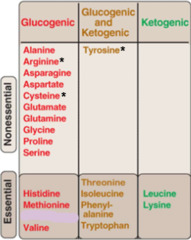
Essential Glucogenic amino acids
answer
Met, Val, Arg, His Glucogenic AA's can be converted into glucose via gluconeogenesis.
question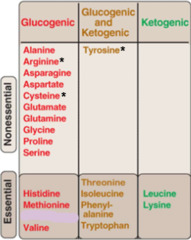
Essential AA's
answer
Met, Val, Arg, His Ile, Phe, Thr, Trp Leu, Lys All essential AA's need to be supplied in diet. (classified as glucogenic and/or ketogenic)
question
Glucogenic/ketogenic AA's
answer
Ile, Phe, Thr, Trp Glucogenic AA's can be converted into glucose via gluconeogenesis. Ketogenic AA's form ketone bodies.
question
Ketogenic AA's
answer
Leu, Lys Ketogenic AA's form ketone bodies.
question
Acidic AA's
answer
Asp and Glu (negatively charged at body pH)
question
Basic AA's
answer
Arg, Lys, and His Arg is the most basic. His has no charge at body pH. Arg and His are req'd during periods of growth. Arg and His are elevated in histones, which bind (-) charged DNA.
question
Urea cycle: fxn/purpose?
answer
Amino acid catabolism results in the formation of common metabolites (e.g., pyruvate, acetyl-CoA), which serve as metabolic fuels. Excess nitrogen (NH4+) generated by this process is converted to urea and excreted by the kidneys.
question
Mnemonic to remeber the important molecules in the urea cycle
answer
"O rdinarily, C areless C rappers A re A lso F rivolous A bout U rination" O rnithine C arbamoyl phosphate C itrulline A spartate A rginosuccinate F umarate A rginate U rea
question
Hyperammonemia: etiology?
answer
Can be acquired (e.g., liver dz) or hereditary (e.g., urea cycle enzyme deficiencies)
question
Hyperammonemia: Result?
answer
Results in exccess NH4+, which depletes alpha-ketoglutarate, leading to inhibition of the TCA cycle. Ammonia intoxication : tremor, slurring speech, somnolence, vomiting, cerebral edema, blurring of vision.
question
Tx for hyperammonemia
answer
Benzoate or phenylbutyrate to lower serum ammonia levels.
question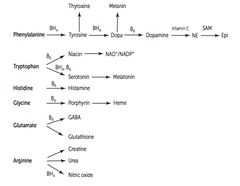
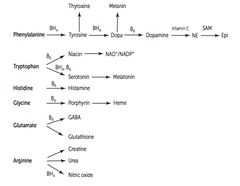
Phenylalanine derivatives
answer
1.) Phenylalanine --< Tyrosine --< Thyroxine + Dopa 2.) Dopa --< Melanin + Dopamine 3.) Dopamine --< NE --< Epi
question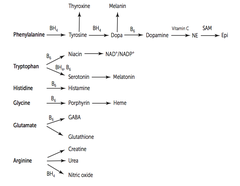
Tryptophan derivatives
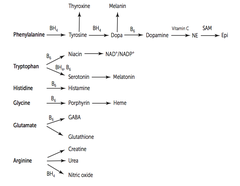
answer
Tryptophan --< Niacin + Serotonin Niacin --< NAD+/NADP+ Serotonin --< Melatonin
question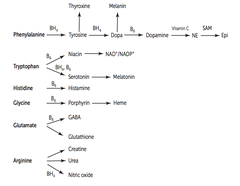
Histadine derivatives
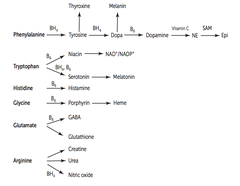
answer
Histadine --< Histamine
question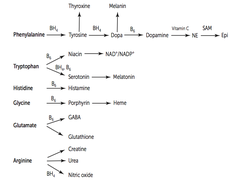
Glycine derivatives
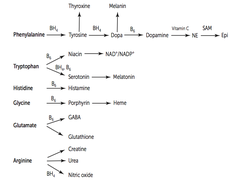
answer
Glycine --< Porphyrin --< heme
question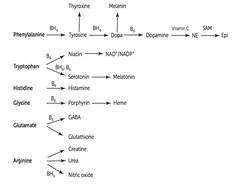
Arginine derivatives
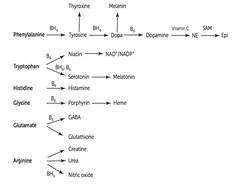
answer
Arginine --< Creatinine, urea, NO
question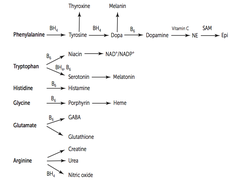
Glutamate derivatives
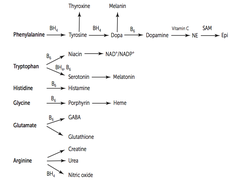
answer
Glutamate --< GABA (glutamate decarboxylase -- requires B6) Glutamate --< Glutathione
question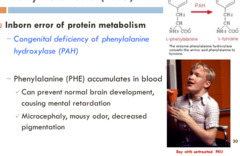
Phenylketonuria: due to...? What does this mean molecularly?
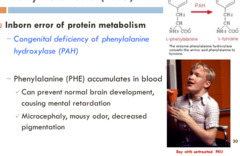
answer
Due to decr phenylalanine hydroxylase or decr tetrahydrobiopterin cofactor. Tyrosine becomes essential. Incr phenylalanine leads to excess phenylketones in urine.
question
Findings w/ PKU
answer
Mental retardation, growth retardation, seizures, fair skin, eczema, musty body odor (d/o of aromatic AA metabolism --< musty body odor ).
question
Tx for PKU
answer
Decr phenylalanine (contained in aspartame, e.g., NutraSweet) and incr tyrosine in diet.
question
Maternal PKU
answer
Lack of proper dietary therapy during pregnancy. Findings in infant: microcephaly, mental retardation, growth retardation, congenital heart defects.
question
PKU: genetics? incidence? screening?
answer
Autosomal recessive. Incidence ~ 1:10,000 Screened for 2-3d after birth.
question
Alkaptonuria (ochronosis): What is it? Genetics? Prognosis?
answer
Congenital deficiency of homogentisic acid oxidase in the degradative pathway of tyrosine. Autosomal recessive. Benign dz.
question
Alkaptonuria (ochronosis): findings?

answer
Dark connective tissue, pigmented sclera, urine turns black on standing. May have debilitating arthralgias.
question
Albinism: etiologies (+ genetics, when applicable)?
answer
Congenital deficiency of either of the following: 1.) Tyrosinase (inability to synthesize melanin from tyrosine) -- Autosomal recessive 2.) Defective tyrosine transporters (decr amounts of tyrosine, and thus melanin) Can result from lack of migration of neural crest cells. Variable inheritance due to locus heterogeneity (vs. ocular albinism -- X-linked recessive)
question
Risk of what dz w/ albinism?
answer
Lack of melanin results in an incr risk of skin cancer.
question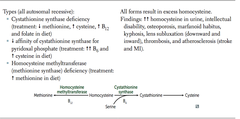
3 Forms of homocystinuria
answer
1.) Cystathionine synthase deficiency (Tx: decr Met and Incr Cys, and incr B12 and folate in diet) 2.) Decr affinity of cystathionine synthase for pyridoxal phosphate (Tx: incr (++) vitamin B6 in diet) 3.) Homocysteine methyltransferase deficiency
question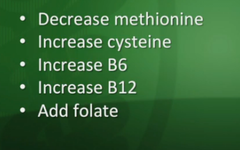
Commonalities for all 3 forms of homocystinuria
answer
All are autosomal recessive. All forms result in excess homocysteine. Cystine becomes essential.
question
Findings w/ homocystinuria
answer
(++) homocysteine in urine, mental retardation, osteoporosis, tall stature, kyphosis, lens subluxation (downward and inward), and atherosclerosis (stroke and MI)
question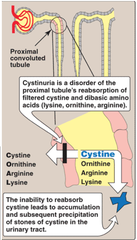
Cystinuria: Etiology? Genetics/incidence?
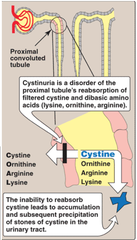
answer
Hereditary defect of renal tubular AA transporter for cysteine, ornithine, lysine, and arginine in the PCT of the kidneys. Autosomal recessive and common (1:7,000)
question
Cystinuria: findings? Tx?
answer
Excess cystine in urine can lead to precipitation of cystine kidney stones (cystine staghorn calculi). Tx: acetazolamide to alkalinize urine *Cystine is make of 2 cysteines connected by a disulfide bond.
question
Maple syrup urine dz: etiology?

answer
Blocked degradation of branched amino acids (I le, L eu, V aline) due to decr alpha-ketoglutarate dehydrogenase. ("I L ove V ermont maple syrup from maple trees with branches .")
question
Maple syrup urine dz: findings?
answer
Causes severe CNS defects, mental retardation, death. Urine smells like maple syrup.
question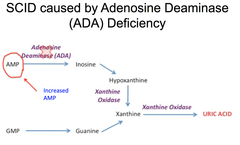
Purine salvage deficiencies: Adenosine deaminase deficiency
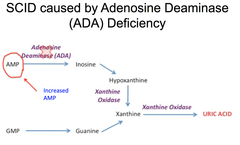
answer
Excess ATP and dATP imbalances nucleotide pool via feedback inhibition of ribonucleotide reductase. | Prevents DNA synthesis and thus decr lymphocyte count. One of the major causes of SCID.
question
SCID (sever combined immunodeficiency dz)
answer
SCID happens to kids (e.g., "bubble boy"). 1st dz to be Tx w/ experimental human gene therapy. One of the major causes of SCID: ADA deficiency
question
Purine salvage deficiencies: Lesch-Nyhan syndrome

answer
Defective purine salvage owing to absence of HGPRT which converts hypoxanthine to IMP and guanine to GMP. Results in excess uric acid production.
question
Lesch-Nyhan syndrome: findings?
answer
Retardation, self-mutilation, aggression, hyperuricemia, gout, choreoathetosis.
question
Lesch-Nyhan syndrome: genetics?
answer
X-linked recessive. HGPRT gene: "H e's G ot P urine R ecovery T rouble"
question
Orotic aciduria: etiology? genetics?
answer
Inability to convert orotic acid UMP (de novo pyrimidine synthesis pathway) due to defect in either orotic acid phosphoribosyltransferase or orotidine 5'-phosphate decarboxylase. Autosomal recessive.
question
Orotic aciduria: findings?

answer
Incr orotic acid in urine, megaloblastic anemia (does not improve w/ administration of vitamin B12 or folic acid), failure to thrive. No hyperammonemia (vs. OTC deficiency -- incr orotic acid w/ hyperammonemia).
question
Orotic aciduria: Tx?
answer
Oral uridine administration.
question
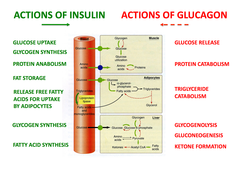
Insulin: when/where is it made? What are its basic effects?
answer
Made in Beta-cells of panccreas in response to ATP from glucose metabolism acting on K+ channels and depolarizing cells. Required for adipose and skeletal muscle uptake of glucose. Inhibits glucagon release by alpha-cells of pancreas.
question
C-peptide
answer
Serum C-peptide is not present w/ exogenous insulin intake (proinsulin --< insulin + C-peptide)
question
Anabolic effects of inuslin (list of 6)
answer
1.) Incr glucose transport ("In sulin moves glucose In to cells." 2.) Incr glycogen synthesis and storage 3.) Incr TG synthesis and storage 4.) Incr Na+ retention (kidneys) 5.) Incr protein synthesis (muscles) 6.) Incr cellular uptake of K+
question
Tissues that don't need insulin for glucose uptake
answer
"BRICK L " B rain R BCs I ntestine C ornea K idney L iver
question
GLUT1 transporter
answer
RBCs, brain
question
GLUT2 transporter
answer
(bidirectional) Beta-islet cells, liver, kidney
question
GLUT4 transporter
answer
(insulin responsive) Adipose tissue, skeletal muscle
question
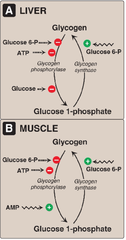
Glycogen synthase: metabolism and activity?
answer
Fed state: *GS* (active) vs. Fasting state: GS-P (phosphorylated, inactive)
question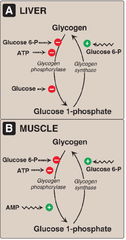
Glycogen synthase: regulation in liver and muscle?
answer
Regulation in liver: (+): Insulin, Glucose (-): Glucagon, epinephrine Regulation in muscle: (+): Insulin (-): Epinephrine
question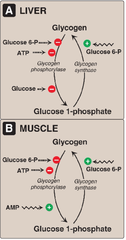
Glycogen phosphorylase (in muscle, V): metabolism and activity?
answer
Is phosphorylated/dephosphorylated similarly to glycogen synthase, with the opposite resulting activity: GP (inactive) in fed state vs. *GP-P* (active, phosphorylated) in fasting state
question
Glycogen phosphorylase (in muscle, V): regulation in liver and muscle?
answer
Regulation in liver: (+): Epinephrine, Glucagon (-): Insulin Regulation in muscle: (+): AMP, Epinephrine (-): ATP, Insulin
question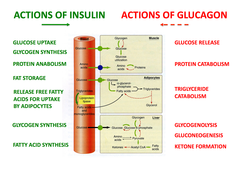
Phosphorylation and Insulin vs. Glucagon
answer
Insulin de phosphorylates (decr cAMP --< decr PKA) Glucagon phosphorylates (incr cAMP --< incr PKA)
question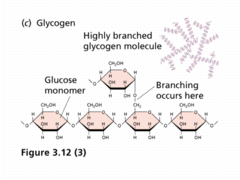
Glycogen structure
answer
Branches have alpha(1,6) bonds; Linkages have alpha(1,4) bonds.
question
Glycogen in skeletal muscle
answer
Glycogen undergoes glycogenolysis to form glucose, which is rapidly metabolized during exercise.
question
Glycogen in hepatocytes
answer
Glycogen is stored and undergoes glycogenolysis to maintain blood sugar at appropriate levels.
question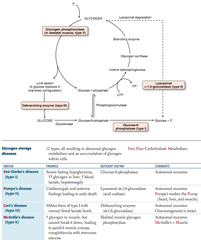
Glycogen synthesis dz's: generallly How many types? Molec path? List?
answer
V ery P oor C arbohydrate M etabolism: V on Gierke's dz (type 1) P ompe's dz (type 2) C ori's dz (type 3) M cArdle's dz (type 5)
question
Glycogen storage dz's: Von Gierke's dz (type I) Findings? Deficient enzyme? Comments?

answer
Findings: severe fasting hypoglycemia, (++) glycogen in liver, incr blood lactate, hepatomegaly. Deficient enzyme: Glucose-6-phosphatase [see below]
question
Glycogen storage dz's: Pompe's dz (type II) Findings? Deficient enzyme? Comments?
answer
Findings: cardiomegaly and systemic findings leading to early death. Deficient enzyme: Lysosomal alpha-1,4 glucosidase (acid maltase "P ompe's trashes the P ump (heart, liver, and muscle)."
question
Glycogen storage dz's: Cori's dz (type III) Findings? Deficient enzyme? Comments?
answer
Findings: milder form of type I w/ normal blood lactate levels. Deficient enzyme: Debranching enzyme (alpha-1,6-glucosidase) Gluconeogenesis is intact.
question
Glycogen storage dz's: McArdle's dz (type V) Findings? Deficient enzyme? Comments?
answer
Findings: incr glycogen in muscle, but cannot break it down, leading to painful muscle cramps, myoglobinuria w/ strenuous exercise. Deficient enzyme: Skeletal muscle glycogen phosphorylase. M cArdle's = M uscle
question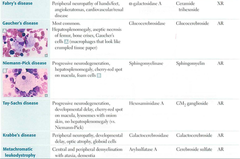
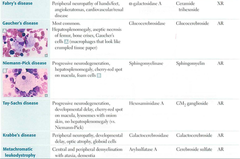
Lysosomal storage dz's (generally)
answer
Each is caused by a deficiency in one of the many lysosomal enzymes. Results in an accumulation of abnormal metabolic products. Include sphingolipidoses and mucopolysaccharidoses.
question
Mnemonic for Niemann-Pick dz?
answer
No man picks (Niemann-Pick ) his nose with his sphinger (sphingo myelinase).
question
Mnemonic for Tay-Sachs?
answer
Tay-SaX lacks heXosaminidase
question
Mnemonic for Hunter's syndrome?
answer
Hunters see clearly (no corneal clouding) and aim for the X (X -linked recessive).
question
Lysosomal storage dz's: population at risk?
answer
Incr incidence of Tay-Sachs, Niemann-Pick, and some forms of Gaucher's dz in Ashkenazi Jews.
question
Fatty acid metabolism: synthesis

answer
"SY trate = SY nthesis"
question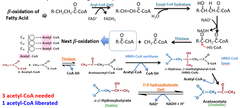
Fatty acid metabolism: degradation
answer
"CAR nitine = CAR nage of FA's"
question
Carnitine deficiency
answer
Inability to utilize LCFAs and toxic accumulation
question
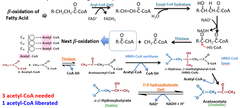
Acyl-CoA dehydrogenase deficiency
answer
Incr dicarboxylic acids, decr glucose and ketones
question
Where does FA degradation take place?
answer
Occurs where its products will be consumed: in the mitochondrion.
question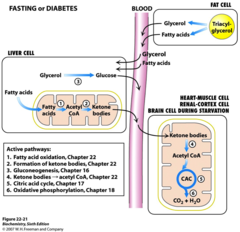
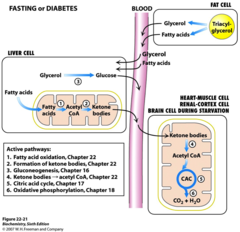
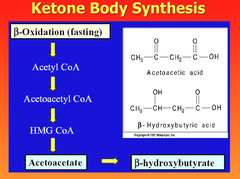
Ketone bodies: in liver?
answer
In the liver, FAs and AAs are metabolized to acetoacetate and Beta-hydroxybutyrate (to be used in muscle and brain)
question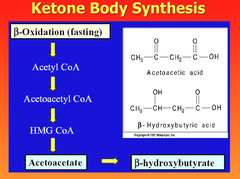
Ketone bodies: in prolonged starvation or diabetic ketoacidosis? ... in alcoholism? Why are these two cases related?
answer
In prolonged starvation or diabetic ketoacidosis, oxaloacetate is depleted for gluconeogenesis. In alcoholism, excess NADH shunts oxaloacetate to malate. Both processes stall the TCA cycle, which shunts glucose and FFA twd the production of ketone bodies.
question
Ketone bodies: made from...? How are they metabolized in brain? How are they excreted?
answer
Made from HMG-CoA. Metabolized in brain to 2 molecules of acetyl-CoA. Excreted in urine.
question
Ketone bodies: findings w/ elevated levels?
answer
Breath smells like acetone (fruity odor). Urine test for ketones does not detect beta-hydroxybutyrate (favored by high redox state).
question
Metabolic fuel use: 1g protein = ? 1g fat = ?
answer
1g protein = 4 kcal 1g fat = 9 kcal
question
Metabolic fuel use: in exercise (generally)
answer
As distances increase, ATP is obtained from additional sources.
question
Metabolic fuel use: in exercise -- 100-meter sprint (seconds)
answer
Stored ATP, creatine phosphate, anaerobic glycolysis
question
Metabolic fuel use: in exercise -- 1000-meter run (minutes)
answer
(;--- as used in sprint) + Oxidative phosphorylation
question
Metabolic fuel use: in exercise -- marathon (hours)
answer
Glycogen and FFA oxidation; glucose conserved for final sprinting.
question
Metabolic fuel use: Fasting and starvation (generally)
answer
Priorities are to supply sufficient glucose to brain and RBCs and to preserve protein.
question
Metabolic fuel use: fasting and starvation -- days 1-3
answer
Blood glucose is maintained by: 1.) Hepatic glycogenolysis and glucose release 2.) Adipose release of FFA 3.) Muscle and liver shifting fuel use from glucose to FFA 4.) Hepatic gluconeogenesis from peripheral tissue lactate and alanine, and from adipose tissue glycerol and propionyl-CoA from odd-chain FFA metabolism (the only TG components that can contribute to gluconeogenesis)
question
Metabolic fuel use: fasting and starvation -- after day 3
answer
Muscle protein loss is maintained by hepatic formation of ketone bodies, supplying the brain and heart.
question
Metabolic fuel use: fasting and starvation -- after several weeks
answer
Ketone bodies become main source of energy for brain, so less muscle protein is degraded than during days 1-3. Survival time is determined by amount of fat stores. After this is depleted, vital protein degradation accelerates, leading to organ failure and death.
question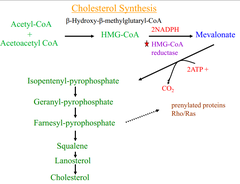
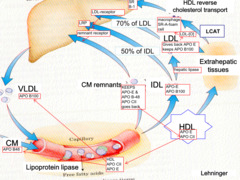
Cholesterol synthesis
answer
Rate-limiting step is catalyzed by HMG-CoA reductase* , which converts HMG-CoA --< mevalonate. 2/3 of plasma XOL is esterified by lecithin-cholesterol acyltransferase (LCAT). *Statins (e.g., lovastatin) inhibit HMG-CoA reductase
question
Essential fatty acids
answer
Linoleic and linolenic acids. Arichidonic acid, if linoleic acid is absent. Eicosanoids are dependent on essential FA's.
question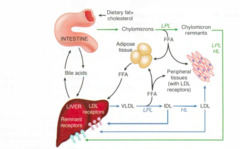
Lipid transport enzymes: Pancreatic lipase
answer
Degradation of dietary TG in small intestine
question
Lipid transport enzymes: Lipoprotein lipase (LPL)
answer
Degradation of TG circulating in chylomicrons and VLDLs
question
Lipid transport enzymes: Hepatic TG lipase (HL)
answer
Degradation of TG remaining in IDL
question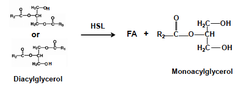
Lipid transport enzymes: Hormone-sensitive lipase
answer
Degradation of TG stored in adipocytes
question
Lipid transport enzymes: Lecithin-cholesterol acyltransferase (LCAT)

answer
Catalyzes esterification of XOL
question
Lipid transport enzymes: Cholesterol ester transfer protein (CETP)

answer
Mediates transfer of XOL-esters to other lipoprotein particles.
question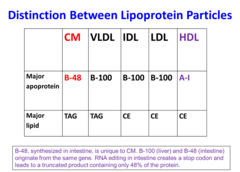
Major apolipoproteins: A-I
answer
A -I A ctivates LCAT
question
Major apolipoproteins: B-100
answer
B -100 B inds to LDL recceptor, mediates VLDL secretion.
question
Major apolipoproteins: C-II
answer
C -II is a C ofactor for lipoprotein lipase.
question
Major apolipoproteins: B-48
answer
Mediates chylomicron secretion.
question
Major apolipoproteins: E
answer
E mediates E xtra (remnant) uptake
question
Lipoprotein fxns (generally)
answer
Lipoproteins are composed of varying proportions of XOL, TGs, and phospholipids. LDL and HDL carry most XOL.
question
Mnemonic for LDL vs. HDL
answer
LDL transports XOL from liver to tissues: "L DL is L ousy" HDL transports XOL from periphery to liver: "H DL is H ealthy"
question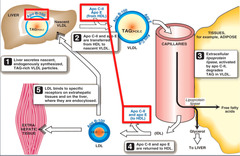
Type of lipoprotein: Chylomicron Function and route? Apolipoproteins?
answer
Deligers dietary TGs to peripheral tissue. Delivers XOL to liver in the form of chylomicron remnants, which are mostly depleted of their triaclyglycerols. Secreted by intestinal epithelial cells. Apolipoproteins: B-48, A-IV, C-II, and E
question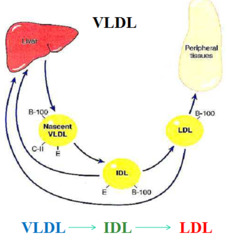
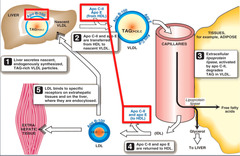
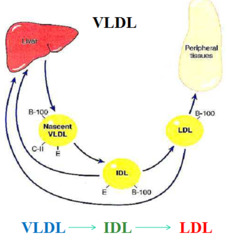
Type of lipoprotein: VLDL Function and route? Apolipoproteins?
answer
Delivers hepatic TGs to peripheral tissue. Secreted by liver. Apo's: B-100, C-II, and E
question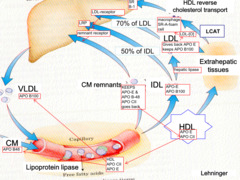
Type of lipoprotein: LDL Function and route? Apolipoproteins?
answer
Delivers hepatic XOL to peripheral tissues. Formed by lipoprotein lipase modification of VLDL in the peripheral tissue. Taken up by target cells via receptor-mediated endocytosis. Apo's: B-100
question
Type of lipoprotein: HDL Function and route? Apolipoproteins?

answer
Mediates reverse XOL transport from periphery to liver. Acts as a repository for apoC and apoE (which are needed for chylomicron and VLDL metabolism). Secreted from both liver and intestine.
question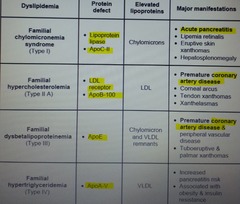
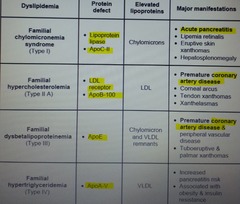
Familial dyslipidemia: Type I - hyperchylomicronemia What's increased? Elevated blood levels of...? Pathophys?
answer
Increased: chylomicrons Elevated blood levels: TG, XOL Pathophys: lipoprotein lipase deficiency or altered apoplipoprotein C-II
question
Familial dyslipidemia: Type IIa - familial hypercholesterolemia What's increased? Elevated blood levels of...? Pathophys?
answer
Increased: LDL Elevated blood levels: XOL Pathophys: Autosomal dominant; absent or decr LDL receptors.
question
Familial dyslipidemia: Type IV - hypertriglyceridemia What's increased? Elevated blood levels of...? Pathophys?
answer
Increased: VLDL Elevated blood levels: TG Pathophys: hepatic overproduction of VLDL
question
Abetalipoproteinemia: what is it? Genetics? Sx? Findings?
answer
Hereditary inability to synthesize lipoproteins due to deficiencies in apoB-100 and apoB-48. Autosomal recessive. Sx appear in the first few months of life. Findings: failure to thrive, steatorrhea, acanthocytosis, ataxia, night blindness.



