Ch 22 The Child with Gastrointestinal Dysfunction – Flashcards
Unlock all answers in this set
Unlock answersquestion
Distribution of Body Fluids
answer
Intracellular fluid (ICF) Extracellular fluid (ECF) Total body water (TBW) Maintenance water requirements Altered fluid requirements in various conditions
question
Altered fluid requirements
answer
Increased requirements: Fever Diabetes- ketoacidosis Tachypnea Burns Shock Radiant warmer phototherapy Decreased requirements: Heart failure Syndrome of inappropriate antidiuretic hormone Mechanical ventilation Increased ICP
question
Fluid Volume Requirements
answer
Growth related- % body wt. in H20 decreases during first year of life. Water balance in infants-very vulnerable to alterations Body surface area (BSA)- allows for large amount of fluid to be lost through skin Basal metabolic rates-higher in infants and children to support cell and tissue growth Kidney function-infant has inefficient kidneys and cannot concentrate or dilute urine Fluid requirements-can under hydrate and overhydrate quickly
question
Dehydration
answer
Types of dehydration- Isotonic- equal depletion of water and electrolytes Hypertonic-more loss of water than electrolytes Hypotonic-more loss of electrolytes than water Degrees of dehydration p.694 textbook Pulse increases, wt. loss, thirst, decreased UOP Diagnostic evaluation Therapeutic management Parenteral fluid therapy Nursing considerations
question
Clinical Manifestations of Gastrointestinal (GI) Dysfunction
answer
Impaired functional integrity Failure to thrive Spitting up, regurgitation Constipation GI losses of fluid; absorption disorders Nausea, vomiting Diarrhea GI track anomalies Inflammatory disorders Crohn disease; liver failure Fever
question
Diarrhea (1 of 3)
answer
Acute diarrhea is the leading cause of illness in children younger than 5 years of age In developing countries, 20% of all deaths are related to diarrhea and dehydration Acute infectious diarrhea has a variety of causative organisms
question
Diarrhea (2 of 3)
answer
Diarrheal disturbances Gastroenteritis Rotavirus infection-most children have in preschool years Bacterial pathogens Antibiotic-associated etiology Enteritis- inflammation of small intestines Colitis-inflammation of colon Enterocolitis- inflammation of small intestines and colon
question
Diarrhea (3 of 3)
answer
Diagnostic evaluations: hx; lab if severely hydrated Therapeutic management Oral rehydration therapy Prevention: Teach good hygiene Teach about traveler's diarrhea Nursing considerations Teach how to monitor diapers and fontanels in infants for dehydration
question
Oral Rehydration Therapy
answer
Effectively enhances and promotes reabsorption of sodium and water Commercially prepared or home recipes Use alone or in combination with breast milk and infant formula Diarrhea losses are replaced 1:1 (4-8 oz. per stool) Oral intervals in small frequent intervals 5-10 ml increments every 1-5 minutes with spoon Give orally (PO) or via nasogastric (NG) tube
question
Prevention of Diarrhea
answer
Teach personal hygiene Most diarrhea is spread by the fecal-oral route Make sure the water supply is clean and protected from contamination Prepare food carefully Wash hands
question
Constipation
answer
An alteration in frequency, consistency, or ease of passage of stool x 2 weeks May be secondary to other disorders Idiopathic (functional) constipation has no known cause-most common Chronic constipation may be due to environmental or psychosocial factors
question
Constipation in Newborn Period
answer
First meconium should be passed within 24 to 36 hours of life; if not, assess for: Anal patency with rectal temperature on first reading Hirschsprung disease Hypothyroidism Meconium plug or meconium ileus (cystic fibrosis)
question
Constipation in Infancy
answer
Often related to diet Constipation in exclusively breastfed infants is almost unknown Formula-fed infants may develop constipation Nursing management: Help determine cause Food history
question
Constipation in Childhood
answer
Often a result of environmental changes or control over body functions Encopresis is inappropriate passage of feces, often with soiling May result from stress Relationship to urinary tract infections Nursing management
question
Hirschsprung Disease (1 of 2)
answer
Also called congenital aganglionic megacolon Mechanical obstruction from inadequate motility of the intestine due to lack of enteric nervous system stimulation and inability of the rectal sphincter to relax. Incidence is 1 in 5000 live births; more common in males and in children with Down syndrome Absence of ganglion cells in colon
question
Clinical Manifestations of Hirschsprung Disease
answer
Accumulation of stool with distention leading to obstruction Failure of internal anal sphincter to relax Newborns: Failure to pass meconium Refusal to feed Vomiting Abdominal distention Infants: Enterocolitis (fever, explosive diarrhea) Failure to thrive Abd distention Vomiting Children: Constipation Ribbon like, foul smelling stools Visible peristalsis Abdominal distention Palpable fecal mass Undernourished, anemic
question
Diagnostic Evaluation of Hirschsprung Disease
answer
X-ray, barium enema Anorectal manometric examination Confirm the diagnosis with rectal biopsy
question
Therapeutic Management of Hirschsprung Disease
answer
Surgery-removal of the aganglionic portion of the bowel to relieve obstruction, restore normal motility, and preserve the function of the external anal sphincter. (Soave endorectal pull through procedure) Preoperative care: Saline enemas Antibiotics- decrease normal flora Baseline vitals and abd girth measurements Postoperative care: Watch for sx of infection Watch for passage of stool Daily dilation of anal canal to prevent strictures Some may have temporary colostomy
question
Vomiting
answer
Many causes but usually self-limiting requiring no treatment) Nonbilious and bilious types (bile suggest obstruction) Identify associated symptoms: Abdominal pain Diarrhea/constipation fever Therapeutic management Prevent dehydration Provide antiemetics prn (ondansetron, promethazine) Nursing management Monitor for dehydration, side lying position
question
Gastroesophageal Reflux (GERD)
answer
Defined as transfer of gastric contents into the esophagus Most frequently after meals and at night Common in 4 to 12 month olds Becomes disease with failure to thrive, respiratory problems, or dysphagia) Predisposition and prevalence: preterm infants, scoliosis, respiratory problems, abdominal issues Frequency and persistency may make it abnormal Diagnosis: vomiting, excessive crying, cough, wheeze, heartburn, abdominal pain, pneumonia, laryngitis Management: dietary modifications, H2 receptor antagonists, PPIs Nursing management: teaching
question
Recurrent and Functional Abdominal Pain
answer
Recurrent abdominal pain (RAP) Often has a psychogenic cause, but may also be caused by a disease Functional abdominal pain Intermittent or continuous pain that occurs at least once a week for 2 months Most common in school age child Diagnostic evaluation: Somatic disposition and disorders Lifestyle habits Temperament and learned responses Family, social, and cultural norms Management: high fiber diet, psyllium bulk agents, dietary modifications, toileting patterns and routines
question
Acute Appendicitis
answer
Etiology and pathophysiology: inflammation of the vermiform appendix Most common cause of emergency surgery in children Diagnostic evaluation: periumbilical pain, nausea, RLQP (McBurney's point), vomiting, and fever, elevated WBC Therapeutic management Ruptured appendix- complicates 20-30% of cases Prognosis: abscess, peritonitis bowel obstruction CT Nursing considerations Postop Care: laparoscopic appendectomy Return of BS Pain management Dressing changes
question
Meckel Diverticulum
answer
Most common congenital malformation of the GI tract-remnant of fetal omphalomesenteric duct Occurs in 2% to 4% of the population- rule of 2s Pathophysiology: bleeding, obstruction or inflammation Diagnostic evaluation: bright red stools (currant jelly-like), abdominal pain, rectal bleeding Meckel Scan, CT, MRI Therapeutic management: surgical removal Nursing management: manage bleeding, IV replacement, pain relief, NG decompression
question
Inflammatory Bowel Disease (IBD): ulcerative colitis and chron disease
answer
ulcerative colitis (UC) : inflammation of colon and rectum Crohn disease: inflammation anywhere from mouth to anus but common in ileum Etiology questionable Diagnostic evaluation: ESR, CRP CBC,upper gi series, colonoscopy Therapeutic management Goal is to induce and maintain remission Nutritional support Surgical interventions: colectomy, colostomy, ileostomy Nursing considerations
question
Peptic Ulcer Disease (PUD)
answer
Etiology: unknown and pathophysiology: imbalance between the destructive and defensive factors in the GI tract Diagnostic evaluation: CBC, LFTs, amylase, lipase, Sed rate, CRP, gi series with biopsies for H. pylori Characteristics: poor feeding, epigastric pain, hematemesis, melena Therapeutic management Medical: abx, H2 receptor antagonists, PPIs: Nursing considerations Monitor for bleeding, fluid replacement, wt. stabilization
question
Acute Hepatitis
answer
Etiology: acute or chronic inflammation of the liver Viral Chemical reaction Drug reaction Other disease processes Reye syndrome
question
Types of Hepatitis: The liver alphabet
answer
Hepatitis A Hepatitis B Hepatitis C Hepatitis D Hepatitis E Hepatitis G
question
Hepatitis
answer
Swelling and damage of parenchymal cells in liver causing degeneration, necrosis, fibrosis that impairs bile excretion, elevates transaminase levels, and decreases albumin synthesis- may be self limiting Manifestations: Prodromal: Anorexia, malaise, lethargy, and easy fatigability Fever N/V Epigastric pain/RUQP Arthralgia and skin rashes ( children) Icteric: Jaundice Dark urine, pale stools Pruritus hepatomegaly
question
Hepatitis cont.
answer
Liver failure: Mental status changes Encephalopathy Ascites Increase white blood cell count Diagnostics: Markers for Hep A, B, C AST and ALT elevated Bilirubin elevated Liver biopsy
question
Hepatitis Management and Teaching
answer
Management Early detection Prevention of spread Well balanced diet Supportive care Interferon alpha lamivudine Prevention teaching Proper hand washing Standard precautions Immune globulin after exposure Hep A and B vaccines Infectious with Hep A until one week post jaundice Caution with drugs due to decreased liver function Discussion of high risk behaviors
question
Biliary Atresia
answer
Progressive inflammatory process that cause both intrahepatic and extrahepatic bile duct fibrosis resulting in ductal obstruction occurring 2-3 weeks after birth Manifestations: Jaundice (1st observed in sclera) Dark yellow urine White or tan stools Failure to thrive Pruritus irritability
question
Biliary Atresia
answer
Diagnostics: CBC, LFTs, bilirubin Abdominal ultrasound Exploratory laparotomy Management: Hepatic portoenterostomy intestine is anastomosed to resected port hepatis to drain bile (Roux-en Y) May require liver transplant Gastrostomy feedings or TPN Nursing Care: Colloidal oatmeal baths for pruritus Teach parents to feed using gastrostomy tube
question
Cleft Lip and Cleft Palate
answer
Facial malformations that occur during embryonic development May appear separately or together Most common congenital malformation in the U.S. Etiology: thought to be associated with folate deficiency, smoking, alcohol, and other medications Diagnostic: in-utero by ultrasound, on newborn exam Management: surgical correction
question
Surgical Correction of Cleft Lip
answer
Closure of the lip defect precedes correction of the palate Z-plasty to minimize retraction of the scar Protect the suture line with a Logan bow or other methods
question
Surgical Correction of Cleft Palate
answer
Typically done at 12 to 18 months of age Effect on speech development Prognosis Nursing considerations Pain management Feeding (suck and swallow impaired, special nipple) Preoperative care Postoperative care Upright feeding Post op syringe feed
question
Esophageal Atresia and Tracheoesophageal Fistula
answer
Rare malformation representing a failure of the esophagus to develop as a continuous passage separate from the trachea Clinical Manifestations: 3 C's Coughing Choking Cyanosis Apnea Abdominal distention Management: #1 priority maintain patent airway Prevent pneumonia Gastric or blind pouch decompression Surgical repair
question
Esophageal Atresia and Tracheoesophageal Fistula
answer
Nursing Care: NPO Position upright to facilitate drainage of secretions Suction with double lumen cath Antibiotics- broad spectrum Gastrostomy feedings Wt. gain, fluid balance, and growth Prevent respiratory distress
question
Hernias
answer
Protrusion of a portion of an organ through an abnormal opening Typically, inguinal (children, males) or umbilical hernia (newborns) Rarely, diaphragmatic hernia Danger of incarceration or strangulation incarcerated- can't be reduced Strangulated- circulation impaired Gastroschisis Omphalocele
question
Hypertrophic Pyloric Stenosis
answer
Occurs when circumferential muscle of the pyloric sphincter become thickened resulting in elongation and narrowing of the pyloric channel. Manifestations: No abdominal pain Upper abdominal distention Projectile vomiting Dehydration Weight low Visible peristalsis
question
Hypertrophic Pyloric Stenosis
answer
Diagnostics: "olive-like" mass is palpable when the stomach is empty Management: Pyloromyotomy-standard therapy Nursing Care: Rehydrate and correct acid-base balance- pre op Fluid balance, feedings at 12 hours, watch for infection - post op
question
Intussusception
answer
Most common cause of intestinal obstruction in children; typically occurs from age 5 months to 3 years Patho: proximal segment of bowel telescopes into a more distal segment causing lymphatic and venous obstruction, venous engorgement cause manifestations. Manifestations: Sudden, acute abdominal pain RUQ sausage type mass Currant jelly stools (bright bloody) vomiting
question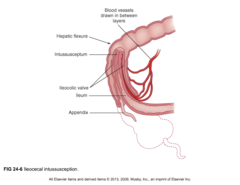
Intussusception
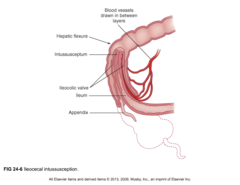
answer
Diagnostics: ultrasound Management: Pneumoenema (air) Saline enema NG decompression Antibiotics Surgical correction if needed
question
Malrotation and Volvulus
answer
Malrotation is abnormal rotation around the superior mesenteric artery during embryonic development Volvulus is twisting of the intestine around itself, compromising the blood supply to the intestines May cause intestinal perforation, peritonitis, necrosis, and death
question
Anorectal Malformations
answer
Some of the most common congenital malformations Rectal atresia- complete obstruction and require immediate surgical intervention Rectal stenosis- diagnosed later in infancy, constipation with ribbon like stools Persistent cloaca-rectum, vagina, and urethra drain into a common channel opening in the perineum Imperforate anus (with or without fistula) Genitalia may be indefinite Diagnostics: physical exam- absent anal opening Management: surgical correction, colostomy Nursing management: Id newborns with issue Sx of infection IV fluids, antibiotics
question
Malabsorption Syndromes
answer
Characterized by chronic diarrhea and malabsorption of nutrients May result in failure to thrive Classified as Digestive defects: conditions in which the enzymes necessary for digestion are diminished or absent Cystic fibrosis- pancreatic enzymes Biliary or liver dz- bile Lactase deficiency- lactose intolerance Absorptive defects: conditions in which intestinal mucosal transport system is impaired due to celiac dz or IBD Anatomic defects: resection of the bowel or short bowel syndrome by decreasing transit time and affecting absorption by compromised surface area.
question
Celiac Disease
answer
Also known as gluten-induced enteropathy or celiac sprue Permanent GI intolerance to dietary wheat and related proteins Four characteristics: Steatorrhea General malnutrition Abdominal distention Secondary vitamin deficiencies
question
Celiac Disease
answer
Pathophysiology Genetic predisposition There is an accumulation of toxic substances that is damaging to the mucosal cells leading to villous atrophy, hyperplasia and infiltration of epithelial cells with lymphocytes Manifestations: Steatorrhea Foul smelling stools Anemia, anorexia Abd distention irritability Diagnostic evaluation: Serological test for markers Upper gi endoscopy with biopsy
question
Celiac Disease
answer
Management: Dietary restrictions- "gluten free" Nursing Care: Teaching It is impossible to remove all gluten, but decrease significantly Use corn, rice, and millet as grain foods Supplement iron, folic acid, and fat soluble vitamins
question
Foods with gluten
answer
Cereal Baked goods Frequently added to processed foods as thickeners or filler Learn to read labels Pizza, cake, doughnuts, malts, hot dogs, lunch meats, pies, spaghetti
question
Short-Bowel Syndrome (SBS)
answer
Malabsorptive disorder resulting from decreased mucosal surface area, usually as a result of small bowel resection Common causes: Necrotizing enterocolitis Volvulus Jeujenal atresias Gastroschisis- abdominal orgarns protrude through hole in abdomen (no membrane covering) Omphalocele- abdominal organs protrude through hole in umbilicus and covered by thin membrane
question
Short Bowel Syndrome (SBS)
answer
2 characteristics: Decreased intestinal surface area for absorption of fluid, electrolytes, and nutrients A need for parenteral nutrition
question
A 7-year-old child with acute diarrhea has been rehydrated with oral rehydration therapy. Which of the following changes in the child's diet should the nurse recommend?
answer
A. Clear liquids B.BRAT diet (banana, rice, apple, toast or tea) C. High-carbohydrate diet D. Regular diet
question
A 6-year-old child is brought to the clinic with a 2-day history of nausea and vomiting. The child has a fever of 101.8°F and episodic abdominal pain at the umbilicus and in the lower left quadrant.
answer
What are the nursing priorities for this child? What diagnostic tests are expected?
question
It is determined that the child has acute appendicitis and will require emergent surgery.
answer
What are the nursing priorities preoperatively? What are the nursing priorities postoperatively?



