54: Endometrial Hyperplasia and Carcinoma – Flashcards
Unlock all answers in this set
Unlock answersquestion
What is the MC Gyn malignancy?
answer
Uterine Carcinoma (Endometrial Cancer)
question
What's the difference between Endometrial Carcinoma and Sarcoma of Uterus?
answer
Endometrial Carcinoma arises from the gland found in endometrium (97%) Sarcoma arises from mesenchymal uterine component. (3%)
question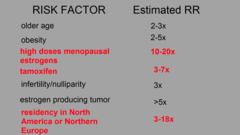
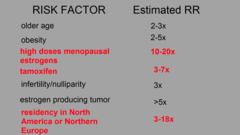
What is the etiology of Endometrial Carcinoma? ; what are its RF?
answer
Endometrial Hyperplasia RF: 1. Unopposed Estrogen (UE) --> Endometrial Proliferation (UE can come from endo or exogenous Estrogen 2. Age 3. Obesity: Adipose tisse contains Aromatase that converts Androstenedione to Estrone 4. Post-Menopausal Estrogen pills: Should only be given with ProG 5. Tamoxifen: SERM - Selective Estrogen Receptor Modulator 6. Granulosa Cell Tumor of Ovary: Secretes Estrogen 7. Nulliparity: No ProG 8. Early Menarche/Late Menopause: Increased duration of Endometrial exposure to Estrogen 9. Metabolic Syndrome: Diabetes, HTN, h/o Gall Bladder dz. 10. Lynch Syndrome
question
Most endometrial cancer are diagnosed in stage 1. T/F?Why?
answer
True B/c they are presented early and 90% will have symptomatic bleeding ; discharge.
question
Types of Endometrial Cancer?
answer
Type 1: Estrogen Dependent (90%) Type 2: NO epidemiology (10%) - High grade nuclei and clear cell histology
question
Postmenopausal pt w/ Vaginal bleeding. Diagnostic work-up?
answer
History --> PE --> Assessment of Endometrium, via Endometrial Sampling Pelvic Transvaginal US: for polyps, myomas, endometrial thickening (>5mm warrants further eval) --> Biopsy
question
What is the MC pattern of met spread?
answer
Direct extension to adjacent structure - myometrium, serosa, cervix, vagina, parametric, rectum, or bladder Less common: 1. Exfoliated cells can travel to tubes and implant on ovaries, parietal peritoneum or omentum 2. Lymphatic spread to Pelvic LN --> Para-aortic LN 3. Hematogenously to Liver or lung
question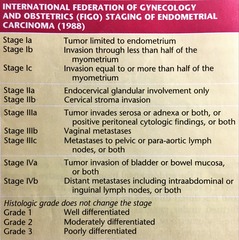
How is the staging and grading done for Endometrial Carcinoma
answer
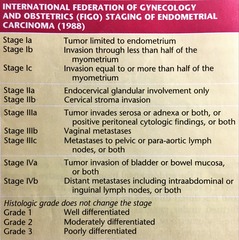
Stage 1: still in uterus: TAH/BSO Stage 2: Cervical involvement: TAH/BSO Stage 3: Adjacent structures/LN: Individualized Stage 4: Bladder +/- Bowel/ Mets: Individualized Histological Grading: Grade 1: Well differentiated Grade 2: Moderately differentiated Grade 3: Poorly Differentiated
question
A 57-year-old G0 postmenopausal woman presents to her gynecologist with a complaint of vaginal bleeding for one week. The patient reports the cessation of normal menses approximately four years ago. She has had no previous episodes of irregular bleeding except when she took hormonal replacement therapy for six months. She saw her nurse practitioner five months ago and reports having a normal gynecologic evaluation and a normal Pap smear. Her past medical history is significant for hypercholesterolemia and diet-controlled diabetes mellitus. Physical exam reveals a 5 feet 3 inches tall, 275-pound woman in no acute distress. Pelvic exam demonstrated a normal vulva, urethra, vagina and cervix. Bimanual exam was normal. An endometrial biopsy was obtained and demonstrated complex atypical hyperplasia. Which of the following is this patient's greatest risk factor for developing endometrial cancer? A. Nulliparity B. Obesity C. Postmenopausal status D. Use of hormone replacement therapy E. Complex atypical hyperplasia
answer
*E* Endometrial cancer is a gynecologic malignancy that has easily identifiable risk factors and typically presents with symptoms that lead to an early diagnosis. Risk factors include nulliparity, obesity, late menopause, hypertension and exposure to unopposed estrogens. Of these risk factors, obesity confers the greatest risk of developing endometrial carcinoma, especially when the patient is more than 50 pounds over ideal body weight (10-fold increase). However, in this case, the patient's greatest risk for developing an endometrial cancer is the presence of complex atypical hyperplasia (CAH) on endometrial biopsy. If left untreated, this process has approximately a 28% chance of progressing to an invasive cancer. More importantly, approximately 30% of women with a diagnosis of CAH will be found to have an invasive endometrial cancer on final pathology. Most women who develop endometrial cancer are postmenopausal, but this is less of an issue because of the finding of CAH.
question
Management of Endometrial AdenoCarcinoma?
answer
By Gyn-Onc: PE + CXR (MC met site) *Intra-Op:* Staging, TAH/BSO, w/ LN Dissection *Post-Op:* Adjuvant therapy - radiation (external pelvic/aortic, vaginal brachytherapy), chemo, Hormonal therapy *Nonsurgical:* High dose progestins and regular endometrial sampling (for nulliparous desiring future fertility)
question
A 69-year-old G3P3 comes in for a health maintenance examination. Her younger sister was recently diagnosed with endometrial cancer and she is concerned about her risk. Your patient experienced her last menstrual period at age 49, and she has not had any bleeding since. Her medications include only a multivitamin and supplemental calcium. She has no other significant family history. Her physical examination including a pelvic examination is normal. She is 5 feet 5 inches tall and weighs 120 pounds. What is the most appropriate management for this patient? A. Endometrial biopsy B. CA125 level C. Ultrasound with measurement of the endometrial lining D. Annual exams E. Refer to genetic counselor for risk assessment
answer
*D* Less than 5% of women diagnosed with endometrial cancer are asymptomatic. Approximately 80-90% of women with endometrial carcinoma present with vaginal bleeding or discharge as their only presenting symptom. Since this patient does not have any symptoms or risk factors for endometrial cancer, she does not need to have any diagnostic testing. Risk factors for endometrial cancer include late menopause, unopposed estrogen therapy, nulliparity, obesity, Tamoxifen therapy and diabetes mellitus. Although sometimes associated with Hereditary Non-polyposis Colorectal Cancer Syndrome (HNPCC, or Lynch II), endometrial cancer is typically not a genetically-inherited malignancy, and so genetic counseling for risk assessment would not be recommended unless a more significant family history existed. Endometrial cancer ranks as the fourth most common cancer detected in women in the US. In 2010, according to the American Cancer Society, there will be an estimated 43,470 new endometrial cancer cases. It is the most common gynecologic malignancy. Top Five Cancers Detected in Women: • Breast 28% • Lung 14% • Colon 10% • Uterine 6% • Ovary 3% Gynecologic Cancers: • Uterine 52% • Ovary 26% • Cervix 14% • Vulva 5% • Vagina 3%
question
A 72-year-old G3P3 presents to the emergency room complaining of abnormal vaginal discharge for the past two months. She has had two episodes of vaginal bleeding over the last year. She used combination hormone replacement therapy for 10 years when she went through menopause at age 58, but stopped once the Women's Health Initiative report came out. Her last gynecologic exam and Pap smear were two years ago and were normal. She has tried several over-the-counter antifungal creams for what she presumed was a yeast infection; however, she reports no change in the nature of the discharge. She does note that she has some mild lower abdominal discomfort. The only significant finding on exam is a mucopurulent discharge from a multiparous cervical os. She has a 10-week sized globular uterus. Which of the following findings is most concerning for presence of endometrial cancer? A. Vaginal bleeding B. Late menopause C. Abnormal vaginal discharge D. Enlarged uterus E. Hormone replacement therapy
answer
*A* Endometrial cancer is a disease that typically presents with symptoms and clinical findings that lead to an early diagnosis. The most common symptom is abnormal postmenopausal bleeding. However, other symptoms or clinical findings that may be seen include abnormal vaginal discharge and lower abdominal discomfort. Endometrial cancer can increase the size of the uterus as it grows, but is usually not the most common finding given the early diagnosis of this cancer. Unopposed estrogen replacement therapy does increase the risk, but not when taken in combination. Early menarche and late menopause are additional risk factors that may be related to endometrial cancer development.
question
A 65-year-old G2P1 woman has been referred to you for further evaluation of postmenopausal bleeding. She initially was seen by her internist after two weeks of intermittent vaginal spotting. She reports a similar episode approximately two months ago. A recent exam and Pap smear were normal. A transvaginal ultrasound showed a homogeneous endometrial lining measuring 5.0 mm. A subsequent office endometrial sample was obtained and returned with rare atypical cells. What is the most appropriate next step in the management of this patient? A. Repeat office endometrial sample B. Follow-up ultrasound in eight to twelve weeks C. Return visit in three to six months D. Abdominopelvic CT scan E. Dilation and curettage
answer
*E*
question
A 62-year-old G0 postmenopausal woman is being referred to your gynecologic oncology colleague after an office endometrial sample demonstrated a FIGO grade 1 endometrioid adenocarcinoma. The patient has no significant medical, surgical or other gynecologic history. She does not smoke and drinks only occasionally at social events. She takes a multivitamin. Her physical exam is unremarkable. Which of the following additional tests is indicated for this patient? A. Pelvic ultrasound B. Chest x-ray C. Pelvic MRI D. CA-125 E. Serum estrogen level
answer
*B* Once a pathologic diagnosis is confirmed by biopsy, a basic clinical assessment should ensue in all patients to help define the extent of the disease. If a careful history and clinical gynecologic exam suggests that the carcinoma is likely of an early stage, minimal pre-treatment evaluation is necessary. Routine evaluation in this setting should include a chest x-ray as the lungs are the most common site of distant spread. A pelvic ultrasound is not indicated once a pathologic diagnosis has been established, although one may have been obtained as part of the initial evaluation of postmenopausal bleeding. When there is a low suspicion for advanced disease, a CT scan, MRI, PET scan, and other invasive and costly tests are not indicated. A CA-125 may be helpful in predicting those patients that may have extrauterine spread, but is not absolutely necessary.
question
A 45-year-old G5P5 premenopausal woman was initially seen in your office for work-up and evaluation of a FIGO grade 3 endometrial cancer that was diagnosed by her gynecologist. Which of the following is the most appropriate treatment for this patient? A. Chemotherapy B. Radiation treatment C. Total abdominal hysterectomy, bilateral salpingo-oophorectomy, bilateral pelvic and para-aortic lymphadenectomy D. Supracervical abdominal hysterectomy with ovarian preservation E. Medroxprogesterone (Megace)
answer
*C* The recommended components of the surgical approach to an early endometrial cancer are the extrafascial total abdominal hysterectomy, bilateral salpingo-oophorectomy, and pelvic and para-aortic lymphadenectomy. Alternative surgical approaches to early endometrial cancer include a total vaginal hysterectomy with or without a bilateral salpingo-oophorectomy in women who are medically unstable or have contraindications to major abdominal surgery. Ideally, this approach would only be utilized in patients with well-differentiated endometrioid adenocarcinomas and avoided in patients with high-grade lesions or aggressive cell types, such as clear cell or papillary serous carcinomas. A total laparoscopic hysterectomy, BSO, with or without staging is being utilized more and more in lieu of the traditional open approach for select patients in many centers, and is a reasonable alternative. Although chemotherapy, radiation, and hormonal therapy may be utilized, it is usually in an adjuvant setting.
question
A 47-year-old G3P3 presents with a several month history of progressive abdominal bloating. She has had regular menses her entire life, but recently notes her bleeding to be heavier and occurring "twice a month." She is otherwise healthy and does not smoke or drink. On examination, she is 5 feet 5 inches tall and weighs 130 pounds. Her abdominal exam is notable for some mild distension, but no palpable masses. Her pelvic examination is notable for a normal appearing cervix, a deviated, but non-enlarged uterus, and a 10 cm mobile, non-tender right adnexal mass. An office endometrial biopsy reveals complex endometrial hyperplasia without atypia. What is the most likely explanation for the adnexal mass and the findings seen on the endometrial biopsy? A. Fibroid uterus B. Endometrioma C. Metastatic endometrial cancer D. Granulosa cell tumor E. Theca lutein cyst
answer
*D* The finding of an adnexal mass in a perimenopausal woman raises the suspicion of a neoplastic process. Because of the new onset of irregular bleeding and the finding of hyperplasia, the most likely explanation would be that of a granulosa cell tumor, an estrogen-secreting tumor. A theca lutein cyst is typically seen in the setting of pregnancy (molar pregnancy) and is often bilateral. A fibroid uterus may present with heavy irregular bleeding, but a pedunculated fibroid mimicking an adnexal mass is unlikely to present with such a bleeding pattern and has no correlation with hyperplasia. Severe endometriosis often presents with dysmenorrhea and is unlikely to develop in the perimenopause.
question
An 81-year-old G3P3 presents to your office with a history of light vaginal spotting. She states this has occurred recently and in association with a thin yellow discharge. She never experienced any vaginal bleeding since menopause at the age of 52, and denies ever having been on hormone replacement therapy. She is otherwise reasonably healthy, except for osteoporosis, well-controlled hypertension, and diabetes. She is physically active and still drives to all her appointments. She is no longer sexually active since the death of her husband two years ago. On examination, she is noted to have severe atrophic changes affecting her vulva and vagina. A small Pederson speculum allows for visualization of a normal multiparous cervix, and the bimanual examination is notable for a small, mobile uterus. Rectovaginal exam confirms no suspicious adnexal masses or nodularity. Which of the following is the most appropriate management for this patient? A. Pelvic transvaginal ultrasound B. Office endometrial biopsy C. Reassurance and observation for further bleeding D. Vaginal estrogen therapy E. Clindamycin vaginal cream
answer
*B* Postmenopausal bleeding or discharge accounts for the presenting symptom in 80-90% of women with endometrial cancer. However, the most common causes of postmenopausal bleeding are atrophy of the endometrium (60-80%), hormone replacement therapy (15-25%), endometrial cancer (10-15%), polyps (2-12%), and hyperplasia (5-10%). Any history of vaginal bleeding requires a thorough history, physical/pelvic examination, and assessment of the endometrium. This is ideally done via office endometrial sampling as part of the initial work-up. The use of pelvic transvaginal ultrasound can provide useful information as to the presence of any structural changes (polyps, myomas, endometrial thickening), and for which a diagnosis of endometrial cancer would be less likely if the endometrial thickness is < 5 mm. Although this patient is likely to have atrophy as the cause of her spotting, a thin endometrial stripe does not exclude the possibility of a non-estrogen dependent carcinoma of the atrophic endometrium. Vaginal estrogen or clindamycin are not indicated.
question
A 65-year-old G2P2 postmenopausal woman with a remote history of stage I, grade 1 endometrial cancer treated with surgery 15 years ago returns to your office for a health maintenance examination. During a review of systems, the patient reports several months of a dry cough, progressive dyspnea on exertion, and swelling in her legs. She is a non-smoker, but her now deceased husband smoked heavily. She saw her family physician, who initially treated her with a short course of antibiotics; however, because of persistent symptoms a chest x-ray was obtained and revealed a bilateral pleural effusion and a suspicious pulmonary nodule. Her examination is notable for decreased breath sounds at the lung bases, a normal abdominal exam, and a pelvic exam without any suspicious masses or nodularity. She has pitting edema in both of her lower extremities. What is the most appropriate next step in the management of this patient? A. Obtain a Doppler of her lower extremities B. Refer to oncologist C. Refer to palliative care D. Refer to pulmonologist E. Repeat chest x-ray in three months
answer
*D* Although recurrent endometrial cancer can present as multiple pulmonary nodules, this patient is unlikely to have a recurrence of her endometrial cancer given the initial early stage and remote timing of her cancer diagnosis. The most appropriate next step is to refer her to a pulmonologist (or cardiologist) for a thorough work-up. The finding of pleural effusions and lower extremity edema point towards a cardiopulmonary etiology; however, the finding of a solitary lung nodule in a patient exposed to second hand smoke certainly suggests the possibility of a primary lung cancer. Referral to palliative care would be premature at this point. A Doppler ultrasound to rule out a deep venous thrombosis is reasonable, but typically of more utility in the setting of unilateral edema, and still would not address the need to evaluate her lung findings
question
A 68-year-old woman with a history of breast cancer presents for evaluation of endometrial cancer risk. She was treated with lumpectomy and axillary node dissection and radiation therapy. She has been on tamoxifen therapy for the past year. She denies any vaginal bleeding or discharge. She is 5 feet 3 inches tall and weighs 140 pounds. Her pelvic examination is notable only for severe vulvovaginal atrophy. What is the next best step in the management of this patient? A. Endometrial biopsy now to obtain a baseline B. Annual endometrial biopsy C. Annual exams D. Annual pelvic ultrasound E. Endometrial biopsy upon completion of five years of tamoxifen therapy
answer
*C* Tamoxifen is known to increase the risk of endometrial cancer. However, *diagnostic studies, such as endometrial biopsy, are reserved for when the patient develops symptoms of bleeding or abnormal vaginal discharge.* Ultrasound is not helpful because Tamoxifen is known to cause changes to the endometrium, including thickening. Endometrial biopsy is not indicated as a screening tool for endometrial cancer.



