Nursing Care of Central Venous Access Devices Nursing 201 Exam 1 – Flashcards
Unlock all answers in this set
Unlock answersquestion
What is CVAD?
answer
They are catheters placed into large veins, usually the subclavian vein or jugular vein to deliver IV therapy Tip is located in the superior vena cava above right atrium Access sites: -internal jugular -subclavian : more secure -cephalic -brachial -basilic -femoral vein SVC - empties into right atrium of heart Other types of lines considered central line (Swan ganz, hemocath
question
where is tip of CVAD located?
answer
Tip is located in the superior vena cava above right atrium
question
Access sites of CVAD?
answer
Access sites: -internal jugular -subclavian : more secure -cephalic -brachial -basilic -femoral vein
question
Purpose of CVAD?
answer
Administration of: -IV fluids -blood and blood products -TPN -meds -traumua pts need fluids fast -vasoactive drugs -chemotherapy: +obtain blood samples +long term IV therapy- hospital, ECF, or home
question
chemotherapy and CVAD
answer
-chemotherapy: +obtain blood samples +long term IV therapy- hospital, ECF, or home
question
Advantages of CVAD
answer
-access to central circulation system -provide access for IV meds, vasoactive vesicants -decrease need for frequent venipuncture -decrease extravasation and phlbetitis -patients with limited peripheral veins -long term IV therapy
question
disadvantages of CVAD
answer
-invasive line -procedure to insert -systemic infection -sepsis -complications air or thrombus embolism, pneumothorax
question
4 Types of CVAD
answer
1. Nontunneled: Central venous Catheters (CVC) Ex. Triple Lumen 2. Tunneled Catheters: Ex. Hickman, Broviac 3. Peripherally Inserted: Central Catheters PICCs 4. Implanted Port: Port-A-Cath
question
Nontunneled Central Venous Catheter site? where inserted? conformation? securement? time frame?
answer
Site: subclavian, jugular or femoral vein Inserted at bedside Placement confirmed with X-ray Held in place with sutures or securement device Short term therapy
question
Nontunneled CVC lumens? flush? risk?
answer
1 to 4 lumens Flush with normal saline May flush with low concentration heparin (100 units/ml) Femoral access possible but not first choice, - increase risk of infection Risk: pneumothorax
question
Tunneled Central Venous Catheter site? insertion? securement? time frame?

answer
Site: chest, subclavian Inserted in OR or IR Held in place Dacron cuff Long term use tunneled subcutaneously to exit site on chest
question
Tunneled Catheter types? how works?
answer
Examples: Groshong, Hickman Has a valve that reduces risk of blood reflux and clotting >> no need for Heparin Pressure opens and closes valve
question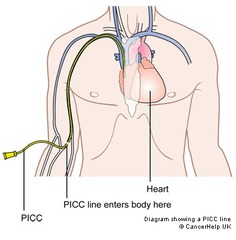
Peripherally Inserted Central Catheter
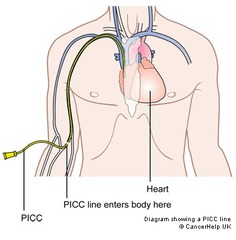
answer
length 20-24 inches No venipunctures or blood pressures in arm Assess for catheter migration by measuring external catheter length from hub to insertion site Held in place with sutures or securement device Power PICC: larger lumen, withstand more pressure *NEVER use a syringe smaller than 10mL * A mid-line catheter is shorter (8-10 inches), not the same Midline tip under axillary area, longer than a peripheral but shorter than CVC, not central venous access Caution: Looks same as PICC but not caution when infusing meds or TPN
question
PICC - Double Lumen

answer
Note clamps and stabilization, 10 ml syringe
question
Implanted Subcutaneous Port site and type
answer
Long term use (oncology patients) Sites: chest, abdomen, inner arm "hidden" under the skin, when not accessed nothing external No dressing change once healed, Tunneled catheter Single or double port Access with a 90 degree non-coring safety needle
question
Port-A-Cath
answer
Surgically implanted port subcutaneously, accessed with Huber needle; flushed with heparin Usually Needle changed every 7 days
question
Needle free cap/hub connector
answer
All CVC need an adapter or "cap" to provide a closed system to prevent air from going in and blood flowing out.
question
Nursing Management of CVADS what needs to be done before using it?
answer
Assist MD/HCP with insertion Confirm placement before using catheter!!!!!! Assessment and maintenance is RN responsibility Maintain patency Maintain sterile technique Apply dressing and cap changes per protocol Administer IV fluids & medications Prevent complications - *infection* * Always per hospital protocol*
question
assessment of catheters
answer
Type of catheter Date inserted, date of last dressing and cap change Skin integrity insertion site & surrounding area- redness, edema, pain, drainage, leaking Assess patency of catheter Assess for signs or complications Assess patient's knowledge ; learning needs
question
Flushing the catheter reason and technique
answer
To maintain patency Wash hands apply non-sterile gloves Flush with 10mls of sterile normal saline (20 mls following blood draw) Use 10 ml pre-filled saline syringe expel all air bubbles Scrub hub - twist alcohol wipe for 15 -30 seconds ; allow to dry Push-Pause technique Flush ALL lumens not being used for infusions Clamp unused ports if indicated per protocol Syringe size - smaller creates increased PSI, "Minimize contamination risk by scrubbing the access port with an appropriate antiseptic (chlorhexidine, povidone iodine, an iodophor, or 70% alcohol)" CDC Guidelines
question
Which lumens get flushed on catheters
answer
Flush ALL lumens not being used for infusions Clamp unused ports if indicated per protocol
question
Push pause technique and why?how to end?
answer
Creates positive pressure ; turbulence to keep catheter patent Push 1 -2 mls, pause, push 1-2 mls pause, continue until all 10 ml instilled but END with positive pressure Alternate pushing ; pausing on syringe plunger apply a steady gentle pressure
question
Flushing catheter procedure?
answer
Don non-sterile gloves "scrub hub" with alcohol or chloraprep Allow to dry Expel air bubbles from 10 mL pre-filled saline syringe Attach saline flush to catheter hub, twist on Inject saline using push-pause technique (positive pressure) End with pressure on plunger while removing syringe Apply disinfectant cap IF Heparin flush indicated per protocol: Scrub hub again for 15 seconds Attach heparin filled syringe (100u or 10u per mL) Instill correct amount of Heparin per hospital protocol Apply disinfectant cap
question
Administering Medication S.A.S.H Method
answer
"Scrub hub" - antiseptic solution (15 - 20 seconds) each ; every time you access S aline - sterile normal saline 10 ml syringe A dminister - IV medication - using 6 rights ; 3 checks! S aline - flush with 10 ml saline after IV medication H eparin - only if indicated **per protocol** **heparin may be used as last flush to prevent thrombus forming, low concentration 100u/mL or 10u/mL
question
why do we use a 10 mL syringe with flushing a catheter?
answer
Use a 10 ml syringe because smaller size syringes create increased pressure on catheter lumen
question
Administering a med via CVAD part 1
answer
Perform the 3 checks ; 5 rights of medication gloves Scrub hub ; allow to dry Attach prefilled 10 mL saline syringe *Pull back plunger slightly to aspirate small amount blood Inject saline using push-pause and remove syringe
question
administering a med via CVAD part 2
answer
Scrub hub again Connect IV tubing with medication ; set IV pump to infuse at correct rate (ml/hr) When infusion complete - Disconnect IV tubing, put a sterile cap on end of IV tubing scrub hub and flush (push-pause) with 10 mLs of saline If using Heparin ; scrub hub again and administer Heparin as prescribed per hospital protocol Apply disinfectant cap Clamp CVC if indicated
question
CVAD dressing change
answer
Gauze dressing for first 24 hours then..... Transparent dressing Wash site with antiseptic solution (chlorhexidine) for 30 seconds Chloraprep applicator - break ampule release antiseptic into sponge allow time to air dry Apply stabilization device label dressing Usually every 7 days ; PRN Measure catheter length
question
Central Line Dressing Kit
answer
it is a sterile container mask, gloves, chloraprep, transparent dressing, tape, gauze, label
question
how to secure CVAD
answer
with stabilization device
question
Dressinf change procedure
answer
1. Wash hands 2. Open sterile dressing kit 3. Don mask ; nonsterile gloves 4. Remove old dressing with clean gloves 5. Inspect insertion site (redness, drainage, edema) 6. Don Sterile gloves 7. Wash site - with chlorhexidine for 30 seconds using repeated back ; forth strokes, entire area under dressing, gentle back ; forth friction 8. Allow to air dry 9. Apply sterile transparent dressing (no wrinkles) 10. Position so insertion site is in center of dressing 11. If CHG gel pad dressing center it over insertion site 12. Apply securement tape or device if indicated 13. Label dressing - date, time ; initials 14. Wash hands 15. Document
question
cap change for CVAD
answer
Change Caps per agency protocol Prime cap with sterile normal saline Clamp catheter Using aseptic technique twist off old cap Scrub the end (threads) of catheter 15 to 30 seconds with alcohol Attach new cap twist completely Unclamp ; Flush catheter Apply disinfectant cap
question
nursing interventions for CVAD? can it be delegated?
answer
Draw blood samples - discard 3-5 mLs first, draw blood samples then flush with 20 mL NS Measure length of catheter (PICC ; Hickman) Measure circumference of arm (PICC) Apply securement device Assess insertion site for signs of infection *Document- assessment, dressing ; cap change Patient teaching for home care Care of CVAD can not be delegated
question
revmoval of CVAD
answer
*** According to agency policy *** RNs that have demonstrated competency Remove dressing, sutures, stabilization device Ask patient to perform the Valsalva maneuver, take deep breath ; hold it. Valsalva maneuver to prevent air embolism Remove catheter with smooth continuous motion Inspect tip of catheter; ? send tip for culture Apply pressure to insertion site Apply dressing- petroleum-based occlusive dressing antibiotic ointment Measure tip of catheter, PICC
question
what type of dressing is applied after CVAD removal?
answer
Apply dressing- petroleum-based occlusive dressing antibiotic ointment
question
CVAD: what assessments will be found and the interventions for CVAD occlusion or formation of clot?
answer
Assessment: Can not flush. No blood return check for mechanical obstruction 1st intervention: Flush using proper technique Heparinize if indicated Administer thrombolytics per protocol only
question
CVAD: what assessments will be found and the interventions for CVAD Blood infection CR-BSI (CLABSI) Local or systemic
answer
assessment: Fever, Shaking, chills, Positive blood cultures interventions: Strict asepsis Clean skin with antiseptic Cap changes Scrub hub Culture ; Antibiotics
question
CVAD: what assessments will be found and the interventions for CVAD Pneumothorax complication
answer
assessment: Absent breath sounds Chest pain respiratory distress interventions: CXR Oxygen Chest Tube
question
CVAD: what assessments will be found and the interventions for CVAD Embolism air or thrombus complication
answer
assessment: Chest pain respiratory distress interventions: Clamp, Valsalva Oxygen Pt. on left side
question
CVAD: what assessments will be found and the interventions for CVAD Malposition or Dislodgement
answer
assessment: No blood return Edema at site Occlusion interventions: Confirm placement Aspirate for blood return Use securing device Assess length
question
other possible CVAD complications
answer
Other complications: skin erosion, catheter damage or breakage, infiltration, extravasation, incorrect placement
question
Preventing CLABSI (CVAD)
answer
Institute for Healthcare Improvement The Central line bundle is a set of 5 interventions 1. Hand hygiene 2. Maximal barrier on insertion 3. Chlorhexidine skin antisepsis 4. Site selection 5. Daily review for need with prompt removal of unnecessary lines Use of disinfectant caps
question
catheter occlusion
answer
Intraluminal thrombus Inability to flush or aspirate blood from catheter Never force flush when meeting resistance Follow protocol for declotting catheter Use a "clot buster" ex., Alteplase * Per agency protocol only* NEVER flush a CVAD, administer medication or perform dressing or cap change without your Clinical instructor present
question
key points to remember with CVAD
answer
Fluid ; Electrolytes Skin Integrity Infection



