Hand & UE – Flashcards
Unlock all answers in this set
Unlock answersquestion
Palmar abduction

answer
Abductor pollicus brevis
question
Thumb opposition
answer
Opponens pollicus
question
Thumb MCP flexion
answer
Flexor Pollicus Brevis
question
MCP Flexion & IP Extension of digits II & III
answer
Lumbricals (Radial)
question
Abduction of the 5th digit
answer
Abductor Digiti Mini
question
Opposition of the 5th Digit
answer
Opponens Digiti Mini
question
5th digit MCP flexion & opposition
answer
Flexor Digiti Mini
question
Adducts CMC joint of thumb
answer
Adductor
question
MCP Flexion & IP Extension of digits IV & V
answer
Lumbricals (Ulnar)
question
Adduction* & assistance with MCP flexion & IP extension of digits II through V
answer
Palmar Interossei
question
Abduction* & assistance with MCP flexion & IP extension of digits II through V
answer
Dorsal Interossei
question
Flexion of PIP joints

answer
Flexor digitorum superficialis (FDS)
question
Flexion of DIP joints in digits II through V

answer
Flexor digitorum profundus (FDS)
question
Flexion of IP of thumb

answer
Flexor Pollicus Longus (FPL)
question
Extension of MCP's ; IP's
answer
Extensor Digitorum Communis (EDC)
question
Extension of IP of thumb
answer
Extensor Pollicus Longus (EPL)
question
Extension of CMC & MCP of thumb
answer
Extensor Pollicus Brevis (EPB) *B comes before L for longs so CMC & MCP for B since first!
question
Abduction & extension of CMC
answer
Abductor Pollicus Longus (APL)
question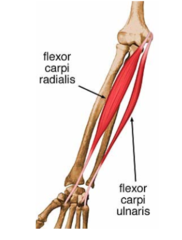
Wrist flexion & RD
answer
Flexor Carpi Radialis (FCR)
question
Flexion of wrist

answer
Palmaris longus
question
Flexion of wrist & UD
answer
Flexor Carpi Ulnaris (FCU)
question
Wrist extension & RD
answer
Extensor Carpi Radialis Brevis (ECRB) AND Extensor Carpi Radialis Longus (ECRL) *Brevis 3, Longus 2
question
Wrist extension & UD
answer
Extensor Carpi Ulnaris (ECU)
question
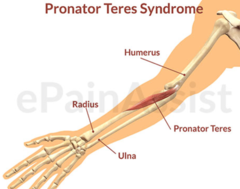
Forearm Pronation

answer
Pronator Teres & Quadratus *Pic is Pronator Teres
question
Forearm Supination

answer
Supinator
question
Elbow flexion in supinated position
answer
Biceps
question
Elbow Flexion in pronated position

answer
Brachilais
question
Elbow flexion in neutral position

answer
Brachioradialis
question
Elbow extension

answer
Tricep & anconeus
question
Rotator cuff muscles of SHOULDER?
answer
SITS: 1. Supraspinatus 2. Infraspinatus 3. Teres minor 4. Subscapularis
question
IR of shoulder

answer
Subscapularis
question
Abduction & flexion of shoulder

answer
Supraspinatus
question
ER of shoulder (2)

answer
Infrapsinatus & Teres minor
question
Shoulder flexion (3)
answer
Anterior deltoid & corachiobrachilais & supraspinatus
question
Shoulder abduction (2)
answer
Middle deltoid & supraspinatus
question
Shoulder horizontal ab*duction?
answer
Posterior deltoid
question
Shoulder horizontal add*uction
answer
Pec major
question
Shoulder extension? (3)
answer
Latissimus dorsi, Teres major & Post deltoid
question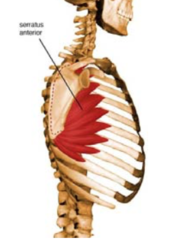
Upward rotation of Scapula (2)
answer
Trapezius & Serrates Anterior
question
Downward rotation of Scapula (4)
answer
Latissimus Dorsi, Levator Scapula, Rhomboids& Serratus Anterior
question
Scapular ADDuction? (2)
answer
Middle Trap Rhomboid Major
question
Scapular ABduction
answer
Serrates anterior
question
Scapular elevation (2)

answer
Trapezius & Levator Scapulae
question
Scapular depression

answer
Trapezius
question
Disease of the fascia of the palm & digits where fascia becomes thick & extends into cords & bands in digits Result: flexion deformities of involved digits *Conservative tx has NOT been successful; surgical operations needed
answer
Dupuytren's
question
OT intervention with Dupuytren's? (6)
answer
1. Wound care: dressing changes 2. Edema control: elevation of hand above heart 3. Extension splint: Initially, at all times, except to remove for ROM & bathing 4. AROM to PROM and progress to strengthening once wounds are healed* 5. Scar management: massage, scar pad, compression garment 6. Purposeful & occupation-based tasks that emphasize flexion (gripping) & extension (release)**
question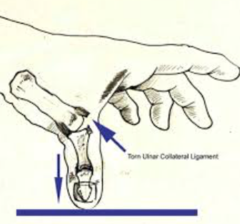
Rupture of the ulnar collateral ligament (UCL) of the thumb joint
answer
Skier's Thumb (Gamekeepers Thumb) *Most common cause: Fall while skiing with thumb held in ski pole
question
OT intervention for Skier's Thumb? (4)
answer
1. Conservative treatment for 4-6 weeks with THUMB SPLINT 2. AROM & pinch strengthening at 6 weeks 3. ADL's that require opposition ; pinch strength 4. Post-op tx involves: thumb splint for 6 weeks, followed by AROM; PROM can begin at 8 weeks; strengthening at 10 weeks
question
Vasomotor dysfunction as a result of an abnormal reflex -It can be localized to one specific area or spread to other parts of the extremity *May follow trauma (i.e. Colles fx) or surgery, but actual cause is unknown
answer
Complex Regional Pain Syndrome (CRPS)
question
Severe pain Edema Discoloration Osteoporosis Sudomotor changes Temperature changes Trophic changes Vasomotor Instability
answer
Symptoms of CRPS
question
OT Intervention CRPS? (5)
answer
1. Modalities to decrease pain 2. Edema Management: elevation, manual mobilization, compression glove 3. STRESS LOADING** (weight bearing ; joint distraction activities, including scrubbing ; carrying activities) 4. Splinting to prevent contractors ; enable engagement in occupation-based activities 5. Encourage self management
question
Interventions to AVOID/proceed with caution with CRPS? (5)
answer
1. PROM 2. Passive stretching 3. Joint mobilization 4. Dynamic splinting 5. Casting
question
Medical Treatment for Fractures: -Closed Reduction: i.e. Short Arm Cast (SAC), Long Arm Cast (LAC), Splint, Sling or Fracture Brace -ORIF: i.e. nails, screws, plates, wires -External Fixation -___1___: fusion -___2___: joint replacement
answer
1. Arthrodesis 2. Arthroplasty
question
Fracture of the distal radius with DORSAL displacement

answer
Colles' Fracture
question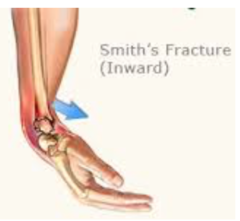
Fracture of the distal radius with VOLAR displacement
answer
Smith's Fracture
question
Carpal Fractures: -Most common is ___1___ fracture (60% of carpal fractures); This has a poor blood supply ; may become necrotic

answer
1. Scaphoid
question
Metacarpal Fractures: -Classified according to location (head, neck, shaft, base) -Common complication is rotational deformities i.e. ___1___: a fracture to the 5th Metacarpal, which requires a ___2___ splint

answer
1. Boxer's Fracture 2. Ulnar gutter
question
Proximal Phalanx Fracture: -Most common with thumb & index finger -Common complication: loss of PIP AROM/PROM
answer
:)
question
Middle phalanx fractures are not common
answer
:)
question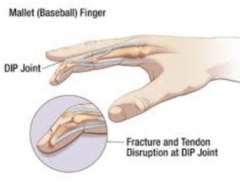
Distal Phalanx Fracture: *Most common finger fracture -May result in ___1___, which involves terminal extensor tendon
answer
1. Mallet Finger
question
Elbow Fracture: -Involvement of the radial head may result in limited rotation of the ___1___
answer
1. Forearm
question
Humerus Fractures: non displaced vs. displaced -From a fall on outstretched UE -Fractures of greater tuberosity may result in ___1___ -Humeral shaft fractures may result in ___2___
answer
1. RTC injuries 2. Radial nerve injury causing wrist drop
question
OT Eval for Fractures: -Mechanism of injury & fracture management -Results of special tests (X-rays, MRI, CT) -Edema -Pain -AROM: DO NOT ASSESS PROM UNTIL ORDERED BY PHYSICIAN; exceptions are ___1___ which usually begin with PROM before AROM**** -Sensation -Roles, occupations, ADLs/activities related to roles
answer
1. Humeral Fractures
question
OT Ix Fractures for Immobilization Phase: *Goals: stabilization & healing -___1___ of joints above & below the stabilized part -Edema control: elevation, retrograde massage, compression garments -Light ADL & role activities with NO RESISTANCE, progress as tolerated
answer
1. AROM
question
OT Ix Fractures for Mobilization Phase: *Goal: Consolidation -Edema control: elevation, retrograde massage, contrast baths, compression garments -AROM, progress to PROM when approved by physician (4-8 wks); exceptions are humeral fractures which go PROM to AROM -Light purposeful/occupation based activities -Pain management: positioning & PAM's -Strengthening: begin with isometrics when approved by physician
answer
:)
question
____1___: -Risk factors: repetition, static position, awkward postures, forceful exertions, vibration, acute trauma, pregnancy, diabetes, arthritis, wrist size/shape -Most common types: 1. de Quervain's 2. Lateral & Medial Epicondylitis 3. Trigger Finger 4. Nerve compressions
answer
1. Cumulative Trauma Disorders (CTD) AKA repetitive strain injuries (RSI), overuse syndromes or musculoskeletal d/o's
question
____1___: -Stenosing tenosynovitis of abductor pollicus longus (APL) and extensor pollicus braves (EPB) -Causes pain ; swelling over radial styloid -Positive ___2___

answer
1. de Quervain's 2. Finkelstein's Test
question
Conservative treatment for de Quervain's? (4)
answer
1. THUMB SPICA SPLINT (IP joint free) 2. Activity/work modification 3. Ice massage over radial wrist 4. Gentle AROM of wrist & thumb to prevent stiffness
question
Post-op treatment for de Quervain's? (3)
answer
1. Thumb spica splint ; gentle AROM (0-2 weeks) 2. Strengthening, ADL ; role activities (2-6 weeks) 3. Unrestricted activity (6 weeks)
question
*Degeneration of the tendon origin as a result of repetitive microtrauma -___1___: overuse of wrist EXTENSORS, especially ECRB; also called ___2___ -___3___: Overuse of wrist FLEXORS, also called ___4___
answer
1. Lateral epicondylitis (LE) 2. Tennis Elbow 3. Medial epicondylitis (MF) 4. Golfer's Elbow
question
Conservative treatment for Medial/Lateral epicondylitis? (5)
answer
1. Elbow strap, wrist splint 2. Ice & deep friction massage 3. Stretching 4. Activity/work modification 5. As pain decreases, add strengthening; begin with isometric & progress to isotonic & eccentric exercises
question
___1___: tenosynovitis of the finger FLEXORS; most commonly the ___2___ -Caused by repetition and the use of tools that are too far apart
answer
1. Trigger Finger 2. A1 pulley
question
Conservative treatment for Trigger Finger? (5)
answer
1. HAND based TRIGGER FINGER SPLINT (MCP extended, IP free) 2. Scar massage 3. Edema control 4. Tendon gliding 5. Activity/work modification: avoid repetitive gripping activities & using tools with handles too far apart
question
Tendon Repairs: Rationale for Early Mobilization: -Prevents adhesion formation -Facilitates wound/tendon healing Occupational Therapy Goals: -Increase tendon excursion -Improve strength at repair site -Increase joint ROM -Prevent adhesions -Facilitate resumption of meaningful roles, activities & occupations
answer
:)
question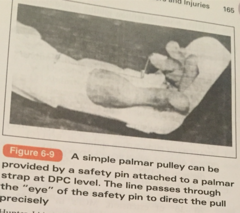
Early Mobilization Protocols for Flexor Tendons: ___1___: Passive flexion using rubber band traction & active extension to the hood of the splint
answer
1. Kleinert Protocol
question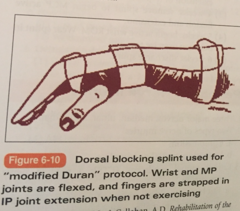
Early Mobilization Protocols for Flexor Tendons: ___1___: Passive flexion & extension of digit
answer
1. Duran Protocol
question
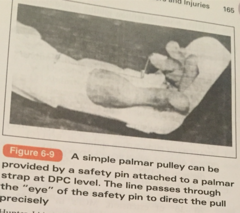
0-4 weeks (early phase): DORSAL BLOCK SPLINT -Wrist positioned in 20-30 degrees flexion -MCP its in 50-60 degrees flexion -IP joints extended -Passive flexion & active extension w/i limits of splint 4-7 weeks (intermediate phase): Continue DORSAL BLOCK SPLINT, but adjust wrist to neutral -Place/hold exercises and differential flexor tendon gliding exercises. Scar management. 6-8 weeks: AROM -Differential tendon gliding -Light purposeful & occupation based activities -D/C SPLINT 8-12 weeks: Strengthening & work/leisure activities
answer
Kleinert Protocol for Flexor Tendon Repairs
question
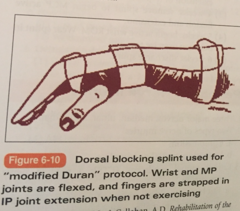
0-4.5 weeks: DORSAL BLOCKING SPLINT -Exercises in splint include passive flexion of PIP joint, DIP joint & DCP joint, 10 reps every hour 4.5-6 weeks: active flexion & extension within limits of splint 6-8 weeks: -Tendon gliding & differential tendon gliding -Scar management -Light & purposeful & occupation based activities 8-12 weeks: strengthening & work activities
answer
Duran Protocol for Flexor Tendon Repairs
question
Early Mobilization Programs for Extensor Tendons: Zone I & II: -Mallet Finger Deformity: ____1____ splint (0-6 weeks)
answer
1. DIP Extension Splint
question
Early Mobilization Programs for Extensor Tendons: Zone III & IV: -Boutinniere Deformity: 0-4 wks: ___1___ splint; AROM of DIP while in splint 4-6 wks: begin AROM DIP & flexion of digits to the DPC
answer
1. PIP Extension Splint (DIP free)
question
Early Mobilization Programs for Extensor Tendons: Zone V, VI & VII: 0-2 wks: ___1___ splint 2-3 wks: Shorten splint to allow flexion & extension of IPs 4 wks: Remove splint & begin MCP active flexion & extension 5 wks: begin wrist AROM; wear splint in between exercise sessions 6 wks: D/C splint
answer
1. Volar Wrist Splint -20-30 degrees extension -MCPs in 0-10 deg flexion -IP's in full extension
question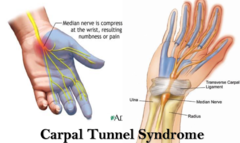
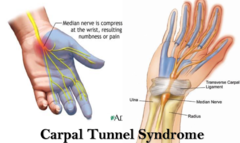
___1___: -Median nerve compression -Cause: repetition, awkward postures, vibration, anatomical anomalies, pregnancy -Symptoms: numbness ; tungling go the thumb, index, middle ; radial half of ring fingers: Paresthesias usually OCCUR AT NIGHT* (most characteristic sx) -Positive ___2-3___ signs *Advanced stage can result in muscle atrophy of the thenar eminance
answer
1. Carpal Tunnel Syndrome (CTS) 2. Tinel's sign 3. Phalen's sign
question
Conservative Tx of CTS? (4)
answer
1. Wrist splint in neutral: should be worn at night ; during the day if performing repetitive activity 2, Median nerve gliding exercises ; differential tendon gliding exercises 3. Activity modification: avoid activities of wrist flexion, wrist flexion w/ repetitive finger flexion, wrist flexion w/ static grip 4. Ergonomics: appropriate workstation design; CTS most common work related injury of UE
question
Surgical Ix for CTS?
answer
Carpal Tunnel Release (CTR)
question
Post-op Tx after CTR for CTS? (6)
answer
1. Edema control: elevation, retrograde massage, compression glove, contrast bath 2. AROM 3. Nerve ; tendon gliding exercise 4. Sensory reeducation 5. Strengthening of thenar muscles (usually 6 wks post op) 6. Work/activity modification
question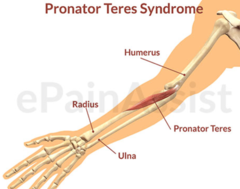
___1___: median nerve compression between two heads of pronator teres -Cause: repetitive pronation ; supination ; excessive pressure on VOLAR forearm -Sxs: same as CTS ; also pain in proximal forearm, but NO NIGHT SXS (daytime only) -Positive ___2___ sign
answer
1. Pronator Teres Syndrome (proximal volar forearm) 2. Tinel's
question
Conservative Tx for Pronator Teres Syndrome? (2)
answer
1. Elbow splint at 90 degrees with forearm in neutral 2. Avoid activities that include repetitive forearm pronation & supination
question
Surgical Ix for Pronator Teres Syndrome?
answer
Decompression
question
Post-op Decompression for Pronator Teres Syndrome? (5)
answer
1. AROM 2. Nerve gliding 3. Strengthening (2 wks post-op) 4. sensory reeducation 5. Work/activity modification
question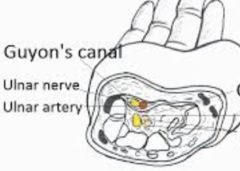
____1____: ulnar nerve compression at the wrist Cause: repetition, ganglion, pressure, fascia thickening Symptoms: -Numbness & tingling in ulnar nerve distribution of hand -Motor weakness of ulnar nerve-innervated musculature -Positive ____2___ sign at the canal (AKA ulnar canal) -Advanced stages can lead to muscle atrophy of ulnar-innervated musculature of hand
answer
1. Guyon's Canal 2. Tinel's sign
question
Conservative Tx of Guyon's Canal? (2)
answer
1. Wrist splint in neutral 2. Work/activity modification
question
Surgical Ix for Guyon's Canal?
answer
Decompression
question
Postop decompression for Guyon's Canal? (5)
answer
1. Edema control 2. AROM 3. Nerve gliding 4. Strengthening at 2-4 wks: FOCUS ON POWER GRIP 5. Sensory reeducation
question
___1___: ulnar nerve compression at the elbow Cause: second most common compression; compression at elbow (leaning on elbow) ; extreme elbow flexion Sis: numbness ; tingling along ulnar aspects of forearm ; hand -Pain in elbow w/ extreme position of the elbow -Weakness of power grip -Positive ___2___ sign at elbow -Advanced stages can lead to atrophy of FCU, FDP to digits IV and V and ulnar nerve innervated muscles of the hand
answer
1. Cubital Tunnel Syndrome 2. Tinel's
question
Conservative Tx for Cubital Tunnel Syndrome? (3)
answer
1. Elbow splint to prevent positions of extreme flexion (especially at night) 2. Elbow pad to decrease compression of nerve when leaning on elbows 3. Work/activity modification
question
Surgical intervention for Cubital Tunnel Syndrome?
answer
Decompression OR transposition
question
Postop Decompression OR transposition for Cubital Tunnel Syndrome? (5)
answer
1. Edema control 2. Scar management 3. AROM & nerve gliding (2 wks postop) 4. Strengthening (4 wks post op) 5. MCP flexion splint if clawing noted
question
___1___: radial nerve compression Cause: Saturday night palsy, a term used to describe sleeping in a position that places stress on radial nerve; also compression of humeral shaft fracture Symptoms: weakness or paralysis of extensors to the wrist, MCPs, thumb & wrist drop
answer
1. Radial Nerve Palsy
question
Conservative Treatment Radial Nerve Palsy? (3)
answer
1. Dynamic Extension Splint 2. Work/activity modification 3. Strengthening wrist & finger extensors when motor function returns
question
Surgical Intervention for Radial Nerve Palsy?
answer
Decompression
question
Post-op Tx for Radial Nerve Plays? (4)
answer
1. ROM 2. Nerve gliding 3. Strengthening (6-8 wks post op) 4. ADL & meaningful role activities
question
Median Nerve Laceration: Sensory Loss? (3)
answer
1. Central palm (thumb to radial half of finger) 2. Palmar surface of thumb, index, middle and radial half of ring fingers 3. Dorsal surface of thumb, index, middle and radial half of ring fingers (middle & distal phalanges)
question
Median Nerve Laceration: Motor Loss for LOW LESION at WRIST? (4)
answer
1. Lumbricals I & II (MCP flexion of digits II & III 2. Opponens Pollicus (opposition) 3. APB (abduction) 4. FPB (flexion of thumb MCP)
question
Median Nerve Laceration: Motor Loss for HIGH LESION at or proximal to the ELBOW? (6)
answer
1. Lumbricals I & II (MCP flexion of digits II & III 2. Opponens Pollicus (opposition) 3. APB (abduction) 4. FPB (flexion of thumb MCP) 5. FDP to index & middle fingers, FPL (Flexion of top of index, middle fingers & thumb) 6. FCR (inability to flex at radial aspect of wrist)
question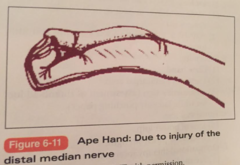
Deformity of Median Nerve Laceration?
answer
1. Flattening of Thenar Eminence (APE HAND) 2. Clawing of index & middle gingers for a low lesion 3. Benediction Sign for high lesion
question
Functional Loss with Median Nerve Laceration? (2)
answer
1. Loss of thumb opposition 2. Weak pinch
question
-Dorsal protection splint: Low lesion: wrist positioned in 30 degrees of flexion High lesion: include elbow at 90 degrees of flexion -Begin AROM/PROM of digits its wrist in FLEXED position at 2 wks post op -Scar management -AROM at 4 wks & include elbow if high lesion -Strengthening at 9 wks *Begin sensory reeducation when the individual demos a level of diminished protective sensation on the Semmes-Weinstein****
answer
OT Ix for MEDIAN & ULNAR Nerve Laceration
question
Splinting Considerations for Median Nerve Laceration?
answer
C-bar prevent thumb adduction contracture
question
Ulnar Nerve Laceration: Sensory Loss? (2)
answer
1. Ulnar aspects of palmar & dorsal surfaces 2. Ulnar half of ring finger & little fingers on palmar & dorsal surfaces
question
Ulnar Nerve Laceration: Motor Loss?
answer
See p. 168 b. & c. in TE!
question
Ulnar Nerve Laceration: Deformity? (3)
answer
1. Claw hand 2. Flattened metacarpal arch 3. Positive for Forment's sign (assessment of thumb adductor while laterally pinching paper)
question
Ulnar Nerve Laceration: Functional loss? (2)
answer
1. Loss of power grip 2. Decreased pinch strength
question
Splint Consideration for Ulnar Nerve Laceration?
answer
MCP Flexion Block Splint
question
Radial Nerve Laceration: Sensory Loss? (3)
answer
1. High lesions at the level of the humerus 2. Medial aspect of dorsal forearm 3. Radial aspect of dorsal palm, thumb, index, middle ; radial half of ring phalanges
question
Radial Nerve Laceration: Motor Loss see p. 168 TE!
answer
:)
question
Radial Nerve Laceration: Functional Loss? (2)
answer
1. Inability to extend digits to release objects 2. Difficulty manipulating objects
question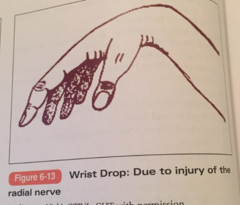
Radial Nerve Laceration: Deformity?
answer
Wrist Drop
question
OT Ix Radial Nerve Laceration? (5)
answer
1. DYNAMIC EXTENSION SPLINT 2. ROM 3. Sensory reeducation if needed 4. Instruct a home program 5. Activity modification
question
___1___: Cause: -Repetitive overuse -Curved/hooked acromion -Weakness of RTC -Weakness of scapula musculature -Ligament ; capsule tightness -Trauma
answer
1. RTC Tendonitis
question
-Activity mod: avoid above the shoulder level activities until pain subsides -Educate on sleeping posture: avoid sleeping with arm overhead or combined adduction ; IR -Decrease pain: positioning, modalities, rest -Restore pain free ROM -Strengthening: below shoulder level -Occupation/role specific training
answer
RTC Tendonitis: OT Conservative Tx
question
-Arthroscopic sx -Open repair: small, medium, large ; massive tears
answer
RTC Tendonitis Sx Ix's
question
OT Postop Ix for RTC Tendonitis?
answer
-PROM (0-6); Progress to AAROM to AROM***** -Decrease pain: begin with ice, progress to heat -Strengthening (6 wks post-op): begin with isometrics, progress to isotonic (below shoulder level) -Activity modification: light ADL & meaningful role activities; progress as tolerated -Leisure & work activities
question
___1___: restricted PROM of shoulder -Greatest limitation is ER, then abduction, IR & flexion -Anatomy: GH ligaments & joint capsule Cause: Inflammation & immobility; linked to DM & PD
answer
1. Adhesive Capsulitis (AKA Frozen Shoulder)
question
OT Conservative Ix Adhesive Capsulitis (AKA Frozen Shoulder): -Encourage active use through ADL & role activities -PROM -Modalities
answer
:)
question
Adhesive Capsulitis (AKA Frozen Shoulder) Sx Ix?
answer
Arthroscopic Sx & manipulation
question
Adhesive Capsulitis (AKA Frozen Shoulder): OT postop Ix? (3)
answer
1. PROM immediately after sx 2. Pain relief: modalities 3. Encourage use of extremity for all ADL & role activities
question
Shoulder Dislocation: Cause: Trauma & repetitive overuse -Anterior dislocation most common OT Ix: -Regain ROM: avoid combined ___1-2___ with anterior dislocation -Pain free ADL & role activities -Strengthen RTC
answer
1. Abduction 2. ER
question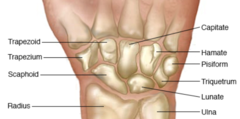
Carpal bones
answer
Distal Row: hamate, capitate, trapezoid & trapezoid Proximal row: Pisiform, lunate, triquetrum & scaphoid
question
proper use of the circumferential proximal interphalangeal (PIP) joint orthosis for boutonniere deformity?
answer
Wear orthosis continuously up to 6 weeks (Continuous use of PIP joint extension splint allows the central slip to reestablish continuity & prevents further flexion deformity)
question
A client with a chronic median nerve compression at the carpal tunnel has severely diminished functional pinch. In what position should the thumb be splinted to facilitate functional pinch?
answer
OPPOSITION & PALMAR ABDUCTION
question
1. An OTR® is treating a client with a proximal interphalangeal (PIP) flexion contracture secondary to a sports injury. To improve extension of the PIP for functional use of the hand, what is the BEST use of limited therapy time?
answer
A. Fit the client with a prefabricated dynamic PIP extension assist splint (This will improve PIP extension LT & takes LESS therapy time to fit than making a custom splint)
question
What do flexion blocking exercises do?
answer
INCREASE FLEXION (NOT extension...)
question
Angle of pull for dynamic splint
answer
90 degrees
question
An OTR® is working in the burn unit of a hospital. A client has undergone skin grafting to close wounds on the dorsum of the hand. What occupational therapy treatment is MOST appropriate for the 5 to 7 days post skin graft?
answer
a. Fabricate & splint patient with safe position splint over dressings (This allows the graft to take & wound to heal & prevents deformities) *Once the skin has been grafted, the wrist and hand should be protected for 5 to 7 days until the staples are removed. No AROM, PROM, or functional use of the hand should occur during this time.
question
An OTR is working with a client who has a flexor tendon injury. The referring physician prefers patients to follow the flexor tendon protocol using controlled passive motion. Which movement is indicated?
answer
A. Passive extension of the distal interphalangeal joint if the metacarpal and proximal phalangeal joints are flexed (The DIP & PIP joints can be passively EXTENDED if other joints of the digits are FLEXED to initiate TENDON GLIDING & PREVENT SCARRING of tendon)
question
With which type of client would it be best practice to allow the proximal interphalangeal (PIP) joints to develop a contracture to facilitate functional grasp?
answer
C6 SCI Ranging the hand (wrist extension combined with finger flexion and wrist flexion combined with finger extension) of a client with a spinal cord injury preserves a functional tenodesis grasp while encouraging PIP flexion contractures.
question
11. An OTR® is treating a client with wrist tendinitis secondary to computer use. Before educating the client on wrist positions to avoid, the OTR® has applied iontophoresis to the affected area. Which medication would the OTR® be MOST likely to use with the iontophoresis?
answer
a. Dexamethasone (This is the most widely used medication by therapists using iontophoresis because of its anti-inflammatory properties)
question
11. An OTR® is treating a client with decreased digital range of motion and minimal subacute edema of the same hand. After ascertaining that there are no contraindications to modality use, which preparatory method is the BEST choice for before therapeutic activities?
answer
a. Mild, superficial heating application to hand & digits (Heating between 71.6-105.8 deg F increases lymph flow & helps soften tissues to promote incr ROM; heating does NOT exacerbate minimal edema)
question
Flexor Tendon Zones?

answer
a. Zone I (This contains flexor digitorum profundus tendon) b.Zone II (This contains the tendon sheath covering FDP & FDS) c. Zone III (This is the lumbrical muscle zone) d. Zone IV & V (Zone IV (Carpal Tunnel Region) consists of transverse carpal ligament & median nerve runs UNDER ligament; Zone V (Forearm Region) is distal to this ligament & contains the median nerve branch)
question
11. When planning a sensory reeducation program for a client with sensory loss associated with peripheral nerve damage, which intervention would the OTR® use FIRST?
answer
Protective sensory reeducation because the client is at risk for injuring the insensate hand
question
Sensation misinterpreted as pain
answer
Allodynia
question
Increased response to painful stimuli
answer
Hyperalgia
question
Pain that continues after stimulus is removed
answer
Hyperpathia
question
11. An OTR® is fabricating an orthotic for a client with radial nerve palsy (Causes wrist drop). Which orthotic design is appropriate to improve function?
answer
A. Forearm-based wrist orthotic that maintains the wrist in 30° of extension (This allows client to extend fingers for object release using intrinsic hand muscles; less costly than a dynamic orthesis) Wrong answers: A. Forearm-based radial thumb spica that supports the lateral aspect of the wrist and hand (This does not offer full wrist support to prevent overstretch of forearm extensors*) C. Anticlaw orthosis (This is for ULNAR NERVE PALSY, to prevent MCP hyperextension) D. Hand-based short thumb spica (This does not support wrist in a functional position)
question
11. An OTR® is treating a client who sustained dorsal hand burns secondary to a work-related injury. In the intensive care unit phase of treatment, which technique for completing ROM of the hand is safest?
answer
a. Passively range all digits one at a time (This DECREASES chances of rupturing finger extensor tendons with dorsal hand burns) *(AROM/PROM of more than one digit at a time increases chances of rupturing finger extensor tendons to the dorsal hand)
question
11. An OTR® is educating a client about what to expect in the process of wound healing after surgery. What are the expected phases of wound healing in the order they occur?
answer
Inflammation (clotting, vasoconstriction, WBC migration) Proliferation (collagen (epithelialization & tissue granulation) Remodeling (scar tissue remodeling)
question
11. A high-level ulnar nerve injury (AKA claw hand deformity) may result in which characteristic deformity?
answer
A. Hyperextension of the ring and small finger MCP joints because of loss of the extension-controlling forces of the third and fourth lumbricals (The third and fourth lumbricals are innervated by the ulnar nerve. Loss of motor function in these muscles allows the extensor digitorum communis to extend the MCP joints without any opposing controlling forces, also known as "claw hand" deformity.)
question
This is result of ulnar nerve injury & hyperextension of MCP in digit IV and V with PIP flexion

answer
Ulnar claw ("Claw Hand" Deformity)
question
11. An OTR is working with a client who has decreased nerve function. The client has lost precision pinch, thenar opposition, and the ability to bend the index and long fingers at the proximal and distal interphalangeal joints. What deformity is the client MOST likely to have?
answer
Ape hand deformity
question
11. An OTR® who is a certified hand therapist is responsible for supervising a new COTA® in an outpatient hand clinic. What is the purpose of the supervisory process, as defined by AOTA?
answer
As stated in the Guidelines for Supervision, Roles, and Responsibilities During the Delivery of Occupational Therapy Services (AOTA, 2014), "Within the scope of occupational therapy practice, supervision is a process aimed at ensuring the safe and effective delivery of occupational therapy services and fostering professional competence and development" (p. S16).
question
11. An OTR® is working with a client who fractured the distal radius 6 weeks ago. Within what time frame can controlled AROM be initiated if the fracture is healing secondarily?
answer
3-6 weeks postop (Controlled AROM can be initiated during this time if the fixation of the fracture is adequate)
question
Over time, diminished blood flow to a peripheral nerve can result in serial impingements AKA?
answer
double crush syndrome
question
In the realm of nerve healing and testing, the order in which recovery occurs is?
answer
one-point moving, one-point discrimination, two-point moving, and finally two-point discrimination
question
11. An OTR® fabricated a thermoplastic splint for a client with carpometacarpal (CMC) osteoarthritis to support the CMC joint. The client is unable to wear it during work hours because some movement of the joint is required to complete tasks. Which positioning device would BEST suit this client's needs?
answer
a. CMC neoprene wrap support (This provides less support, but allows for some movement)
question
11. Which outpatient treatment intervention is contraindicated for decreasing the arm edema and stiffness associated with complex regional pain syndrome of the upper extremity?
answer
A. Provision of an arm sling to wear during the day (This will increase stiffness ; edema bc it places the extremity in dependent ; static positions for long periods of time) What is GOOD- A. Instruction in the use of contrast baths several times a day (This is a benefit for CRPS) B. Instruction in performing gentle, pain-free AROM movements several times a day (Gentle, pain-free AROM encourages circulation, decreases stiffness, and may assist in interrupting the pain cycle.) D. Provision of a compression garment to wear during the day (This would benefit CRPS)
question
11. An OTR is working with a client who presents with digital tenosynovitis in the index finger, or "trigger finger." After the OTR fabricates a splint to support the metacarpophalangeal joint in extension, which exercise should the OTR advise the client to perform FIRST?
answer
a. Hook fist with splint on *Trigger finger is a condition in which edema in the tendon and synovium of the digit results in lack of smooth flexion or extension of the finger. To rest the tendon and prevent snapping as the tendon pulls through the finger pulleys, the MCP joint is blocked by splinting, then gentle pull through with bending and straightening of the distal and proximal interphalangeal joints is recommended *20 times every 2 hours* while the client is awake.
question
A blocking splint fabricated to maintain the metacarpophalangeal (MCP) joints in extension can be useful to isolate which joint movements?
answer
A. IP joint flexion and FDP excursion (MCP joint extension helps isolate PIP ; DIP joint flexion ; isolate FDP excursion)
question
11. An OTR® assigned to the stroke unit of an acute care hospital is prioritizing goals and treatment for a patient with a hemiplegic hand. Based on the expected pattern of progression in the acute phase after a stroke, which areas of focus should the OTR consider to enable the patient to overcome barriers to ADL performance?
answer
PROM, positioning of affected UE ; bed mobility
question
11. An OTR is working with a client with a flexor tendon injury. One week after repair surgery, the OTR removes the cast made postsurgery and fabricates a splint. Which splint is appropriate for this client?
answer
Dorsal blocking hand splint *This will protect the surgery ; guard against flexor tendon rupture (because if over extend, can rupture newly fixed flexor tendon) Wrong answers: a. Active wrist extension splint (This is for an extensor tendon injury) b. Active wrist, finger ; thumb extension splint (This is for an extensor tendon injury) c. Resting hand splint (This is for positioning to prevent deformities i.e. RA)
question
11. A client sustained a nondisplaced humeral neck fracture (normal bone alignment maintained) after a fall. Which course of occupational therapy would be BEST?
answer
Sling with supervised ROM
question
11. An OTR is seeing a client in the upper extremity outpatient clinic. During the initial assessment, the client describes an area extending from the radial head to the proximal aspect of the supinator muscle as having a dull ache and burning sensation. Which syndrome is the client describing?
answer
a. Radial tunnel syndrome (Burning sensation in this area caused by compression of RADIAL nerve)
question
11. An OTR® in an outpatient setting is treating a client who underwent repair of multiple flexor tendons in Zones 2 and 3 approximately 6 weeks ago. The dorsal blocking splint has been removed, and the client is beginning to actively move the digits. The client is eager to return to work as a carpenter, and the OTR is revising the goals with the client. Which goal for this time period is MOST appropriate?
answer
a. Increase digital AROM to facilitate holding a washcloth for bathing (Setting realistic, meaningful goals and revising them as the client progresses is a critical component in treating traumatic injuries. At 6 weeks after operative tendon repair, the client may be ready for light, nonresistive functional activities that promote active flexion.) Wrong answers: a. Increase passive wrist ; digit composite extension to improve flexor tendon length (Adding too much F at this stage may rupture repairs) a. Increase grip strength to maintain grasp on woodworking tools (Strengthening is contraindicated at 6 weeks; not okayed until 10-12 weeks) b. String 25 beads of various sizes ; shapes to improve FMC (This has no functional component or intrinsic value to the client)
question
11. An OTR is advising a client who has had a flexor tendon repair on the timing for resuming ADLs. During what time period is the flexor tendon repair the weakest and most likely to rupture?
answer
a. 10-12 days post surgery (A tendon repair is typically at its weakest 10-12 days postsurgery during the fibroplasia phase, in which collagen is just beginning to be laid down to strengthen the repair.) Wrong answers: a. 1-3 days post surgery (The tendon is still newly repaired and has the strength of the original suture.) b. 7-9 days post surgery (The tendon is still newly repaired and has the strength of the original suture.) a. 4-8 weeks post surgery (This is considered the intermediate phase, during which the tendon gains strength.)
question
11. A client is being treated for an extensor tendon repair in Zone VI of the middle finger proximal to the juncturae tendinum. Which orthosis would be MOST appropriate?
answer
A. Forearm based, including the middle, ring, and index fingers (It is important to consider adjacent digits when applying an orthosis. In this example, the injury falls proximal to the juncturae tendinum, which can apply force to the repaired site if the adjacent digits were to flex, thus compromising the repair.) Wrong answers: A. Hand based, including only the middle finger (Hand-based splints would not protect tendon repair unless the wrist were immobile as well) B. Forearm based, including only the middle finger (Adjacent digits need to be included in the splint because flexion of adjacent digits can apply too much force to the tendon repair, resulting in a possible rupture.) C. Hand based, including the middle, ring, and index fingers (Hand-based splints would not protect tendon repair unless the wrist were immobile as well)
question
11. An OTR® is treating a client with a cumulative trauma disorder resulting from work in an automotive assembly plant. Acute symptoms have subsided, and the client is preparing to return to work. Which strategies should the OTR® train the client in to prevent symptoms from recurring?
answer
A. Activity modification and proper body mechanics (Activity modification and proper body mechanics are essential for long-term control of an inflammatory cumulative trauma disorder.) (Joint protection ; pacing techniques addresses arthritis!)
question
This is used to treat trigger points ; increase PROM
answer
Cold spray (PAM)
question
facilitates muscle contraction
answer
NMES
question
best PAM for pain control
answer
TENS
question
This is used to control inflammatory conditions
answer
Iontophoresis
question
An OTR is working with a client who jammed the distal interphalangeal (DIP) joint of the long finger while playing basketball. The terminal tendon was avulsed, so the client was diagnosed with mallet finger. Which occupational therapy intervention is appropriate to use FIRST with this client?
answer
Splint DIP in extension continuously for 6 weeks *DIP is delicate and requires 6 weeks of continuous splint extension to prevent extensor lag of the tendon
question
11. During an assessment, an OTR asks the client to pinch a pinch gauge and notices increased flexion of the thumb interphalangeal joint. What term is used to describe this type of pinch?
answer
a. Froment's Sign (This occurs when then FPL compensates for a weak/paralyzed adductor pollicus & flexor pollicus brevis; when client attempts to pinch, IP joint of the thumb flexes more than usual; signs for CUBITAL TUNNEL & CLAW DEFORMITY (ulnar nerve))
question
This is when 5th digit is abducted from 4th digit
answer
Wartenberg's sign Sign for: CUBITAL TUNNEL ; CLAW DEFORMITY (ulnar nerve)
question
This is hyperextension of the proximal phalanx of the thumb
answer
Jeanne's Sign Sign for: claw deformity (ulnar nerve)
question
11. An OTR is working with a client with lateral epicondylitis. What is the BEST client education the OTR can offer in terms of wearing a splint for this condition?
answer
A. To wear the splint during any activity that causes pain (The splint rests the muscle & tendon & protects against pain with activity) Wrong answers: A. To wear the splint only at night so that it does not interfere with the client's daily activities (Wearing a splint at night is appropriate for CARPAL TUNNEL syndrome, not lateral epicondylitis) B. To wear the splint 24 hours a day without removing it for any reason until the next occupational therapy appointment (Wearing a splint continuously decreased blood flow and O2 to tissues) C. To not wear the splint unless the client feels pain (The splint needs to be worn during activities that cause pain, not after the pain begins)
question
11. A client with a nondisplaced shaft fracture of the right fifth metacarpal has a physician's order for full-time splinting. Which orthosis would the OTR® be MOST likely to fabricate?
answer
A. Volar-based ulnar gutter with MCP joints of the ring and fifth fingers in 70°-90° flexion, fourth and fifth IP joints in 0° extension, and the wrist in approximately 20° extension (Holding MCP joints in flexion with metacarpal fracture helps prevent contracture of collateral ligaments) *Maintain MCP in extension may lead to collateral ligament shortening & decreased ability to flex MCP joint after fracture is healed so BAD
question
Can't EXTEND DIP joint (may do it passively though)
answer
Mallet finger Splint in slight hyperextension to heal extensor tendon injury
question
11. An OTR is evaluating a client with a brachial plexus injury. When checking upper-extremity movement patterns, what is the GREATEST degree of abduction the OTR should allow on the affected side?
answer
90 degrees
question
11. A 10-year-old child sustained a Zone 2 flexor digitorum profundus tendon laceration and underwent primary repair. Which flexor tendon repair protocol represents best practice standards?
answer
a. Immobilization (Children younger than 12 are placed on immobilization protocol because of their low maturity level ; low ability to comply with exercises/precautions of their protocols)
question
Frozen shoulder Patients experience pain, limited range of motion, and disability
answer
Primary adhesive capsulitis
question
11. An OTR® is treating a client with a nondisplaced radial head fracture and is following the referring physician's order for an immediate mobilization protocol. In which position would the client BEST tolerate early elbow flexion and extension?
answer
A. Supine with the upper arm supported on a folded towel along the torso (Positioning in supine with the upper arm supported on a folded towel along the torso facilitates gravity-assisted motion of the elbow with support to the affected extremity. Gravity-assisted motion allows for early, nonresistive motion of a stable fracture, which can promote bone healing.)
question
11. A client fell while skiing downhill and sustained a Type III fracture of the radial head. Which treatment would be MOST appropriate for this type of fracture?
answer
Fragment excision with a long arm cast for 3-4 weeks (A Type III fracture of the radial head requires removal of the fragmented bone and a cast for 3-4 weeks to ensure proper healing and support.) (Splint would NOT be sufficient enough for type III fracture; need a cast!)
question
11. An OTR is working with a child who has an epiphyseal fracture of the proximal interphalangeal bone with slight malalignment. Which intervention is MOST appropriate for a child with this condition?
answer
A. Buddy tape the finger to an adjacent finger (The least invasive and most effective treatment for a slight malalignment is buddy taping, and this is the intervention the child would be most likely to tolerate.) Wrong answers: A. Do nothing; the child's fracture will heal and no occupational therapy is required (Because it is an epiphyseal fracture, it is important to realign the bone for future growth.) B. Fabricate a serial cast for the child's finger (Serial cast is generally unnecessary for slight malalignment secondary to fracture and may not be well tolerated by children.) C. Fabricate a dynamic splint for the child's finger (Dynamic splint is generally unnecessary for slight malalignment secondary to fracture and may not be well tolerated by children.)



