Chapter 8: Cancers of the Female Reproductive Tract – Flashcards
Unlock all answers in this set
Unlock answersquestion
Cancer
answer
-Second leading cause of death for women in the United States, surpassed only by cardiovascular disease, many women between the ages of 35 and 74 are developing and dying of cancer. African American women have the highest death rates for both heart disease and cancer. -Certain cancers are related to infectious agents, such as hepatitis B virus (HBV), human papillomavirus (HPV), human immunodeficiency virus (HIV), and Helicobacter pylori (H. pylori), and can be prevented through behavioral changes, vaccines, or antibiotics. -Nurses need to focus their energies on screening, education, and early detection to reduce these numbers. Cancer risk is strongly associated with lifestyle and behavior, screening programs are of par- ticular importance for early detection.
question
Reproductive Tract Cancer
answer
-Two primary needs arise: information and emotional support -Nurses working with women following a cancer diagnosis include assessing women's definitions and availability of support; respecting varied needs for informational support; providing a supportive clinical environment; educating clinicians, family, and friends regarding unsupportive responses within the cultural context; and validating women's control and balancing of support needs
question
Assessment
answer
-Involves a thorough history and physical examination. In addition, various lab and diagnostic tests may be done to evaluate for a malignancy. -HX: Determine any current or past factors that might increase her risk of cancer, such as early menarche, late menopause, STIs, use of hormonal agents, or infertility. Find out if the woman has a family history of cancer. Be thorough in obtaining the woman's past medical history, especially her reproductive, obstetric, and gynecologic history. Ask about her lifestyle and behaviors, including risky behaviors such as engaging in unprotected sexual intercourse or sexual intercourse with multiple partners -Any symptoms, such as abnormal vaginal bleeding or discharge or vaginal discomfort. Often the symptoms of cancer are vague and nonspecific and the woman may attribute them to another problem, such as aging, stress, or improper diet.
question
Labs and DX Testing (common)
answer
-Clinical breast exam: identifies palpable mass, skin change, inverted nipple or unresolved rash -Mammography: detects calcifications, densities, and nonpalpable cancer lesions -Pap smear: aids in detecting abnormal cells of the cervix -Transvaginal US: measurement of endometrial thickness to determine if endometrial biopsy is needed for postmenomausal bleeding - CA-125: elevation of marker suggests malignancy but is not specific to ovarian cancer
question
Educating to prevent cancer
answer
-Nurses need to provide clients with information to help prevent disease and enhance quality of life. Educate women about the importance of consistent and timely screenings to identify cancer early. Emphasize the importance of having an annual pelvic examination. Stress the need for follow-up screenings as recommended. Provide clients with information if further di- agnostic testing is needed
question
Reducing risk for cancer
answer
- Don't smoke - Drink alcohol only in moderation (no more than one drink daily) - Be physically active -Healthy diet -Current with immunizations. -Condom with every sexual encounter -Maintain a healthy weight. -Preventive medicines if needed. -Recommended screening tests: -Body mass index (BMI) to identify obesity -Mammogram every 1 to 2 years starting at age 40 -Pap smear every 1 to 3 years if sexually active, be- tween the ages of 21 and 65 -Cholesterol checked annually starting at age 45 -Blood pressure checked at least every 2 years -Diabetes test if hypertensive or hypercholesterolemic -Check for STIs if sexually active
question
Ovarian Cancer
answer
-Malignant neoplastic growth of the ovary -9th most common cancer, risk is 1 in 71 -Mainly develops in older women, about 1/2 are over 60. More common in caucasian women -Ovarian cancer,cause is unknown, can originate from different cell types. Most ovarian cancers originate in the ovarian epithelium. Usually present as solid masses that have spread beyond the ovary and seeded into the peritoneum prior to diagnosis
question
Screening and Dx of Ovarian Cancer
answer
-75 percent of ovarian cancers are not diagnosed until the cancer has advanced to stage III or IV, because there is still no adequate screening test. -Two genes, BRCA1 and BRCA2, are linked with hereditary breast and ovarian cancers. Blood tests can be performed to assess DNA in white blood cells to detect mutations in the BRCA genes. -These genetic markers do not predict whether the person will develop cancer. Rather, they pro- vide information regarding the risk of developing cancer: a woman who is BRCA positive may have up to an 80% chance of developing breast cancer and a 40% chance of developing ovarian cancer
question
Risk factors for Ovarian Cancer
answer
- Nulliparity - Early menarche (before 12 years old) - Late menopause (after 55 years old) - Increasing age (over 50 years of age) - High-fat diet - Obesity - Persistent ovulation over time - First-degree relative with ovarian cancer - Use of perineal talcum powder or hygiene sprays - Older than 30 years at first pregnancy - Positive BRCA1 and BRCA2 mutations - Personal history of breast, bladder, or colon cancer - Hormone replacement therapy for more than 10 years • Infertility
question
Educating the client
answer
-Promote early detection!! -Education is a major focus of nursing care. Teaching involves risk reduction and health promotion. Teach the woman about risk reduction strategies; for instance, pregnancy, use of oral contraceptives, and breastfeeding reduce the risk of ovarian cancer. -Instruct women to avoid using talc and hygiene sprays on their genitals. Review the lifetime risks related to BRCA1 and BRCA2 genes and options available should the woman test positive for these genes. Help to promote community awareness of ovarian cancer by educating the public about risk-reducing behaviors. -Instruct the woman about the importance of healthy lifestyles. Stress the importance of maintaining a healthy weight to reduce risk. Encourage women to eat a low-fat diet.
question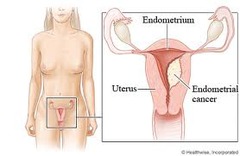
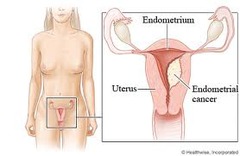
Endometrial Cancer
answer
-also known as uterine cancer; is a malignant neoplastic growth of the uterine lining -4th most common gynecologic malignancy, uncommon before the age of 40, as women age their risk for this type of cancer increases -Two mechanisms are believed to be involved in the development of endometrial cancer. A history of exposure to unopposed estrogen is the cause in 75% of women. -Those that are spontaneous and are unrelated to estrogen or endometrial hyperplasia represent the other 25% of endometrial cancers -Endometrial cancer may originate in a polyp or in a diffuse multifocal pattern. Metastatic spread occurs in a characteristic pattern and most commonly involves the lungs, inguinal and supraclavicular nodes, liver, bones, brain, and vagina -Early tumor growth is characterized by friable and spontaneous bleeding. Later tumor growth is characterized by myometrial invasion and growth toward the cervix -Adenocarcinoma of the endometrium is typically preceded by hyperplasia. Carcinoma in situ is found only on the endometrial surface. Type I carcinomas, the most common, begin as endometrial hyperplasia and progress to carcinomas -Type II carcinomas appear spontaneously, are associated with a poorly differentiated cell type, and have a poor prog- nosis. They account for less than 10% of all endometrial cancers but contribute to the majority of all endometrial deaths
question
Screening and Dx of Endometrial Cancer
answer
-not routinely done because it is not practical or cost effective -recommends that women be informed about the risks and symptoms of endometrial cancer at the onset of menopause and strongly encouraged to report any unexpected bleeding or spotting to their health care provide -Ultrasound can reliably exclude cancer without the need for biopsy in some women with postmenopausal bleeding. In particular, numerous studies have shown that women with an endometrial thickness of 4 mm or less have an extremely low likelihood of endometrial cancer and thus do not need to undergo endometrial biopsy. -Transvaginal ultrasound can be used to evaluate the endometrial cavity and measure the thickness of the endometrial lining. If the endometrium measures less than 4 mm, then the client is at low risk for malignancy -Cancer can spread locally to other parts of the uterus or regionally to nearby lymph nodes. The regional lymph nodes are found in the pelvis and farther away along the aorta. Finally, the cancer can spread to distant lymph nodes or organs such as lung, liver, bone, brain, and others -Stages: -Stage I: the tumor has spread to the muscle wall of the uterus. -Stage II: it has spread to the cervix, but not outside the uterus. -Stage III: it has spread regionally to the bowel or vagina, with metastases to pelvic lymph nodes. -Stage IV: it has invaded the bladder mucosa, with distant metastases to the lungs, liver, and bone
question
Risk factors for Endometrial cancer
answer
Nulliparity • Obesity (more than 50 pounds overweight) • Liver disease • Infertility • Diabetes mellitus • Hypertension • History of pelvic radiation • Polycystic ovary syndrome • Early menarche (before 12 years old) • High-fat diet • Use of prolonged exogenous unopposed estrogen with an intact uterus • Endometrial hyperplasia • Family history of endometrial cancer • Personal history of hereditary nonpolyposis colon cancer • Personal history of breast, colon or ovarian cancer • History of uterine fibroids • Late onset of menopause (after age 52 years) • Tamoxifen use • Chronic anovulation
question
Therapeutic Management for Endometrial Cancer/Nursing Management
answer
-usually involves surgery with adjunct therapy based on pathologic findings. Surgery most often involves removal of the uterus (hysterectomy) and the fallopian tubes and ovaries (salpingo-oophorectomy). Removal of the fallopian tubes and ovaries is recommended because tumor cells spread early to the ovaries, and any dormant cancer cells could be stimulated to grow by ovarian estrogen. In more advanced cancers, radiation and chemotherapy are used as adjuncts to surgery. Routine surveillance intervals for follow-up care are typically every 3 to 4 months for the first 2 years, since 85% of recurrences occur in the first 3 years after diagnosis - Educate the client about preventive measures or follow-up care if she has been treated for cancer. Education may be the most important tool currently available for the early detection of endometrial cancer. Many risk factors for endometrial cancer are modifiable or treatable, including obesity, hypertension, and diabetes. Educating women about risk factors and ways to decrease the risks is essential so that women can learn about their own risk and can become partners in the fight against the number one gynecologic cancer
question
Cervical Cancer
answer
-Cancer of the uterine cervix -Second leading cause of cancer deaths among women world wide -Tends to occur in midlife -Most cases are found in women are younger than 50, rarely develops in women younger than 20 -Almost 20% of women with cervical cancer are diagnosed when they are over 65 years old. That is why it is important for older women to continue having regular Pap tests -More common in hispanic, african america and native american -Hispanic women have the highest rates of cervical cancer in the United States, and also have the highest rates of poverty, poor access to health care, and language and cultural barriers. Barriers to screening and prevention of cervical cancer include procrastination and fear of finding out they have cancer -Cervical cancer starts with abnormal changes in the cellular lining or surface of the cervix. Has been linked to HPV which is acquired through sexual activity. (most common STI); most are asymptomatic and don't even realize they have the virus -More than 90% of squamous cervical cancers contain HPV DNA, and the virus is now accepted as a major causative factor in the development of cervical cancer and its precursor, cervical dysplasia
question
Screening and Dx for Cervical Cancer
answer
-Screening for cervical cancer is very effective because the presence of a precursor lesion, cervical intraepithelial neoplasia (CIN), helps determine whether further tests are needed -Progression from low-grade to high-grade dysplasia takes an average of 9 years, and progression from high- grade dysplasia to invasive cancer takes up to 2 years. -Three main factors have been postulated to influence the progression of low-grade dysplasia to high-grade. These include the type and duration of viral infection,with high-risk HPV type and persistent infection predicting a higher risk for progression -Routine Pap smear testing for all sexually active women is the primary screening method for early detec- tion of cervical irregularities related to HPV and is crucial for the prevention of cervical cancer. Should start at the age of 21 -First Pap Age 21 -Until age 30: Yearly based on risk profile using glass slide method Every 2 years using liquid-based method -Ages 30-70 Every 2-3 years if last three Pap smears were normal -After age 70 May discontinue if: • Past three Pap smears were normal and no Pap smears in the past 10 years were abnormal -Colposcopy is a microscopic examination of the lower genital tract using a magnifying instrument called a colposcope
question
Risk Factors for Cervical Cancer
answer
• Early age at first intercourse (within 1 year of menarche) • Lower socioeconomic status • Promiscuous male partners • Unprotected sexual intercourse • Family history of cervical cancer (mother or sisters) • Sexual intercourse with uncircumcised men • Female offspring of mothers who took diethylstilbestrol (DES) • Infections with genital herpes or chronic chlamydia • Multiple sex partners • Cigarette smoking • Immunocompromised state • HIV infection • Oral contraceptive use • Moderate dysplasia on Pap smear within past 5 years • HPV infection
question
Treatment for Cervical Cancer
answer
• Cryotherapy—destroys abnormal cervical tissue by freezing with liquid nitrogen, Freon, or nitrous oxide. Healing takes up to 6 weeks, and the client may experience a profuse, watery vaginal discharge for 3 to 4 weeks • Cone biopsy or conization removes a cone-shaped section of cervical tissue. The base of the cone is formed by the ectocervix and the point or apex of the cone is from the endocervical canal. The cone biopsy is also a treatment and can be used to completely remove any precancers and very early cancers. Two methods are commonly used for cone biopsies: • LEEP (loop electrosurgical excision procedure) or LLETZ (large loop excision of the transfor- mation zone)—the abnormal cervical tissue is removed with a wire that is heated by an electrical current. For this procedure, a local anesthetic is used. It is performed in 10 minutes. Mild cramping and bleeding may persist for several weeks after the procedure. • Cold knife cone biopsy—a surgical scalpel or a laser is used instead of a heated wire to remove tissue. This procedure requires general anesthesia and is done in a hospital setting. After the procedure, cramping and bleeding may persist for a few weeks. • Laser therapy—destroys diseased cervical tissue by using a focused beam of high-energy light to vapor- ize it (burn it off). After the procedure, the woman may experience a watery brown discharge for a few weeks. Very effective in destroying precancers and preventing them from developing into cancers. • Hysterectomy—removes the uterus and cervix surgically • Radiation therapy—delivered by internal radium applications to the cervix or external radiation ther- apy that includes lymphatics of the pelvis • Chemoradiation—weekly cisplatin therapy con- current with radiation. Investigation of this therapy is ongoing
question
Nursing Management of Cervical Cancer
answer
-Gardasil and Cervarix are vaccines approved by the U.S. Food and Drug Administration to protect girls and women from HPV and thus prevent cervical cancer. The vaccines prevent infection from four HPV types: HPV 6, 11, 16, and 18. Theses types are responsible for 70% of cervical cancers and 90% of genital warts -The vaccine is administered by intramuscular injection, and the recom- mended schedule is a three-dose series with the second and third doses administered 2 and 6 months after the first dose. The recommended age for vaccination of females is 9 to 26 years old -Focus primary prevention education on the following: • Identify high-risk behaviors in clients and teach them how to reduce such behaviors: • Take steps to prevent STIs. • Avoid early sexual activity. • Faithfully use barrier methods of contraception. • Avoid smoking and drinking. • Receive the HPV vaccine. • Instruct women on the importance of screening for cervical cancer by having annual Pap smears
question
Vaginal Cancer
answer
-Malignant tissue growth arising in the vagina, vaginal cancers are rare. -Prognosis of vaginal cancer depends largely on the stage of disease and type of tumor. -Can be effectively treated, and when found early it is often curable -The etiology of vaginal cancer has not been identified. Malignant diseases of the vagina are either primary vaginal cancers or metastatic forms from adjacent or distant organs. About 80% of vaginal cancers are metastatic, primarily from the cervix and endometrium. -These cancers invade the vagina directly. Cancers from distant sites that metastasize to the vagina through the blood or lymphatic system are typically from the colon, kidneys, skin (melanoma), or breast. Tumors in the vagina commonly occur on the posterior wall and spread to the cervix or vulva
question
Therapeutic Management/Nursing Management for Vaginal Cancer
answer
-T/M: Treatment depends of type of cells involved and stage of the disease. If cancer is localized, radiation, laser surgery, or both may be used. If cancer has spread, radical surgery may be needed, such as a hysterectomy, or removal of the upper vagina with dissection of the pelvic nodes in addition to radiation therapy. -Direct risk factors for the initial development of vaginal cancer have not been identified, associated risk factors include advancing age (over 60 years old), previous pelvic radiation, exposure to DES in utero, vaginal trauma, history of genital warts (HPV infection), HIV infection, cervical cancer, chronic vaginal discharge, smoking, and low socioeconomic level -N/M: Nursing management for this cancer is similar to that for other reproductive cancers, with emphasis on sexuality counseling and referral to local support groups. Women undergoing radical surgery need intensive counseling about the nature of the surgery, risks, potential compli- cations, changes in physical appearance and physiologic function, and sexuality alterations.
question
Vulvar Cancer
answer
-Abnormal neoplastic growth on the external female genitalia. -Found most commonly in older women (mid 60's-mid 70's) -It is the fourth most common gy- necologic cancer, after endometrial, ovarian, and cervical cancers -Approximately 90% of vulvar tumors are squamous cell carcinomas. This type of cancer forms slowly over several years and is usually preceded by precancerous changes. These precancerous changes are termed vulvar intraepithelial neoplasia (VIN). The two major types of VIN are classic (undifferentiated) and simplex (differentiated). Classic VIN, the more common one, is associated with HPV infection -It typically occurs in women between 30 and 40 years old. In contrast to classic VIN, simplex VIN usually occurs in postmenopausal women and is not as- sociated with HPV
question
Screening and Dx for Vulvar Cancer
answer
-Annual vulvar examination is the most effective way to prevent vulvar cancer. Careful inspection of the vulva during routine annual gynecologic examinations remains the most productive diagnostic technique. Liberal use of biopsies of any suspicious vulvar lesion is usually necessary to make the diagnosis and to guide treatment. -However, many women do not seek health care evaluation for months or years after noticing an abnormal lump or lesion. -The diagnosis of vulvar cancer is made by a biopsy of the suspicious lesion, which is usually found on the labia majora.
question
Risk Factors for Vulvar Cancer
answer
-Exposure to HPV type 16 • Age over 50 years • HIV infection • VIN • Lichen sclerosus • Melanoma or atypical moles • Exposure to HSV type 2 • Multiple sex partners • Smoking • Herpes simplex • History of breast cancer • Immune suppression • Hypertension • Diabetes mellitus • Obesity
question
Therapeutic Management of Vulvar Cancers
answer
-T/M: In most cases, the woman reports persistent vulvar itching, burning, and edema that do not improve with the use of creams or ointments. A history of condyloma, gonorrhea, and herpes simplex are some of the factors for greater risk for VIN. -Diagnosis of vulvar carcinoma is often delayed. Women neglect to seek treatment for an average of 6 months from the onset of symptoms. In addition, a delay in diagnosis often occurs after the client presents to her physician. In many cases, a biopsy of the lesion is not performed until the problem fails to respond to numerous topical therapies. -During the physical examination, observe for any masses or thickening of the vulvar area. A vulvar lump or mass most often is noted. The vulvar lesion is usually raised and may be fleshy, ulcerated, leukoplakic, or warty. The cancer can appear anywhere on the vulva, although about three fourths arise primarily on the labia
question
Nursing Management of Vulvar Cancer
answer
-Women with vulvar cancer must clearly understand their disease, treatment options, and prognosis. To accomplish this, provide information and establish effective commu- nication with the client and her family. Act as an educator and advocate. -Teach the woman about healthy lifestyle behaviors, such as smoking cessation and measures to reduce risk factors. For example, instruct the woman how to examine her genital area, urging her to do so monthly between menstrual periods. -Tell her to look for any changes in appearance (whitened or reddened patches of skin); changes in feel (areas of the vulva becoming itchy or painful); or the development of lumps, moles (changes in size, shape, or color), freckles, cuts, or sores on the vulva. Urge the woman to report these changes to the health care provider -Teach the woman about preventive measures such as not wearing tight undergarments and not using perfumes and dyes in the vulvar region. Also educate her about the use of barrier methods of birth control (condoms) to reduce the risk of contracting HIV, HSV, and HPV.
question
Key Concepts
answer
-Women have a 1 in 3 lifetime risk of developing cancer, and one out of every four deaths is from cancer; thus, nurses must focus on screening and educating all women regardless of risk factors. -The nurse plays a key role in offering emotional support, determining appropriate sources of support, and helping the woman use effective coping strategies when facing a diagnosis of cancer of the reproductive tract. Although reproductive tract cancer is rare during pregnancy, the woman's vigilance and routine screenings should continue throughout. -A woman's sexuality and culture are inextricably interwoven, and it is essential that nurses working with women of various cultures recognize this and remain sensitive to the vast changes that will take place when the diagnosis of cancer is made. -Ovarian cancer is the eighth most common cancer among women and the fourth most common cause of cancer deaths for women in the United States, accounting for more deaths than any other cancer of the reproductive system. Ovarian cancer has been described as the "over- looked disease" or "silent killer" because women and health care practitioners often ignore or ratio- nalize early symptoms. It is typically diagnosed in advanced stages. -Unopposed endogenous and exogenous estrogens, obesity, nulliparity, menopause after the age of 52 years, and diabetes are the major etiologic risk factors associated with the development of endo- metrial cancer.
question
Key Concepts continued
answer
-The American Cancer Society recommends that women should be informed about risks and symptoms of endometrial cancer at the onset of menopause and strongly encouraged to report any unexpected bleeding or spotting to their health care providers. -Malignant diseases of the vagina are either primary vaginal cancers or metastatic forms from adjacent or distant organs. Vaginal cancer tumors can be ef- fectively treated and, when found early, are often curable. -Cervical cancer incidence and mortality rates have decreased noticeably in the past several decades, with most of the reduction attributed to the Pap test, which detects cervical cancer and precancerous lesions. -The nurse's role involves primary prevention of cervical cancer through education of women regarding risk factors and preventive vaccines to avoid cervical dysplasia. -Diagnosis of about 80% of vaginal cancers are metastatic, primarily from the cervix and endometrium. These cancers invade the vagina directly. Vulvar cancer is often delayed significantly because there is no single specific clinical symptom that heralds it. The most common presentation is persistent vulvar itching that does not improve with the application of creams or ointments.



